Abstract
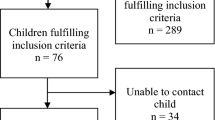
This study aimed to assess the balance function in children with sensorineural hearing loss (SNHL) using different tests to assess vestibulospinal pathway and tests to assess vestibular system and to compare the result obtained with those of children with normal hearing sensitivity. Detailed balance assessment was done for 15 children with severe to profound SNHL and 15 children with normal hearing sensitivity in the age range of 6–10 years. The audiological evaluation included pure-tone audiometry, speech audiometry, immittance evaluation, otoacoustic emission, vestibular evoked myogenic potential (cervical VEMP and ocular VEMP), and tests to assess vestibulospinal pathway and cerebellar function, such as Romberg test, Fukuda stepping test, Tandem gait test, and Finger-to-nose test. cVEMP and oVEMP were absent in 8 ears (27%) of a total of 30 ears with SNHL. Statistical analysis shows no significant difference between latency and amplitude of cVEMP peaks and latency of oVEMP peaks across groups. Significant reduction of oVEMP peaks amplitude was seen in children with SNHL compared to children with normal hearing. Fukuda stepping test showed an abnormal response in 2 children with SNHL (13%) and one child could not perform tandem gait test (7%). Children with SNHL showed an evident abnormality on the balance assessment test results. The abnormal function of the vestibular system and the vestibulospinal pathway can compromise the child’s motor development and thus needs investigation early in life.


Similar content being viewed by others
References
Herdman SJ (2007) Vestibular rehabilitation, 3rd edn. F. A. Davis Company, Philadelphia
Northern JL, Downs MP (2002) Hearing in children. Lippincott Williams & Wilkins, Philadelphia
Humphriss RL, Hall AJ (2011) Dizziness in 10 year old children: an epidemiological study. Int J Pediatr Otorhinolaryngol 75:395–400. https://doi.org/10.1016/J.IJPORL.2010.12.015
Li CM, Hoffman HJ, Ward BK et al (2016) Epidemiology of dizziness and balance problems in children in the United States: a population-based study. J Pediatr 171:240–247. https://doi.org/10.1016/j.jpeds.2015.12.002
Janky KL, Thomas MLA, High RR et al (2018) Predictive factors for vestibular loss in children with hearing loss. Am J Audiol 27:137–146. https://doi.org/10.1044/2017_AJA-17-0058
Zhou G, Kenna MA, Stevens K, Licameli G (2009) Assessment of saccular function in children with sensorineural hearing loss. Arch Otolaryngol Neck Surg 135:40–44. https://doi.org/10.1001/archoto.2008.508
Zhou G, Dargie J, Dornan B, Whittemore K (2014) Clinical uses of cervical vestibular-evoked myogenic potential testing in pediatric patients. Medicine 93:1–6. https://doi.org/10.1097/MD.0000000000000037
Singh S, Gupta RK, Kumar P (2012) Vestibular evoked myogenic potentials in children with sensorineural hearing loss. Int J Pediatr Otorhinolaryngol 76:1308–1311. https://doi.org/10.1016/J.IJPORL.2012.05.025
Selim E-AS, El-Minawi MS et al (2012) Assessment of saccular function using cervical vestibular-evoked myogenic potentials in children with sensorineural hearing loss. Egypt J Otolaryngol 28:234–241. https://doi.org/10.7123/01.EJO.0000418053.78780.0C
Isaradisaikul S, Navacharoen N, Hanprasertpong C, Kangsanarak J (2012) Cervical vestibular-evoked myogenic potentials: norms and protocols. Int J Otolaryngol 2012:913515. https://doi.org/10.1155/2012/913515
Welgampola MS, Carey JP (2010) Waiting for the evidence: VEMP testing and the ability to differentiate utricular versus saccular function. Otolaryngol Neck Surg 143:281–283. https://doi.org/10.1016/j.cortex.2009.08.003.Predictive
Singh NK, Sinha SK, Govindaswamy R, Apeksha K (2014) Are cervical vestibular evoked myogenic potentials sensitive to changes in the vestibular system associated with benign paroxysmal positional vertigo? Hear Balanc Commun 12:20–26. https://doi.org/10.3109/21695717.2014.883208
Singh NK, Sinha SK, Rajeshwari G et al (2015) Frequency-amplitude ratio of cervical vestibular evoked myogenic potential for iden tifying meniere’ s disease. Int J Heal Sci Res 5:228–237
Verbecque E, Marijnissen T, De Belder N et al (2017) Vestibular (dys)function in children with sensorineural hearing loss: a systematic review. Int J Audiol 56:361–381. https://doi.org/10.1080/14992027.2017.1281444
Singh NK, Apeksha K (2015) Efficacy of cervical and ocular vestibular-evoked myogenic potentials in evaluation of benign paroxysmal positional vertigo of posterior semicircular canal. Eur Arch Oto-Rhino-Laryngol 273:2523–2532. https://doi.org/10.1007/s00405-015-3867-3
Galan-Mercant A, Cuesta-Vargas AI (2014) Mobile Romberg test assessment (mRomberg). BMC Res Notes 7:640–647. https://doi.org/10.1186/1756-0500-7-640
Honaker JA, Boismier TE, Shepard NP, Shepard NT (2009) Fukuda stepping test: sensitivity and specificity. J Am Acad Audiol 20:311–314. https://doi.org/10.3766/jaaa.20.5.4
Margolesky J, Singer C (2018) How tandem gait stumbled into the neurological exam: a review. Neurol Sci 39:23–29. https://doi.org/10.1007/s10072-017-3108-1
Rumalla K, Karim A, Hullar T (2015) The effect of hearing aids on postural stability. Laryngoscope 125:720–723. https://doi.org/10.1002/lary.24974
Maes L, De Kegel A, Van Waelvelde H, Dhooge I (2014) Rotatory and collic vestibular evoked myogenic potential testing in normal-hearing and hearing-impaired children. Ear Hear 35:e21–e32. https://doi.org/10.1097/AUD.0b013e3182a6ca91
Said E-F (2014) Vestibular assessment in children with sensorineural hearing loss using both electronystagmography and vestibular-evoked myogenic potential. Egypt J Otolaryngol 30:43. https://doi.org/10.4103/1012-5574.127203
Inoue A, Iwasaki S, Ushio M et al (2013) Effect of vestibular dysfunction on the development of gross motor function in children with profound hearing loss. Audiol Neurotol 18:143–151. https://doi.org/10.1159/000346344
Acknowledgements
We would like to thank the Director and Principal, JSS Institute of Speech and Hearing, for allowing us to carry out this study. We would also like to thank all the participants of this study.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Apeksha, K., Singh, S., Rathnamala, M. et al. Balance Assessment of Children with Sensorineural Hearing Loss. Indian J Otolaryngol Head Neck Surg 73, 12–17 (2021). https://doi.org/10.1007/s12070-020-01797-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-01797-x