Abstract
Background
Decompressive hemicraniectomy improves survival rates and functional outcome in patients with space-occupying middle cerebral artery (MCA) infarction. We sought to determine clinical outcomes in elderly patients with MCA infarction treated with hemicraniectomy and to identify factors associated with functional outcome.
Methods
We performed a prospective, single-center observational study aiming to include patients aged ≥ 61 years with large MCA infarction treated with hemicraniectomy. The primary endpoint was the functional outcome according to modified Rankin Scale (mRS) score at 6 months after hemicraniectomy. Secondary endpoints included outcome measures at 12 months. A pooled analysis of individual patient data from the single-center cohort and a DESTINY 2 trial subgroup was performed to identify factors associated with functional status at 12 months.
Results
We included 40 MCA infarction patients who underwent hemicraniectomy between 2012 and 2017 at our university hospital (median [IQR] patient age 64 [62–67] years, National Institutes of Health Stroke Scale score 17 [16–21]). The dominant hemisphere was affected in 22/40 patients. Hemicraniectomy was performed within 31 [23–53] h of symptom onset. At 6 months after hemicraniectomy, 6/40 patients (15%) were moderately or moderately severely disabled (mRS score 3 or 4), 19 (47.5%) severely disabled (mRS score 5), and 15 (37.5%) had died. Compared to surgically treated DESTINY 2 patients, the single-center patients less likely exhibited favorable functional outcome at 6 months (mRS scores 0–4; odds ratio 0.239 [95% CI 0.082–0.696]). Case-fatality rate at 12 months was 43%. In a pooled analysis including 79 patients from DECAP and DESTINY 2, no significant associations of baseline and treatment factors with the clinical status at 12 months were observed.
Conclusions
In this single-center cohort of elderly patients with space-occupying MCA infarction and decompressive hemicraniectomy, the probability for survival without severe disability was low. Lethality at 6 and 12 months was comparable to previously reported data from a randomized trial.


Similar content being viewed by others
References
Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R. “Malignant” middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. 1996;53:309–15.
Heinsius T, Bogousslavsky J, Van Melle G. Large infarcts in the middle cerebral artery territory. Etiology and outcome patterns. Neurology. 1998;50:341–50.
Hofmeijer J, Algra A, Kappelle LJ, van der Worp HB. Predictors of life-threatening brain edema in middle cerebral artery infarction. Cerebrovasc Dis. 2008;25:176–84.
Thomalla G, Hartmann F, Juettler E, Singer OC, Lehnhardt F-G, Köhrmann M, et al. Prediction of malignant middle cerebral artery infarction by magnetic resonance imaging within 6 hours of symptom onset: a prospective multicenter observational study. Ann Neurol. 2010;68:435–45.
Scahill RI, Frost C, Jenkins R, Whitwell JL, Rossor MN, Fox NC. A longitudinal study of brain volume changes in normal aging using serial registered magnetic resonance imaging. Arch Neurol. 2003;60:989–94.
Huttner HB, Schwab S. Malignant middle cerebral artery infarction: clinical characteristics, treatment strategies, and future perspectives. Lancet Neurol. 2009;8:949–58.
Neugebauer H, Kollmar R, Niesen W-D, Bösel J, Schneider H, Hobohm C, et al. DEcompressive surgery Plus hypoTHermia for Space-Occupying Stroke (DEPTH-SOS): a protocol of a multicenter randomized controlled clinical trial and a literature review. Int J Stroke. 2013;8:383–7.
Schneider H, Krüger P, Algra A, Hofmeijer J, van der Worp HB, Jüttler E, et al. No benefits of hypothermia in patients treated with hemicraniectomy for large ischemic stroke. Int J Stroke. 2017;12:732–40.
Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol. 2007;6:215–22.
Hofmeijer J, Kappelle LJ, Algra A, Amelink GJ, van Gijn J, van der Worp HB, et al. Surgical decompression for space-occupying cerebral infarction (the Hemicraniectomy After Middle Cerebral Artery infarction with Life-threatening Edema Trial [HAMLET]): a multicentre, open, randomised trial. Lancet Neurol. 2009;8:326–33.
Jüttler E, Hacke W. Early decompressive hemicraniectomy in older patients with nondominant hemispheric infarction improves outcome. Stroke. 2011;42:843–4.
Jüttler E, Bösel J, Amiri H, Schiller P, Limprecht R, Hacke W, et al. DESTINY II: DEcompressive Surgery for the Treatment of malignant INfarction of the middle cerebral arterY II. Int J Stroke. 2011;6:79–86.
Jüttler E, Unterberg A, Woitzik J, Bösel J, Amiri H, Sakowitz OW, et al. Hemicraniectomy in older patients with extensive middle-cerebral-artery stroke. N Engl J Med. 2014;370:1091–100.
Puetz V, Campos CR, Eliasziw M, Hill MD, Demchuk AM. Calgary stroke program. Assessing the benefits of hemicraniectomy: what is a favourable outcome? Lancet Neurol. 2007;6:580.
Ropper AH. Hemicraniectomy-to halve or halve not. N Engl J Med. 2014;370:1159–60.
