Abstract
Purpose of Review
Non-adherence to medications for the secondary prevention of myocardial infarction (MI) is a major contributor to morbidity and mortality in these patients. This review describes recent advances in promoting adherence to therapies for coronary artery disease (CAD).
Recent Findings
Two large randomized controlled trials to “incentivize” adherence were somewhat disappointing; neither financial incentives nor “peer pressure” successfully increased rates of adherence in the post-MI population. Patient education and provider engagement appear to be critical aspects of improving adherence to CAD therapies, where the provider is a physician, pharmacist, or nurse and follow-up is performed in person or by telephone. Fixed-dose combinations of CAD medications, formulated as a so-called “polypill,” have shown some early efficacy in increasing adherence. Technological advances that automate monitoring and/or encouragement of adherence are promising but seem universally dependent on patient engagement. For example, medication reminders via text message perform better if patients are required to respond. Multifaceted interventions, in which these and other interventions are combined together, appear to be most effective.
Summary
There are several available types of proven interventions through which providers, and the health system at large, can advance patient adherence to CAD therapies. No single intervention to promote adherence will be successful in all patients. Further study of multifaceted interventions and the interactions between different interventions will be important to advancing the field. The goal is a learning healthcare system in which a network of interventions responds and adapts to patients’ needs over time.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fihn SD, Blankenship JC, Alexander KP, Bittl JA, Byrne JG, Fletcher BJ, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014;64(18):1929–49.
Eikelboom JW, Connolly SJ, Bosch J, Dagenais GR, Hart RG, Shestakovska O, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377(14):1319–30. https://doi.org/10.1056/NEJMoa1709118.
Sattar N, Petrie MC, Zinman B, Januzzi JL Jr. Novel diabetes drugs and the cardiovascular specialist. J Am Coll Cardiol. 2017;69(21):2646–56. https://doi.org/10.1016/j.jacc.2017.04.014.
Lloyd-Jones DM, Morris PB, Ballantyne CM, Birtcher KK, Daly DD Jr, DePalma SM, et al. 2017 focused update of the 2016 ACC expert consensus decision pathway on the role of non-statin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk. J Am Coll Cardiol. 2017;70(14):1785–822. https://doi.org/10.1016/j.jacc.2017.07.745.
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377(12):1119–31. https://doi.org/10.1056/NEJMoa1707914.
Ho PM, Spertus JA, Masoudi FA, Reid KJ, Peterson ED, Magid DJ, et al. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med. 2006;166(17):1842–7. https://doi.org/10.1001/archinte.166.17.1842.
• Bansilal S, Castellano JM, Garrido E, Wei HG, Freeman A, Spettell C, et al. Assessing the impact of medication adherence on long-term cardiovascular outcomes. J Am Coll Cardiol. 2016;68(8):789–801. Demonstrates increased costs as well as worse outcomes among non-adherent patients and establishes that a minimum of 40% adherence is necessary to gain significant benefit from medical therapy for CAD.
Bissonnette JM. Adherence: a concept analysis. J Adv Nurs. 2008;63(6):634–43. https://doi.org/10.1111/j.1365-2648.2008.04745.x.
•• Sabaté E, World Health Organization. Adherence to long-term therapies. World Health Organization; 2003. 1 p. Establishes the domains of non-adherence used to categorize research interventions to improve adherence.
Arnet I, Kooij MJ, Messerli M, Hersberger KE, Heerdink ER, Bouvy M. Proposal of standardization to assess adherence with medication records. Ann Pharmacother. 2016;50(5):360–8. https://doi.org/10.1177/1060028016634106.
Kriegbaum M, Liisberg KB, Wallach-Kildemoes H. Pattern of statin use changes following media coverage of its side effects. Patient Preference and Adherence Dove Press. 2017;11:1151–7. https://doi.org/10.2147/PPA.S133168.
Wallert J, Lissåker C, Madison G, Held C, Olsson E. Young adulthood cognitive ability predicts statin adherence in middle-aged men after first myocardial infarction: a Swedish National Registry study. Eur J Prev Cardiol. 2017;24(6):639–46. https://doi.org/10.1177/2047487317693951.
Schedlbauer A, Schroeder K, Peters TJ, Fahey T. Interventions to improve adherence to lipid lowering medication. Cochrane Database Syst Rev. 2004;80(4):CD004371.
Zhao S, Zhao H, Wang L, Du S, Qin Y. Education is critical for medication adherence in patients with coronary heart disease. Acta Cardiol. 2017;70(2):197–204.
Meng K, Seekatz B, Haug G, Mosler G, Schwaab B, Worringen U, et al. Evaluation of a standardized patient education program for inpatient cardiac rehabilitation: impact on illness knowledge and self-management behaviors up to 1 year. Health Educ Res. 2014;29(2):235–46. https://doi.org/10.1093/her/cyt107.
Keyserling TC, Sheridan SL, Draeger LB, Finkelstein EA, Gizlice Z, Kruger E, et al. A comparison of live counseling with a web-based lifestyle and medication intervention to reduce coronary risk: a randomized clinical trial. JAMA Intern Med. 2014;174(7):1144–57. https://doi.org/10.1001/jamainternmed.2014.1984.
Nord JW, Berry A, Stults B, Burningham Z, Beddhu S, Sauer BC. Evaluation of the effectiveness of a patient centered educational mailer designed to improve statin adherence: a pragmatic trial. eGEMs. 2017;4(1):30. https://doi.org/10.13063/2327-9214.1256.
Schwalm J-D, Ivers NM, Natarajan MK, Taljaard M, Rao-Melacini P, Witteman HO, et al. Cluster randomized controlled trial of delayed educational reminders for long-term medication adherence in ST-elevation myocardial infarction (DERLA-STEMI). Am Heart J. 2015;170(5):903–13. https://doi.org/10.1016/j.ahj.2015.08.014.
Richards SH, Anderson L, Jenkinson CE, Whalley B, Rees K, Davies P, et al. Psychological interventions for coronary heart disease. Cochrane Database Syst Rev. 2017;4:CD002902.
•• Ho PM, Lambert-Kerzner A, Carey EP, Fahdi IE, Bryson CL, Melnyk SD, et al. Multifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomized clinical trial. JAMA Intern Med. 2014;174(2):186–93. Trial that engaged providers, pharmacists, and patients using multiple interventions to significantly improve medication adherence.
Unni EJ, Farris KB. Unintentional non-adherence and belief in medicines in older adults. Patient Educ Couns. 2011 May;83(2):265–8. https://doi.org/10.1016/j.pec.2010.05.006.
Gadkari AS, McHorney CA. Unintentional non-adherence to chronic prescription medications: how unintentional is it really? BMC Health Serv Res. 2012;12(1):44.
Isaacs SL, Schroeder SA. Class—the ignored determinant of the Nation’s health. N Engl J Med. 2004;351(11):1137–42. https://doi.org/10.1056/NEJMsb040329.
• Doll JA, Hellkamp AS, Goyal A, Sutton NR, Peterson ED, Wang TY. Treatment, outcomes, and adherence to medication regimens among dual Medicare-Medicaid–eligible adults with myocardial infarction. JAMA Cardiol. 2016;1(7):787–94. Reveals the complexity of adherence relationships by showing that superior medication adherence does not guarantee better outcomes.
Clark AM, Des Meules M, Luo W, Duncan AS, Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009;6(11):712–22. https://doi.org/10.1038/nrcardio.2009.163.
Gaalema DE, Elliott RJ, Morford ZH, Higgins ST, Ades PA. Effect of socioeconomic status on propensity to change risk behaviors following myocardial infarction: implications for healthy lifestyle medicine. Prog Cardiovasc Dis. 2017;60(1):159–68. https://doi.org/10.1016/j.pcad.2017.01.001.
Yuan C, Wei C, Wang J, Qian H, Ye X, Liu Y, et al. Self-efficacy difference among patients with cancer with different socioeconomic status: application of latent class analysis and standardization and decomposition analysis. Cancer Epidemiol. 2014;38(3):298–306. https://doi.org/10.1016/j.canep.2014.02.012.
Kripalani S, Schmotzer B, Jacobson TA. Improving medication adherence through graphically enhanced interventions in coronary heart disease (IMAGE-CHD): a randomized controlled trial. J Gen Intern Med. 2012;27(12):1609–17. https://doi.org/10.1007/s11606-012-2136-z.
•• Reese PP, Kessler JB, Doshi JA, Friedman J, Mussell AS, Carney C, et al. Two randomized controlled pilot trials of social forces to improve statin adherence among patients with diabetes. J Gen Intern Med. 2015;31(4):402–10. Randomized trial in which two types of “social forces” (i.e., peer pressure) failed to improve medication adherence.
Kripalani S, Henderson LE, Jacobson TA, Vaccarino V. Medication use among inner-city patients after hospital discharge: patient-reported barriers and solutions. Mayo Clin Proc. 2008;83(5):529–35. https://doi.org/10.1016/S0025-6196(11)60724-6.
Dhaliwal KK, King-Shier K, Manns BJ, Hemmelgarn BR, Stone JA, Campbell DJT. Exploring the impact of financial barriers on secondary prevention of heart disease. BMC Cardiovasc Disord. 2017;17(1):2686.
Luiza VL, Chaves LA, Silva RM, Emmerick ICM, Chaves GC, Fonseca de Araújo SC, et al. Pharmaceutical policies: effects of cap and co-payment on rational use of medicines. Cochrane Database Syst Rev. 2015;79(5):CD007017.
Tajeu GS, Kent ST, Kronish IM, Huang L, Krousel-Wood M, Bress AP, et al. Trends in antihypertensive medication discontinuation and low adherence among Medicare beneficiaries initiating treatment from 2007 to 2012. Hypertension. 2016;68(3):565–75. https://doi.org/10.1161/HYPERTENSIONAHA.116.07720.
Colantonio LD, Huang L, Monda KL, Bittner V, Serban M-C, Taylor B, et al. Adherence to high-intensity statins following a myocardial infarction hospitalization among Medicare beneficiaries JAMA Cardiol. 2017.
Choudhry NK, Avorn J, Glynn RJ, Antman EM, Schneeweiss S, Toscano M, et al. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365(22):2088–97. https://doi.org/10.1056/NEJMsa1107913.
•• Volpp KG, Troxel AB, Mehta SJ, Norton L, Zhu J, Lim R, et al. Effect of electronic reminders, financial incentives, and social support on outcomes after myocardial infarction: the Heart Strong Randomized Clinical Trial. JAMA Intern Med. 2017;177(8):1093–101. A large randomized controlled trial from a thought leader in behavioral economics of medication adherence, unfortunately no benefit to multifaceted intervention leveraging financial incentives.
• Patel MS, Asch DA, Rosin R, Small DS, Bellamy SL, Heuer J, et al. Framing financial incentives to increase physical activity among overweight and obese adults: a randomized, controlled trial. Ann Intern Med. 2016;164(6):385–94. Suggests the aforementioned trial by Volpp et al. may have been positive if the financial incentive had been framed as a loss, i.e., if you give patients money at the beginning of the trial then “fine” them if they are non-adherent.
Doll JA, Wang TY, Choudhry NK, Cannon CP, Cohen DJ, Fonarow GC, et al. Rationale and design of the Affordability and Real-world Antiplatelet Treatment Effectiveness after Myocardial Infarction Study (ARTEMIS): a multicenter, cluster-randomized trial of P2Y12 receptor inhibitor copayment reduction after myocardial infarction. Am Heart J. 2016;177:33–41. https://doi.org/10.1016/j.ahj.2016.04.008.
Calvert SB, Kramer JM, Anstrom KJ, Kaltenbach LA, Stafford JA, Allen LaPointe NM. Patient-focused intervention to improve long-term adherence to evidence-based medications: a randomized trial. Am Heart J. 2012;163(4):657–665.e1.
van Driel ML, Morledge MD, Ulep R, Shaffer JP, Davies P, Deichmann R. Interventions to improve adherence to lipid-lowering medication. Cochrane Database Syst Rev. 2016;12:CD004371.
Jia J-J, Dong P-S, Du L-J, Li Z-G, Lai L-H, Yang X-M, et al. Impact of physician-coordinated intensive follow-up on long-term medical costs in patients with unstable angina undergoing percutaneous coronary intervention. Acta Cardiol Sin. 2017;33(2):173–81.
• Faridi KF, Peterson ED, McCoy LA, Thomas L, Enriquez J, Wang TY. Timing of first postdischarge follow-up and medication adherence after acute myocardial infarction. JAMA Card. 2016;1(2):147–55. Nice retrospective analysis demonstrating better adherence among patients who followed up with a clinician within 6 weeks of discharge after MI.
Cai H, Dai H, Hu Y, Yan X, Xu H. Pharmacist care and the management of coronary heart disease: a systematic review of randomized controlled trials. BMC Health Serv Res. 2013;13(1):461. https://doi.org/10.1186/1472-6963-13-461.
Peersen K, Munkhaugen J, Gullestad L, Liodden T, Moum T, Dammen T, et al. The role of cardiac rehabilitation in secondary prevention after coronary events. Eur J Prev Cardiol. 2017;24(13):1360–8. https://doi.org/10.1177/2047487317719355.
Lewin S, Munabi-Babigumira S, Glenton C, Daniels K, Bosch-Capblanch X, van Wyk BE, et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev. 2010;94(3):CD004015.
• Xavier D, Gupta R, Kamath D, Sigamani A, Devereaux PJ, George N, et al. Community health worker-based intervention for adherence to drugs and lifestyle change after acute coronary syndrome: a multicentre, open, randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4(3):244–53. Showed that using lay health workers to engage patients improved adherence to medications as well as healthy lifestyle among post-MI patients in India.
Jakobsson S, Irewall A-L, Bjorklund F, Mooe T. Cardiovascular secondary prevention in high-risk patients: a randomized controlled trial sub-study. BMC Cardiovasc Disord. 2015;15(1):1752.
Rinfret S, Rodés-Cabau J, Bagur R, Déry J-P, Dorais M, Larose E, et al. Telephone contact to improve adherence to dual antiplatelet therapy after drug-eluting stent implantation. Heart. 2013;99(8):562–9. https://doi.org/10.1136/heartjnl-2012-303004.
Crutchfield TM, Kistler CE. Getting patients in the door: medical appointment reminder preferences. Patient Preference Adherence. 2017;11:141–50. https://doi.org/10.2147/PPA.S117396.
Adler AJ, Martin N, Mariani J, Tajer CD, Owolabi OO, Free C, et al. Mobile phone text messaging to improve medication adherence in secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2017;4:CD011851.
Park LG, Howie-Esquivel J, Chung ML, Dracup K. A text messaging intervention to promote medication adherence for patients with coronary heart disease: a randomized controlled trial. Patient Educ Couns. 2014;94(2):261–8. https://doi.org/10.1016/j.pec.2013.10.027.
• Wald DS, Butt S, Bestwick JP. One-way versus two-way text messaging on improving medication adherence: meta-analysis of randomized trials. Am J Med. 2015;128(10):1139.e1–5. Meta-analysis showing superiority of two-way text messaging, i.e., requiring a response from patients, in promoting adherence.
Pfaeffli Dale L, Dobson R, Whittaker R, Maddison R. The effectiveness of mobile-health behaviour change interventions for cardiovascular disease self-management: a systematic review. Eur J Prev Cardiol. 2016;23(8):801–17. https://doi.org/10.1177/2047487315613462.
Devi R, Singh SJ, Powell J, Fulton EA, Igbinedion E, Rees K. Internet-based interventions for the secondary prevention of coronary heart disease. Cochrane Database Syst Rev. 2015;12:CD009386.
Desteghe L, Kluts K, Vijgen J, Koopman P, Dilling-Boer D, Schurmans J, et al. The health buddies app as a novel tool to improve adherence and knowledge in atrial fibrillation patients: a pilot study. JMIR mHealth uHealth. 2017;5(7):e98. https://doi.org/10.2196/mhealth.7420.
Kociánová E, Václavík J, Tomková J, Ondra P, Jarkovský J, Benešová K, et al. Heart rate is a useful marker of adherence to beta-blocker treatment in hypertension. Blood Press. 2017;26(5):311–8. https://doi.org/10.1080/08037051.2017.1346458.
Rui Wang, Sitova Z, Xiaoqing Jia, Xiang He, Abramson T, Gasti P, et al. Automatic identification of solid-phase medication intake using wireless wearable accelerometers. IEEE 4168–71.
Kalantarian H, Motamed B, Alshurafa N, Sarrafzadeh M. A wearable sensor system for medication adherence prediction. Artif Intell Med. 2016;69:43–52. https://doi.org/10.1016/j.artmed.2016.03.004.
• Frias J, Virdi N, Raja P, Kim Y, Savage G, Osterberg L. Effectiveness of digital medicines to improve clinical outcomes in patients with uncontrolled hypertension and type 2 diabetes: prospective, open-label, cluster-randomized pilot clinical trial. J Med Internet Res. 2017;19(7):e246. A unique digital medicine offering (DMO) in which digital medicines (medication taken with ingestible sensor), wearable sensor patches, and a mobile device app improved medication adherence and clinical targets for blood pressure, diabetes, and cholesterol control.
Patel MS, Asch DA, Volpp KG. Wearable devices as facilitators, not drivers, of health behavior change. JAMA. 2015;313(5):459–60. https://doi.org/10.1001/jama.2014.14781.
Fontana M, Asaria P, Moraldo M, Finegold J, Hassanally K, Manisty CH, et al. Patient-accessible tool for shared decision making in cardiovascular primary prevention: balancing longevity benefits against medication disutility. Circulation. 2014; 129(24):CIRCULATIONAHA.113.007595–2546.
George J, Elliott RA, Stewart DC. A systematic review of interventions to improve medication taking in elderly patients prescribed multiple medications. Drugs Aging. 2008;25(4):307–24. https://doi.org/10.2165/00002512-200825040-00004.
• Ivers N, Schwalm JD, Witteman HO, Presseau J, Taljaard M, McCready T, et al. Interventions Supporting Long-term Adherence aNd Decreasing cardiovascular events (ISLAND): pragmatic randomized trial protocol. Am Heart J. 2017;190:64–75. Important forthcoming trial studying mailings alone for promoting adherence in comparison with mailings plus engagement by lay health workers if non-adherence is detected via an automated telephone call.
Serban M-C, Colantonio LD, Manthripragada AD, Monda KL, Bittner VA, Banach M, et al. Statin intolerance and risk of coronary heart events and all-cause mortality following myocardial infarction. J Am Coll Cardiol. 2017;69(11):1386–95. https://doi.org/10.1016/j.jacc.2016.12.036.
Booth JN, Colantonio LD, Chen L, Rosenson RS, Monda KL, Safford MM, et al. Statin discontinuation, reinitiation, and persistence patterns among Medicare beneficiaries after myocardial infarction: a cohort study. Circ Cardiovasc Qual Outcomes. 2017;10(10):e003626.
Bahiru E, de Cates AN, Farr MR, Jarvis MC, Palla M, Rees K, et al. Fixed-dose combination therapy for the prevention of atherosclerotic cardiovascular diseases. Cochrane Database Syst Rev. 2017;3:CD009868.
Patel A, Cass A, Peiris D, Usherwood T, Brown A, Jan S, et al. A pragmatic randomized trial of a polypill-based strategy to improve use of indicated preventive treatments in people at high cardiovascular disease risk. Eur J Prev Cardiolog. 2014;22(7):920–30.
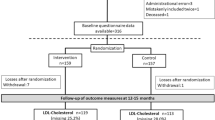
• Castellano JM, Sanz G, Peñalvo JL, Bansilal S, Fernández-Ortiz A, Alvarez L, et al. A Polypill strategy to improve adherence: results from the FOCUS project. J Am Coll Cardiol. 2014;64(20):2071–82. An important study in which phase 1 consisted of a cohort study to understand risk factors for non-adherence and phase 2 randomized approximately 700 patients to receive usual care or a fixed dose combination “polypill” formulated with 3 CAD therapies (“polypill”). The “polypill” group had higher rates of adherence.
Castellano JM, Bueno H, Fuster V. The cardiovascular polypill: clinical data and ongoing studies. Int J Cardiol Elsevier. 2015;201:S8–S14. https://doi.org/10.1016/S0167-5273(15)31027-5.
Shore S, Jones PG, Maddox TM, Bradley SM, Stolker JM, Arnold SV. Longitudinal persistence with secondary prevention therapies relative to patient risk after myocardial infarction. Heart. 2015;101(10):800–7. https://doi.org/10.1136/heartjnl-2014-306754.
Barefoot JC, Helms MJ, Mark DB, Blumenthal JA, Califf RM, Haney TL, et al. Depression and long-term mortality risk in patients with coronary artery disease. Am J Cardiol. 1996;78(6):613–7. https://doi.org/10.1016/S0002-9149(96)00380-3.
Mathews R, Wang TY, Honeycutt E, Henry TD, Zettler M, Chang M, et al. Persistence with secondary prevention medications after acute myocardial infarction: insights from the TRANSLATE-ACS study. Am Heart J. 2015;170(1):62–9. https://doi.org/10.1016/j.ahj.2015.03.019.
Smolderen KG, Buchanan DM, Gosch K, Whooley M, Chan PS, Vaccarino V, et al. Depression treatment and 1-year mortality after acute myocardial infarction clinical perspective: insights from the TRIUMPH registry (Translational Research Investigating Underlying disparities in acute Myocardial infarction Patients’ Health Status). Circulation. 2017;135(18):1681–9. https://doi.org/10.1161/CIRCULATIONAHA.116.025140.
Jørstad HT, Minneboo M, Helmes HJM, Fagel ND, Scholte op Reimer WJ, JGP T, et al. Effects of a nurse-coordinated prevention programme on health-related quality of life and depression in patients with an acute coronary syndrome: results from the RESPONSE randomised controlled trial. BMC Cardiovasc Disord. BioL Med Central. 2016;16(1):2458.
• Committee on the Learning Health Care System in America, Institute of Medicine (IOM), Smith M, Saunders R, Stuckhardt L, JM MG. Best care at lower cost: the path to continuously learning health care in America. Washington (DC): National Academies Press (US); 2013. Clairvoyant position paper outline the path towards a learning healthcare system.
Author information
Authors and Affiliations
Ethics declarations
Conflict of Interest
Carrie Huang and Allen Huang declare no conflict of interest. Andrew Levy reports grants from National Institutes of Health (T32 Training Grant 5T32-HL-007822-19) during the conduct of the study. Michael Ho reports personal fees from Janssen, outside of this submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Coronary Heart Disease
Rights and permissions
About this article
Cite this article
Levy, A.E., Huang, C., Huang, A. et al. Recent Approaches to Improve Medication Adherence in Patients with Coronary Heart Disease: Progress Towards a Learning Healthcare System. Curr Atheroscler Rep 20, 5 (2018). https://doi.org/10.1007/s11883-018-0707-0
Published:
DOI: https://doi.org/10.1007/s11883-018-0707-0