Abstract
The ongoing COVID-19 pandemic has caused significant psychological impact on medical professionals, including medical students, many who have been caring for patients on the frontlines. Understanding how medical students perceive their stressful life experiences is important as the mental health of these future physicians directly impacts their ability to care for patients. We assessed for post-traumatic growth and resilience in the face of traumatic events among a cohort of medical students that attended a medical school located in an early epicenter of the COVID-19 pandemic. Between October 29, 2020 and December 1, 2020, medical students at the Icahn School of Medicine at Mount Sinai in New York City were surveyed on various stressful life events, including COVID-19. We identified specific resilience behaviors, including establishing a supportive social network, relying on a moral compass, and using cognitive flexibility, that medical students commonly used to cope with traumatic experiences. Compared with students who perceived COVID-19 as their most stressful life event, students who perceived other events, such as family issues or serious illness, as most stressful experienced less COVID-related stress (t = -2.2, p = .03), greater posttraumatic growth (t = 4.3, p < .001), and demonstrated more resilient behaviors including establishing and nurturing a supportive social network (t = 2.2, p = .03), developing brain fitness (t = 2.2, p = .03), and finding meaning and purpose in things (t = 2.9, p = .006). This suggests that stressful experiences prior to or in parallel with COVID-19 encouraged posttraumatic growth and development of resilience behaviors that were protective to COVID-19-related stress.
Similar content being viewed by others
Introduction
The mental health of healthcare workers at every level has been severely impacted during the COVID-19 pandemic. Prior studies during the SARS outbreak showed that healthcare workers caring for patients during the outbreak were at greater risk of developing anxiety, depression, and outbreak-related stress than the general population [1]. Initial studies on healthcare workers and medical students during the COVID-19 pandemic seem to support a similar conclusion. A study on 2,579 frontline healthcare workers (FHCWs) at the Mount Sinai Hospital during the Spring 2020 pandemic surge in New York found that 23.3% screened positively for COVID-19-related PTSD symptoms, 26.6% for MDD symptoms, and 25.0% for GAD symptoms [2]. While limited studies exist on American medical students, studies in China found that 25% of medical students (n = 7143) attending Changzi Medical School experienced COVID-19-related anxiety, while 27% of medical students at Sichuan University experienced COVID-19-related psychological distress, with 11% of students experiencing acute stress reaction to COVID-19 [3, 4]. In Chennai, India, medical student stress and anxiety significantly increased as a result of the COVID-19 pandemic and time in quarantine, as compared with prior measures in 2019 [5].
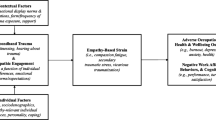
Since highly stressful life events such as the COVID-19 pandemic can negatively impact mental wellbeing, studying post-traumatic growth and resilience allows for greater understanding of how individuals maintain mental wellness in the wake of these events. Post-traumatic growth (PTG), coined first by Tedeschi and Calhoun in 1996 [6], is the set of positive psychological changes that may occur in the aftermath of traumatic or highly stressful events. In comparison, resilience helps individuals effectively cope with stress, allowing them to continue functioning in the wake of a traumatic event [7]. Although PTG often coexists with stress symptoms, resilience is negatively associated with stress symptoms and promotes an individual’s wellbeing. Due to their distinctive associations with stress symptoms, the relationship between PTG and resilience has been equivocal. A study on 9/11 survivors found that 15 years after the events 9/11, survivors exhibited 9/11-related PTG, with greater PTG associated with greater 9/11 exposure, higher post-traumatic stress symptoms, and greater indicators of psychosocial wellbeing [8]. Conversely, a study examining resilience in post-9/11 survivors found that while 65.1% of the sample exhibited resilience, survivors who had greater 9/11 exposure actually had less resilience [9]. Other studies on medical student response after the 3/11 triple disaster in Fukushima, Japan found that students who responded as volunteers to the 3/11 triple disaster exhibited both higher PTG and engaged in higher levels of resilient behaviors than their peers [10, 11].
Medical students have historically been an important source of aid during disasters such as 9/11 and the Fukushima 3/11 triple disaster, as well as during the current COVID-19 pandemic [12, 13]. Direct involvement in efforts related to the COVID-19 pandemic make medical students potentially subject to the same psychological consequences as other healthcare workers on the frontline, albeit with less professional experience on which to rely. Examining the impact that the COVID-19 pandemic had on medical students’ mental health and exploring post-traumatic growth and resilience in this population is thus important, especially since the mental health of medical students has direct implications for their future ability to care for patients as physicians.