Alexander P, Heels-Ansdell D, Siemieniuk R, Bhatnagar N, Chang Y, Fei Y, et al. Hemicraniectomy versus medical treatment with large MCA infarct: a review and meta-analysis. BMJ Open. 2016;6:e014390.
van Middelaar T, Richard E, van der Worp HB, van den Munckhof P, Nieuwkerk PT, Visser MC, et al. Quality of life after surgical decompression for a space-occupying middle cerebral artery infarct: a cohort study. BMC Neurol. 2015;15:156.
Dasenbrock HH, Robertson FC, Aziz-Sultan MA, Guittieres D, Du R, Dunn IF, et al. Patient age and the outcomes after decompressive hemicraniectomy for stroke: a nationwide inpatient sample analysis. Neurocrit Care. 2016;25:371–83.
Saver JL, Filip B, Hamilton S, Yanes A, Craig S, Cho M, et al. Improving the reliability of stroke disability grading in clinical trials and clinical practice: the Rankin Focused Assessment (RFA). Stroke. 2010;41:992–5.
Gupta R, Connolly ES, Mayer S, Elkind MSV. Hemicraniectomy for massive middle cerebral artery territory infarction: a systematic review. Stroke. 2004;35:539–43.
Arac A, Blanchard V, Lee M, Steinberg GK. Assessment of outcome following decompressive craniectomy for malignant middle cerebral artery infarction in patients older than 60 years of age. Neurosurg Focus. 2009;26:E3.
Neugebauer H, Jüttler E. Hemicraniectomy for malignant middle cerebral artery infarction: current status and future directions. Int J Stroke. 2014;9:460–7.
Hofmeijer J, van der Worp HB, Kappelle LJ, Amelink GJ, Algra A, van Zandvoort MJE. Cognitive outcome of survivors of space-occupying hemispheric infarction. J Neurol. 2013;260:1396–403.
Zweckberger K, Juettler E, Bösel J, Unterberg WA. Surgical aspects of decompression craniectomy in malignant stroke: review. Cerebrovasc Dis. 2014;38:313–23.
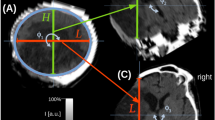
Neugebauer H, Fiss I, Pinczolits A, Hecht N, Witsch J, Dengler NF, et al. Large size hemicraniectomy reduces early herniation in malignant middle cerebral artery infarction. Cerebrovasc Dis. 2016;41:283–90.
Torbey MT, Bösel J, Rhoney DH, Rincon F, Staykov D, Amar AP, et al. Evidence-based guidelines for the management of large hemispheric infarction: a statement for health care professionals from the Neurocritical Care Society and the German Society for Neuro-intensive Care and Emergency Medicine. Neurocrit Care. 2015;22:146–64.
Dasenbrock HH, Robertson FC, Vaitkevicius H, Aziz-Sultan MA, Guttieres D, Dunn IF, et al. Timing of decompressive hemicraniectomy for stroke: a nationwide inpatient sample analysis. Stroke. 2017;48:704–11.
Ropper AH. Management of raised intracranial pressure and hyperosmolar therapy. Pract Neurol. 2014;14:152–8.
Schneider H, Hertel F, Kuhn M, Ragaller M, Gottschlich B, Trabitzsch A, et al. Decannulation and functional outcome after tracheostomy in patients with severe stroke (DECAST): a prospective observational study. Neurocrit Care. 2017;27:26–34.
Neugebauer H, Schneider H, Bösel J, Hobohm C, Poli S, Kollmar R, et al. Hypothermia in addition to decompressive surgery after malignant infarction. European Stroke J. 2017;2(Suppl 1):61.
Neugebauer H, Heuschmann PU, Jüttler E. DEcompressive Surgery for the Treatment of malignant INfarction of the middle cerebral arterY-Registry (DESTINY-R): design and protocols. BMC Neurol. 2012;12:115.
Acknowledgements
We thank the study patients and their relatives for their contribution to the study. The clinical study was conducted at the University Hospital, Technische Universität Dresden, Dresden, Germany. Statistical analyses were mainly performed at the Institute of Medical Biometry and Informatics, University of Heidelberg, Heidelberg, Germany.
Funding
None.
Author information
Authors and Affiliations
Contributions
JR has acquired, analyzed and interpreted data. SW has acquired and interpreted data. EJ has provided data and interpreted data. LU has analyzed and interpreted data. RL has analyzed and interpreted data. JB has acquired and interpreted data. GS has interpreted data and provided administrative support. HR has interpreted data and provided administrative support. HS has designed and coordinated the study, has acquired, analyzed and interpreted data, and drafted the manuscript. All authors critically revised the manuscript for important intellectual content. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interests.
Ethical Approval
The study was approved by the institutional review board (Ethikkommission an der TU Dresden; IRB00001473). Written informed consent was obtained from patients or their legal representatives.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rahmig, J., Wöpking, S., Jüttler, E. et al. Decompressive Hemicraniectomy in Elderly Patients With Space-Occupying Infarction (DECAP): A Prospective Observational Study. Neurocrit Care 31, 97–106 (2019). https://doi.org/10.1007/s12028-018-0660-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0660-3