Abstract
Purpose
To investigate PSA- and PHI (prostate health index)-based models for prediction of prostate cancer (PCa) and the feasibility of using DRE-estimated prostate volume (DRE-PV) in the models.
Methods
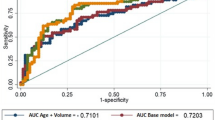
This study included 569 Chinese men with PSA 4–10 ng/mL and non-suspicious DRE with transrectal ultrasound (TRUS) 10-core prostate biopsies performed between April 2008 and July 2015. DRE-PV was estimated using 3 pre-defined classes: 25, 40, or 60 ml. The performance of PSA-based and PHI-based predictive models including age, DRE-PV, and TRUS prostate volume (TRUS-PV) was analyzed using logistic regression and area under the receiver operating curves (AUC), in both the whole cohort and the screening age group of 55–75.
Results
PCa and high-grade PCa (HGPCa) was diagnosed in 10.9 % (62/569) and 2.8 % (16/569) men, respectively. The performance of DRE-PV-based models was similar to TRUS-PV-based models. In the age group 55–75, the AUCs for PCa of PSA alone, PSA with DRE-PV and age, PHI alone, PHI with DRE-PV and age, and PHI with TRUS-PV and age were 0.54, 0.71, 0.76, 0.78, and 0.78, respectively. The corresponding AUCs for HGPCa were higher (0.60, 0.70, 0.85, 0.83, and 0.83). At 10 and 20 % risk threshold for PCa, 38.4 and 55.4 % biopsies could be avoided in the PHI-based model, respectively.
Conclusions
PHI had better performance over PSA-based models and could reduce unnecessary biopsies. A DRE-assessed PV can replace TRUS-assessed PV in multivariate prediction models to facilitate clinical use.

Similar content being viewed by others
References
Schröder FH, Hugosson J, Roobol MJ, Tammela TL, Zappa M, Nelen V et al (2014) Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet 384(9959):2027–2035
Andriole GL, Crawford ED, Grubb RL 3rd, Ss Buys, Chia D, Church TR et al (2009) Mortality results from a randomized prostate-cancer screening trial. N Engl J Med 360(13):1310–1319
Kranse R, Roobol MJ, Schröder FH (2008) A graphical device to represent the outcomes of a logistic regression analysis, an illustration of its possible use in prostate cancer screening and prostate cancer treatment counseling. Prostate 68:1674–1680
Roobol MJ, van Vugt HA, Loeb S, Zhu X, Bul M, Bangma CH et al (2012) Prediction of prostate cancer risk: the role of prostate volume and digital rectal examination in the ERSPC risk calculators. Eur Urol 61:577–583
Ankerst DP, Hoefler J, Bock S, Goodman PJ, Vickers A, Hernandez J et al (2014) The Prostate Cancer Prevention Trial risk calculator 2.0 for the prediction of low- versus high-grade prostate cancer. Urology 83(6):1362–1367
Catalona WJ, Partin AW, Sanda MG, Wei JT, Klee GG, Bangma CH et al (2011) A multicenter study of [-2] pro-prostate specific antigen combined with prostate specific antigen and free prostate specific antigen for prostate cancer detection in the 2.0 to 10.0 ng/ml prostate specific antigen range. J Urol 185(5):1650–1655
Abrate A, Lughezzani G, Gadda GM, Lista G, Kinzikeeva E, Fossati N et al (2014) Clinical use of [-2] proPSA (p2PSA) and its derivatives (%p2PSA and Prostate Health Index) for the detection of prostate cancer: a review of the literature. Korean J Urol 55(7):436–445
Ng CF, Chiu PKF, Lam N, Lam HC, Lee KW, Hou SS (2014) The Prostate Health Index in predicting initial prostate biopsy outcomes in Asian men with prostate-specific antigen levels of 4–10 ng/mL. Int Urol Nephrol 46(4):711–717
Lughezzani G, Lazzeri M, Larcher A, Lista G, Scattoni V, Cestari A et al (2012) Development and internal validation of a Prostate Health Index based nomogram for predicting prostate cancer at extended biopsy. J Urol 188:1144–1150
Roobol MJ, Vedder MM, Nieboer D, Hougatte A, Vincendeau S, Lazzeri M et al (2015) Comparison of two prostate cancer risk calculators that include the Prostate Health Index. EU Focus 1(2):185–190
Ankerst DP, Till C, Boeck A, Goodman P, Tangen CM, Feng Z et al (2013) The impact of prostate volume, number of biopsy cores, and AUA symptom score on the sensitivity of cancer detection using the Prostate Cancer Prevention Trial Risk Calculator. J Urol 190(1):70–76
Vickers AJ, Cronin AM, Roobol MJ, Hugosson J, Jones JS, Kattan MW et al (2010) The relationship between prostate-specific antigen and prostate cancer risk: the Prostate Biopsy Collaborative Group. Clin Cancer Res 16:4374–4381
Chen R, Ren SC, Chinese Prostate Cancer Consortium, Yiu MK, Ng CF, Cheng WS et al (2014) Prostate cancer in Asia: a collaborative report. Asian J Urol 1(1):15–27
Teoh JY, Yuen SK, Tsu JH, Wong CK, Ho BSh, Ng AT et al (2015) Prostate cancer detection upon transrectal ultrasound-guided biopsy in relation to digital rectal examination and prostate-specific antigen level: what to expect in the Chinese population? Asian J Androl 17(5):821–825
Semjonow A, Köpke T, Eltze E, Pepping-Schefers B, Burgel H, Darte C (2010) Pre-analytical in vitro stability of [-2] proPSA in blood and serum. Clin Chem 43(10–11):926–928
Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL, ISUP Grading Committee (2005) The 2005 International Society of Urological Pathology (ISUP) consensus conference on gleason grading of prostatic carcinoma. Am J Surg Pathol 29(9):1228–1242
Loeb S, Han M, Roehl KA, Antenor JA, Catalona WJ (2005) Accuracy of prostate weight estimation by digital rectal examination versus transrectal ultrasonography. J Urol 173:63–65
Ren S, Peng Z, Mao JH et al (2012) RNA-seq analysis of prostate cancer in the Chinese population identifies recurrent gene fusions, cancer-associated long noncoding RNAs and aberrant alternative splicings. Cell Res 22:806–821
Rubin MA, Maher CA, Chinnaiyan AM (2011) Common gene rearrangements in prostate cancer. J Clin Oncol 29:3659–3668
Yoon BI, Shin TS, Cho HJ et al (2012) Is it effective to perform two more prostate biopsies according to prostate-specific antigen level and prostate volume in detecting prostate cancer? Prospective study of 10-core and 12-core prostate biopsy. Urol J. Spring 9(2):491–497
Mottet N, Bellmunt J, Briers E et al (2016) European Association of Urology (EAU) Prostate cancer guidelines. (uroweb.org/guideline)
Acknowledgments
The instruments and testing reagents for the study were provided by Beckman Coulter Limited, but it has no role in all parts of the study and manuscript.
Funding
There was no funding for the study. The instruments and testing reagents for the study were provided by Beckman Coulter Limited, but it has no role in the study design, data analysis, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants in the study.
Rights and permissions
About this article
Cite this article
Chiu, P.K.F., Roobol, M.J., Teoh, J.Y. et al. Prostate health index (PHI) and prostate-specific antigen (PSA) predictive models for prostate cancer in the Chinese population and the role of digital rectal examination-estimated prostate volume. Int Urol Nephrol 48, 1631–1637 (2016). https://doi.org/10.1007/s11255-016-1350-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-016-1350-8