The present study involved a medical student sample at the Icahn School of Medicine at Mount Sinai in New York City, which was located in an early epicenter of the COVID-19 pandemic. Since the earliest days of the COVID-19 pandemic in March of 2020, medical students at Mount Sinai were immediately mobilized to aid in a host of efforts to combat the spread of COVID-19. Students of all years helped package, deliver, and monitor PPE supplies, built ventilators, called to notify patients of COVID-19 test results, sought out advance care directives for hospitalized patients, delivered telehealth care to patients normally seen at a student-run free clinic, aided in grocery and medication delivery to homebound patients, and helped with childcare for frontline physicians. A number of fourth year medical students also graduated early and began working as frontline physicians treating COVID-positive patients. This population provided an opportunity to understand how medical students attending a medical school in an epicenter of the COVID-19 pandemic experienced COVID-19 stress, and how they were able to cope with the isolation, anxiety, and uncertainty of a global pandemic. We predicted that medical students who demonstrated greater resilience-promoting behaviors would experience less posttraumatic stress. We also predicted that students who experienced PTG as a result of a highly stressful life crisis other than the COVID-19 would experience less COVID-related stress, because their previously acquired PTG may be protective for COVID-related stress, or because the other events they experienced may have had a more severe impact than COVID-19.
To our knowledge, there are no existing studies on PTG and resilience of American medical students in the wake of the COVID-19 pandemic. Nor are there existing studies on how prior stressful experiences may affect a medical student’s PTG or resilience during the COVID-19 pandemic. We sought to fill this gap by a) allowing students to choose their most stressful life event to reflect upon (vs. only asking about response to a specific disaster); b) assessing their post-traumatic stress, PTG, resilience, and resilience-promoting behaviors in light of this stressful life event; and c) evaluating how their prior PTG, resilience, and resilience-promoting behaviors influenced their COVID-19-related stress.
Method
Participants
The primary sample for our study was a group of urban-dwelling, medical students at the Icahn School of Medicine at Mount Sinai in New York City. Table 1 provides descriptive statistics for the sample.
Procedure
We distributed an original survey via RedCap to medical students at the Icahn School of Medicine at Mount Sinai between October 29, 2020 and December 1, 2020. The survey assessed post-traumatic stress, post-traumatic growth, and resilience-promoting behaviors exhibited by medical students after experiencing stressful life events, including but not limited to COVID-19. We also surveyed the COVID-19 pandemic’s impact on students’ lives and assessed for COVID-19 related stress symptoms. Participants were initially informed of the study via an email blast from the research team. The URL for the survey was included in the email blast, and participants consented to participate in the study by indicating consent on the first page of the survey. Responses to the survey were anonymous. We also conducted optional interviews to provide qualitative insights and commonalities in students’ experiences.
All procedures were determined to be exempt from institutional review board review at the Icahn School of Medicine at Mount Sinai, under Exempt Category 2.
Measures
Post-traumatic Stress Symptoms
We used an adapted version of the Davidson Trauma Scale (DTS) to assess for post-traumatic stress symptoms. The DTS is a clinically validated 17-item scale that was developed as a self-assessment tool for post-traumatic stress disorder symptoms [14]. Compared to a semi-structured interview for diagnosing PTSD, the DTS has a sensitivity of 69.0% and specificity of 95.0% at a score of 40, which was recommended as the cut-off point for accurate classification of which individuals did or did not have PTSD [14]. In our study, we used a 12-item, adapted version of the DTS similar to Kaye-Kauderer et al.'s study on resilience in Fukushima medical students [11]. Respondents rated items using a 5-point scale, from 0 (not at all) to 4 (strongly agree), with a possible score range from 0–48. Prior studies have shown that the DTS has high internal reliability, with a test–retest reliability coefficient of .86 and a Cronbach’s alpha value of .99. In the current sample, the Cronbach’s alpha value was 0.72.
Post-traumatic Growth
We used the short form of the Post-Traumatic Growth Inventory (PTGI-SF) to assess for post-traumatic growth after the student’s most stressful life event. Post-traumatic growth is defined as the set of positive changes that individuals report in the aftermath of traumatic or highly stressful events [15, 16]. The 10-item PTGI-SF assesses post-traumatic growth across five domains: personal strength, relating to others, new possibilities, appreciation of life, and spiritual change, including two items from each of the five domains [16]. The PTGI-SF has high internal reliability, with Cronbach’s alpha value of .72–.84 across the five domains, and .89 for the overall scale [16]. In the current sample, the Cronbach’s alpha value was .86.
Resilience
We used two scales–the Connor-Davidson Resilience Scale (CD-RISC) and a newly-developed Resilience Behavior Scale (RBS)–to measure resilience, defined by Luthar et al. [7], as positive adaptations by individuals in the face of adversity.
The 10-item CD-RISC is a clinically validated scale that is a self-reporting tool for characteristics of resilience [17]. It asks respondents to rate items on a 5-point scale, from 0 (strongly disagree) to 4 (strongly agree), with a possible score range from 0–40. Prior studies have shown that the 10-item CDRS has good internal validity, with Cronbach’s alpha value of .85. In the current sample, the Cronbach’s alpha value was .858.
The RBS is a newly-introduced tool that identifies specific resilience promoting behaviors that individuals employ to cope with stress [18]. Based on a prior study using the RBS to survey resilience in Fukushima medical students [11], we asked participants to report 11 forms of behaviors they used to cope with the stressful event, including engaging in positive attitude/optimism, using cognitive flexibility, relying on moral compass, finding resilient role models, confronting fears, developing active coping skills, seeking social support, tending to physical wellbeing, developing brain fitness, focusing on strengths, and finding meaning/purpose in things. Respondents rated items on a 5-point scale, from 0 (strongly disagree) to 4 (strongly agree), with a possible score range from 0–44. Higher scores indicate more use of resilience promoting behaviors. In the current sample, the Cronbach’s alpha value was .904, demonstrating that this new scale has good internal validity.
COVID-19 Stress Symptoms
We assessed for loneliness, boredom, irritability, and intrusive thoughts (how often participants thought of COVID-19) in assessing for COVID-related stress, based prior studies [19] linking loneliness and social isolation experienced during COVID-19 to development of future depressive symptomatology. Respondents rated items using a 5-point scale, ranging from 0 (not at all) to 4 (enormously), with a possible score range from 0–20.
Results
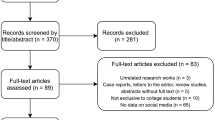
Table 1 illustrates the demographics of the participants of our study, with Fig. 1 as a visual representation of the most stressful events that medical students self-reported. While the majority (52.1%) of medical students indicated that the COVID-19 pandemic was their most stressful event, the remaining 47.9% of students indicated that another life event was most stressful to them, even in the context of the COVID-19 pandemic. Other traumatic events students indicated as most stressful included family issues, serious illness, relationship problems, bullying, and death of loved ones. Students who were interviewed also experienced a breakdown of stressful events similar to that of the students who were surveyed: half of the students indicated that their most stressful life event was not COVID-related, including an unexpected death of a parent and a severe illness of a sibling.
Students used an array of resilience behaviors as measured by the RBS to cope during their most stressful life event (Table 2). Behaviors most commonly used, as reflected by higher mean scores, included establishing a supportive social network, relying on a moral compass, and using cognitive flexibility. Students that were interviewed spoke of a wider ranging array of coping behaviors than the RBS could capture: some sought creative outlets (journaling, writing, art), while others turned to volunteering as a tangible way to get their mind off of pandemic-related stress. Leaning on family, trusted friends, and significant others in these difficult times was essentially ubiquitous for students who were interviewed.
We then assessed the correlation between the two resilience scales (RBS and CDRS) and the PTGI-SF. The RBS and the CDRS were positively correlated with one another (r = .53, p < .001). The RBS and the PTGI-SF were also positively correlated (r = .46, p < .001). However, there was no correlation between the CDRS-10 and the PTGI-SF (r = .03, n.s.).
Afterwards, we examined correlations between resilience and post-traumatic stress symptoms, resilience and desire to help during crises, and resilience and post-traumatic growth (Table 3). We chose to analyze two subsamples of students- those indicating a non-COVID-19 event as most stressful vs those indicating the COVID-19 pandemic as most stressful. There was no significant correlation between either resilience scale (CDRS-10 or RBS) and post-traumatic stress symptoms (measured by the DTS). There was also no significant correlation between either resilience scale and COVID-19-related stress.
There was a positive correlation between resilience behaviors (measured by the RBS) and wanting to help (p = .011)/feeling capable of helping (p = .014) among students who indicated a non-COVID-19 event as their most stressful event (Table 3). Additionally, there was a positive correlation between resilience traits (measured by the CDRS-10) and wanting to help (p = .027)/feeling capable of helping (p = .005) among students who indicated that COVID-19 was their most stressful event. Resilience measured by the RBS and post-traumatic growth were positively correlated in the subsample of students indicating a non-COVID-19 event as their most stressful event (p < .001). In contrast, resilience behaviors and post-traumatic growth were not significantly correlated in the subsample of students listing COVID-19 as their most stressful event.
Finally, we examined differences in PTG, resilience, and COVID-19 stress experienced by two subsamples of students: those indicating a non-COVID-19 event as most stressful versus those indicating the COVID-19 pandemic as most stressful (Table 4). Students who indicated a non-COVID-19 event as most stressful demonstrated significantly greater posttraumatic growth (p < .001), resilience behaviors (p = .033 for RBS-7, p = .034 for RBS-9, p = .006 for RBS-11), and less COVID-19 stress symptoms (p < .029) than students who indicated that COVID-19 was their most stressful event.
Discussion
Using a sample of medical students from a medical school located at an epicenter of the COVID-19 pandemic in the U.S, we gained insight into the most stressful events that students experienced, including but not limited to COVID-19, and assessed their post-traumatic growth and resilience. First, almost half of all students in our study indicated that an event outside of COVID was most stressful to them. Most of these events were deeply personal in nature, such as family issues, serious illness, relationship problems, bullying, and death of loved ones. Even at a relatively young age and early on in their medical training, students had experienced stressful life events that could potentially shape their response to COVID-related stress.
Second, we identified specific resilience promoting behaviors (from the RBS) that students in our study commonly used to cope with these stressful events. Common resilience behaviors used included seeking social support, adopting positive attitudes/reevaluation of the trauma, and relying on moral compass/personal values. This is in line with prior studies in preclinical medical students showing that to cope with stress, students commonly used strategies such as personal engagement, positive reinterpretation of the situation, and seeking support programs [20]. Students that we interviewed confirmed similar resilience behaviors to cope with traumatic events–they relied on family, friends, and significant others as their primary support system, stayed consistent to their values, and sought professional help when needed. Specifically to cope with COVID-19 stress and isolation, students mentioned adopting routines to give their days structure, volunteering as an outlet to give them a continued sense of purpose, and seeking creative outlets (writing, journaling, art) to destress. In future studies, it would be interesting to compare the resilience behaviors exhibited by medical students, a self-selecting group of community-minded individuals with access to higher education, to a wider population of young people across different professions.
Third, we gained insight into how the two resilience scales–CD-RISC and the RBS–were related to each other. The CD-RISC focuses on self-perceived personality traits whereas the RBS focuses on behaviors, and they were positively correlated with one another, in line with the fact that both scales measure overlapping aspects of an individual’s resilience. However, the RBS was positively correlated with PTG, while the CDRS-10 was not. This indicates that the CDRS-10 and the RBS may be measuring different aspects of a person’s resilience. Specific resilience promoting behaviors, measured by the RBS, may be more adoptable and dynamic, correlating with transformational experience of growth after trauma. In contrast, resilience traits, as measured by the CDRS-10, may be less positively correlated with post-traumatic growth. An already highly resilient person who scored high on the CDRS-10 may not have as much growth measured after trauma, because psychological struggle that is required for growth might not be necessary for them or they already demonstrated a high functioning, leading to lower levels of PTG experiences.
We did not identify an expectable negative correlation in our population of students between resilience and post-traumatic stress symptoms, or between resilience and COVID-19-related stress. One potential explanation for this is that our survey of stress symptoms may not have encompassed the full magnitude of symptoms escalating to a post-traumatic diagnosis. Future work could involve determining whether resilience is negatively correlated with symptoms escalating to a post-traumatic diagnosis such as acute stress disorder or post-traumatic stress disorder.
Our research revealed positive correlations between resilience and wanting to help/feeling capable of helping during a crisis. This is consistent with prior findings of higher levels of resilience in Japanese medical student volunteers versus non-volunteers after the 3/11 disaster in Fukushima [10, 11]. We were able to further delve into this correlation by distinguishing resilience traits from behaviors. Resilient traits (CDRS-10) were positively associated with wanting to help/feeling capable of helping in students who indicated COVID-19 as their most stressful event, while resilient behaviors (RBS) were positively associated with wanting to help/feeling capable of helping in students who indicated a non-COVID-19 event as most stressful. And, only in the non-COVID-19 subsample of students, PTG was positively correlated with resilient behaviors. An intriguing explanation for these collective findings may be that prior experience with traumatic stressors spurred PTG over time, which in turn fostered more resilient behaviors in the face of COVID-19 (assuming non-COVID-19 events were not contemporaneous with the pandemic). Whereas, in those students who found COVID-19 the most stressful, insufficient time had elapsed to allow for PTG and for translating feeling resilient into behaving resiliently, especially as the pandemic was ongoing at the time of this study. A longitudinal study would be required to further vet these or other potential causal connections between stressful events, resilient traits, resilient behaviors, PTG and helping in times of crisis.
Finally, we assessed differences in coping with COVID-19 stress between two groups of students: those who indicated a non-COVID-19 event as most stressful versus those who indicated the COVID-19 pandemic as most stressful. We found that students who indicated a non-COVID-19 event as most stressful demonstrated significantly greater PTG (p < .001), greater resilience behaviors (p = .033 for RBS-7: Established and nurtured supportive social network, p = .034 for RBS-9: Developed brain fitness, p = .006 for RBS-11: Found meaning and purpose in things), and less COVID-19 stress symptoms (p < .029) than students who indicated that COVID-19 was their most stressful event. This suggests that non-COVID-19 stressful events were potentially more personal and impactful, which in turn must have challenged or shaken their worldviews, and led to self-recognition of PTG and resilience behaviors that were protective against COVID-19-related stress.
Qualitative data from our interviews seemed to support our findings that prior traumatic events may have instilled resilience behaviors that were protective against COVID-19-related stress. Students mentioned the “if I could get through that, I can get through this” mentality when asked about how their prior stressful events may have impacted their response to COVID-19. Interestingly, others described the circumstances of the COVID-19 pandemic as a “hidden blessing,” giving them increased flexibility to be with family and serve as a source of support for non-COVID-19 related illness or death.
Prior studies have explored the effect of previous stress or trauma on an individual’s response to future stressful or traumatic events, with equivocal findings. Stress-inoculation training (SIT), a cognitive-behavioral therapy aimed at exposing individuals to repeated stressful stimuli in order to strengthen coping mechanisms, decreased levels of stress, anxiety, and depression in cancer patients [21, 22]. In contrast, a study in Chilean primary care providers found that individuals experiencing multiple stressors before the 2010 earthquake in Chile were more vulnerable to developing MDD or PTSD after the earthquake [23]. Furthermore, a study in Israeli trauma survivors showed that PTG attributed to prior trauma actually sensitized individuals to greater intrusion, avoidance, and hyperarousal symptoms during the COVID-19 pandemic [24]. It is possible that multiple prior stressors can either be protective or handicapping in the face of a future stressor depending upon other factors. While prior stressful or traumatic events may condition an individual to be resilient in the face of future events, if the trauma experienced reaches a particular threshold of severity, it may lead to greater vulnerability to future mental health conditions. Alternatively, experiencing prior trauma may give an individual a heightened awareness of their own symptoms, equipping them with more precise language to describe their symptoms, which may also lead to higher reported symptoms when surveyed about later traumas.
In addition to studying how prior traumas can impact an individual’s resilience, an individual’s understanding of resilience itself is also subjective. Medical student interviews provided more insight into the complexities of how students defined resilience: “[Resilience] is not being unaffected by a stressful event, but rather, being able to go on or get stronger.” “[Resilience] is faith that even if things get really bad, you’ll still be able to move on somehow.” “It is consistent strength in the face of obstacles.” “It’s a cop-out term for the medical system: trying to put the onus of self-care on medical students and providers.” This last point is one that highlights the importance of not studying resilience in a vacuum–hospital leadership cannot solely place the responsibility of mental wellness on an individual’s own coping skills, but should in conjunction be proactively working to expand accessible and affordable mental health care for all staff. One recent study illustrating this point showed that perceived support from hospital leadership for its employees was one of the greatest protective factors for symptoms of MDD and GAD during the COVID-19 pandemic [2].
Several limitations exist in our study. First, we studied medical students from a single medical school in NYC, limiting the generalizability of our findings to locations less affected by the pandemic. Second, selection bias exists with administering a voluntary survey and optional interview–the experience of the students who felt compelled to respond may not be generalizable to all medical students at the school. Third, given our smaller sample size and the anonymous nature of the survey, we did not explore correlations between gender, race, ethnicity, socioeconomic status, and COVID-19 stress, resilience traits, or PTG. Since COVID-19 has had a disproportionate impact on communities of color and exacerbated existing financial vulnerabilities, future research focusing on these factors with a larger number of medical students would be important. Fourth, we measured PTG when the COVID-19 pandemic was still prevailing; PTG is usually measured after a traumatic event, after enough time has passed to allow for the growth to occur [2, 6]. Consequently, for students who indicated COVID-19 as their most stressful event, it is possible that their PTG is lower than it would be if we measured it again several years later.
Future studies are needed to examine PTG and resilience after the COVID-19 pandemic has ended and compare results to our current findings. Additionally, further research is needed to continue to determine the effect of prior stressful events on PTG, resilience, and coping with peritraumatic stress. It would be useful to explore whether the type of prior trauma (e.g. personal in nature vs. natural disaster), the time elapsed since the trauma (e.g. months vs. years ago), and the demographics/background of individuals experiencing the trauma would affect whether the prior event is provoking or protective for future traumatic events. Finally, cross-cultural comparisons of PTG and resilience would be interesting to explore, for example, investigating how Fukushima medical students coped with COVID-19 as compared with American medical students.
Our study identified specific resilience behaviors that medical students used to cope with traumatic events, including establishing a supportive social network, relying on a moral compass, and using cognitive flexibility. It also demonstrated that stressful experiences prior to or in parallel to COVID-19 encouraged posttraumatic growth and development of resilience behaviors that were protective to COVID-19-related stress. Our findings have implications for how medical institutions can be better informed to provide support for medical students in times of crisis: by encouraging awareness of resilience behaviors, increasing flexibility for students to be supported among family and friends, and providing consistently accessible mental health support and therapy.
References
Wu KK, Chan SK, Ma TM. Posttraumatic Stress after SARS. Emerg Infect Dis. 2005;11(8):1297–300. https://doi.org/10.3201/eid1108.041083.
Feingold JH, Peccoralo L, Chan CC, Kaplan CA, Kaye-Kauderer H, Charney D, Verity J, Hurtado A, Burka L, Syed SA, Murrough JW, Feder A, Pietrzak RH, Ripp J. Psychological Impact of the COVID-19 Pandemic on Frontline Health Care Workers During the Pandemic Surge in New York City. Chronic Stress. 2021;5:2470547020977891. https://doi.org/10.1177/2470547020977891.
Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287: 112934. https://doi.org/10.1016/j.psychres.2020.112934.
Chandratre S. Medical Students and COVID-19: Challenges and Supportive Strategies. J Med Educ Curric Dev. 2020;7:2382120520935059. https://doi.org/10.1177/2382120520935059.
Saraswathi I, Saikarthik J, Senthil Kumar K, Madhan Srinivasan K, Ardhanaari M, Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ. 2020;8: e10164. https://doi.org/10.7717/peerj.10164.
Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress. 1996;9(3):455–71. https://doi.org/10.1007/BF02103658.
Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 2000;71(3):543–62. https://doi.org/10.1111/1467-8624.00164.
Pollari CD, Brite J, Brackbill RM, Gargano LM, Adams SW, Russo-Netzer P, Davidov J, Banyard V, Cone JE. World Trade Center Exposure and Posttraumatic Growth: Assessing Positive Psychological Change 15 Years after 9/11. Int J Environ Res Public Health. 2020;18(1):104. https://doi.org/10.3390/ijerph18010104.
Bonanno GA, Galea S, Bucciarelli A, Vlahov D. Psychological resilience after disaster: New York City in the aftermath of the September 11th terrorist attack. Psychol Sci. 2006;17(3):181–6. https://doi.org/10.1111/j.1467-9280.2006.01682.x.
Anderson D, Prioleau P, Taku K, Naruse Y, Sekine H, Maeda M, Yabe H, Katz C, Yanagisawa R. Post-traumatic Stress and Growth Among Medical Student Volunteers After the March 2011 Disaster in Fukushima Japan: Implications for Student Involvement with Future Disasters. Psychiatr Q. 2016;87(2):241–51. https://doi.org/10.1007/s11126-015-9381-3.
Kaye-Kauderer HP, Levine J, Takeguchi Y, Machida M, Sekine H, Taku K, Yanagisawa R, Katz C. Post-Traumatic Growth and Resilience Among Medical Students After the March 2011 Disaster in Fukushima. