Abstract
Summary
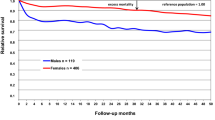
This study describes in detail the burden of caring for patients aged ≥ 50 years seen in one year with a fragility fracture in a large urban environment and shows that these fractures result in a long length of stay and significant mortality. Intervention to prevent further fracture was poorly done.
Purpose
To examine the epidemiology of fragility fracture in patients over age 50 years and record the number who received appropriate secondary prevention treatment.
Methods
All patients aged ≥ 50 years presenting with a fracture during the 12 months following July 1st 2011, to Auckland City Hospital or residing in central Auckland at the time of their fracture, were identified from hospital and Accident Compensation Corporation records. A random sample of 55% of these patient’s records were reviewed to establish the type of fracture, prior fracture and falls history, and use of bisphosphonates in the 12 months before presentation. Their length of stay (LOS) by type of fracture was recorded. The use of bisphosphonate drugs in the following 12 months was obtained from centralised national records of prescriptions.
Results
2729 patients aged ≥ 50 years presented with a fragility fracture in the central Auckland region in one year. Fifty-six percent of these patients were seen at Auckland Hospital and of these, 82% patients required admission with a mean LOS of 20 days (SD ± 24 days).The remaining 44% of patients were looked after in the private outpatient sector. Approximately 30% of the admissions were for hip fracture. Sixty-four percent of patients with a fragility fracture did not receive a potent bisphosphonate, 12% were considered not appropriate for treatment, and 24% received a potent bisphosphonate during their admission or in the next 12 months.
Conclusions
Approximately 1 in 18 people aged ≥ 50 years presented in one year with a fragility fracture.Secondary prevention strategies were poorly implemented. Additional resources for identifying and initiating secondary fracture prevention care such as a Fracture Liaison Service are urgently needed.
Similar content being viewed by others
References
Brown P, McNeill R, Leung W, Radwan E, Willingale J (2011) Current and future economic burden of osteoporosis in New Zealand. Appl Health Econ Health Policy 9:111–123
Fergus L, Cutfield G, Harris R (2011) Auckland City Hospital’s ortho-geriatric service: an audit of patients aged over 65 with fractured neck of femur. N Z Med J 124:40–54
Walker N, Norton R, Vander Hoorn S, Rodgers A, MacMahon S, Clark T, Gray H (1999) Mortality after hip fracture: regional variations in New Zealand. N Z Med J 112(1092):269–271
Marsh D, Akesson K, Beaton DE, Bogoch ER, Boonen S, Brandi ML, McLellan AR, Mitchell PJ, Sale JE, Wahl DA (2011) IOF CSA fracture working group. Coordinator-based systems for secondary prevention in fragility fracture patients. Osteoporos Int 22(7):2051–2065. doi:10.1007/s00198-011-1642-x
Åkesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C (2013) IOF Fracture Working Group. Capture the Fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24:2135–2152
Health Quality and Safety Commission Atlas of healthcare variation: Falls. http://www.hqsc.govt.nz/our-programmes/health-quality-evaluation/projects/atlas-of-healthcare-variation/falls/. Accessed 14 Dec 2016
Dreinhofer KE, Anderson M, Feron JM et al (2005) Multinational survey of osteoporotic fracture management. Osteoporos Int 16:S44–S53
Kenealy H, Paul S, Walker K, Garg A (2011) Secondary prophyaxis of osteoporotic fractures in an orthogeriatric service. Austr J of Ageing 30:41
Bloomfield K, Singh J (2011) Secondary prevention of vertebral fractures in a large New Zealand district health board. N Z Med J 124:26–33
Mitchell PJ (2009) Fracture liaison services: a systematic approach to secondary fracture prevention. Osteoporosis Review 17:14–16
Mitchell PJ (2013) Best practices in secondary fracture prevention: fracture liaison services. Curr Osteoporos Rep 11(1):52–60. doi:10.1007/s11914-012-0130-3
Huntjens KM, van Geel TA, van den Bergh JP, van Helden S, Willems P, Winkens B, Eisman JA, Geusens PP, Brink PR (2014) Fracture liaison service: impact on subsequent nonvertebral fracture incidence and mortality. J Bone Joint Surg Am 96(4):e29. doi:10.2106/JBJS.L.00223
Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR, Eisman JA, March L, Seibel MJ (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int 24(2):393–406. doi:10.1007/s00198-012-2090-y
Osteoporosis New Zealand (2012) Bone Care 2020: A systematic approach to hip fracture care and prevention for New Zealand. Wellington
Acknowledgments
We acknowledge with thanks a grant from Merck Sharpe and Dohme for salary support for the research nurse.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Geoffrey Braatvedt has received financial assistance to attend scientific meetings from Merck Sharpe and Dohme and Eli Lilly. He has sat on an advisory board to MSD and received research grants from MSD and Eli Lilly.
Conflict of interest
Susan Wilkinson, Marilyn Scott and Roger Harris declare no conflict of interest. Paul Mitchell has undertaken consultancy for governments, national osteoporosis societies, healthcare professional organizations and private sector companies throughout the world relating to systematic approaches to fragility fracture care and prevention.
Rights and permissions
About this article
Cite this article
Braatvedt, G., Wilkinson, S., Scott, M. et al. Fragility fractures at Auckland City Hospital: we can do better. Arch Osteoporos 12, 64 (2017). https://doi.org/10.1007/s11657-017-0353-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-017-0353-0