Abstract
Introduction
This study was designed to identify factors related to delays in pre-hospital management of status epilepticus (SE).
Methods
This retrospective study includes all adult (>16 years of age) patients (N = 82) diagnosed with established SE in the Helsinki University Central Hospital emergency department (ED) over 2 years. SE was defined as a clinically observed episode fulfilling one of the following criteria: (1) continuous seizure lasting over 30 min; (2) recurring seizures without return of consciousness between seizures; (3) occurrence of more than four seizures within any 1 h. We collected 15 variables related to SE type, patient, and SE episode from the medical records, defined and calculated six pre-hospital delay parameters and analyzed their relations using univariate analysis and multivariate linear regression models.
Results
In the multivariate regression analysis, the focal SE was significantly associated with a long delay from SE onset to initial treatment (p < 0.05), to diagnosis (p < 0.002), and to anesthesia (p < 0.002). Administration of the initial treatment before emergency medical service arrived was significantly associated with long delay of the first alarm (p < 0.02) and arrival at the first ED (p < 0.04). Primary admission to a healthcare unit other than tertiary hospital caused a significant delay in diagnosis (p < 0.008) and anesthesia (p < 0.02). Surprisingly, univariate analysis revealed that if the SE onset occurred in a healthcare unit, the delays from SE onset to first alarm (p < 0.001), to arrival in first ED (p < 0.001), to arrival in tertiary hospital (p < 0.001), to diagnosis (p < 0.02), and to anesthesia (p < 0.01) were significantly longer than in cases in which SE onset occurred at a public place.
Conclusion
We found remarkable inadequacy in recognition of SE both among laity and medical professionals. There is an obvious need for increasing awareness of imminent SE and optimizing the pre-hospital management of established SE. SE should be considered as a medical emergency comparable with stroke and cardiac infarction and be allocated with similar resources in the pre-hospital management.

Similar content being viewed by others
References
Aminoff M, Simon R. Status epilepticus: causes, clinical features and consequences in 98 patients. Am J Med. 1980;69:657–66.
Towne AR, Pellock JM, Ko D, et al. Determinants of mortality in status epilepticus. Epilepsia. 1994;35(1):27–34.
DeLorenzo R, Hauser W, Towne A. A prospective, population-based epidemiologic study of status epilepticus in Richmond;Virginia. Neurology. 1996;46:1029–35.
Claassen J, Lokin JK, Fitzsimmons B-FM, et al. Predictors of functional disability and mortality after status epilepticus. Neurology. 2002;58:139–42.
Rossetti AO, Logroscino G, Bromfield EB. Refractory Status Epilepticus: effect of treatment aggressiveness on prognosis. Arch Neurol. 2005;62:1698–702.
Chin RFM, Neville BGR, Peckham C, et al. Treatment of community-onset, childhood convulsive status epilepticus: a prospective, population-based study. Lancet Neurol. 2008;7:696–703.
Neligan A, Shorvon SD. Prognostic factors, morbidity and mortality in tonic-clonic status epilepticus: a review. Epilepsy Res. 2011;93:1–10.
Meldrum BS, Horton RW. Physiology of status epilepticus in primates. Arch Neurol. 1973;28:1–9.
Lotham E. The biomechanical basis and pathophysiology of status epilepticus. Neurology. 1990;40:13–23.
Legriel S, Mouvillier B, Bele N, et al. Outcomes in 140 critically ill patients with status epilepticus. Intensive Care Med. 2008;34:476–80.
Naylor DE, Liu H, Wasterlain CG. Trafficking of GABA(A) receptors, loss of inhibition, and a mechanism for pharmacoresistance in status epilepticus. J Neurosci. 2005;25(34):7724–33.
Aranda A, Fuocart G, Ducasse J, et al. Generalized convulsive status epilepticus management in adults: a cohort study with evaluation of professional practice. Epilepsia. 2010;51:2159–67.
Alldredge BK, Gelb AM, Issacs SM, et al. A comparison of lorazepam, diazepam and placebo for the treatment of out-of-hospital status epilepticus. N Engl J Med. 2001;345:631–7.
Alldredge BK, Wall DB, Ferriero DM. Effect of prehospital treatment on the outcome of status epilepticus in children. Pediatr Neurol. 1995;12:213–6.
Pang T, Hirsch LJ. Treatment of convulsive and non-convulsive status epilepticus. Curr Treat Opinions Neurol. 2005;7(4):247–59.
Silbergleit R, Durkalski V, Lowenstein D, et al. Intramuscular versus intravenous therapy for prehospital status epilepticus. N Engl J Med. 2012;366(7):591–600.
Dreifuss FE, Rosman NP, Cloyd JC, et al. A comparison of rectal diazepam gel and placebo for acute repetitive seizures. N Engl J Med. 1998;338(26):1869–75.
Scott RC, Besag FMC, Neville BRG. Buccal midazolam and rectal diazepam for treatment of prolonged seizures in childhood and adolescence: a randomized trial. Lancet. 1999;353:623–6.
Bazil C. Treatment of out-of-hospital status epilepticus. Epilepsy Curr. 2002;2(1):13–4.
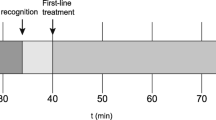
Kämppi L, Mustonen H, Soinila S. Analysis of the delay components in the treatment of status epilepticus. Neurocrit Care. 2013;19:10–8.
Park YH, Kang GH, Song BG, et al. Factors related to prehospital time delay in acute ST-segment elevation myocardial infarction. J Korean Med Sci. 2012;27(8):864–9.
Faiz KW, Sundseth A, Thommessen B, et al. Prehospital delay in acute stroke and TIA. Emerg Med J. 2013;30(8):669–74.
Fassbender K, Balucani C, Walter S, et al. Streamlining of prehospital stroke management: the golden hour. Lancet Neurol. 2013;12:585–96.
Faiz KW, Sundseth A, Thommessen B, et al. Factors related to decision delay in acute stroke. J Stroke Cerebrovasc Dis. 2014;23:534–9.
Puolakka T, Väyrynen T, Häppölä O, et al. Sequential analysis of pretreatment delays in stroke thrombolysis. Acad Emerg Med. 2010;17(9):965–9.
Zanini R, Aroldi M, Bonatti S, et al. Impact of prehospital diagnosis in the management of ST elevation myocardial infarction in the era of primary percutaneous coronary intervention: reduction of treatment delay and mortality. J Cardiovasc Med (Hagerstown). 2008;9(6):570–5.
Sejersten M, Sillesen M, Hansen PR, et al. Effect on treatment delay of prehospital teletransmission of 12-lead electrocardiogram to a cardiologist for immediate triage and direct referral of patients with ST-segment elevation acute myocardial infarction to primary percutaneous coronary intervention. Am J Cardiol. 2008;101(7):941–6.
Meierkord H, Boon P, Engelsen B, et al. EFNS guidelines for the treatment of status epilepticus in adults. Eur J Neurol. 2010;17(3):348–55.
Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23.
Cereghino JJ. Identification and treatment of acute repetitive seizures in children and adults. Curr Treat Options Neurol. 2007;9(4):249–55.
Power K, Flatten H, Gilhus N, et al. Propofol treatment in adult refractory status epilepticus. Mortality risk and outcome. Epilepsy Res. 2011;9:53–60.
Michael G, O’Connor R. The diagnosis and management of seizures and status epilepticus in the prehospital setting. Emerg Med Clin N Am. 2011;29(1):29–39.
Pellock JM, Marmarou A, DeLorenzo R. Time to treatment in prolonged seizure episodes. Epilepsy Behav. 2004;5:192–6.
Hillman J, Lehtimäki K, Peltola J, et al. Clinical significance of treatment delay in status epilepticus. Int J of Emerg Med. 2013;6:6.
Xian Y, Holloway RG, Chan PS, et al. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA. 2011;305(4):373–80.
Ziai WC, Schlattman D, Llinas R, et al. Emergent EEG in the emergency department in patients with altered mental states. J Clin Neurophysiol. 2012;123(5):910–7.
Karakis I, Montouris GD, Otis JA, et al. A quick and reliable EEG montage for the detection of seizures in the critical care setting. J Clin Neurophysiol. 2010;27(2):100–5.
Acknowledgments
This study has been financially supported by Epilepsy Research Foundation in Finland to LK. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Conflict of interest
No author of this paper has any conflict of interest to disclose
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
12028_2014_16_MOESM2_ESM.xls
Online Table 2 The complete univariate analysis of the factors related to pre-hospital delays in the management of SE (XLS 60 kb)
Rights and permissions
About this article
Cite this article
Kämppi, L., Mustonen, H. & Soinila, S. Factors Related to Delays in Pre-hospital Management of Status Epilepticus. Neurocrit Care 22, 93–104 (2015). https://doi.org/10.1007/s12028-014-0016-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-014-0016-6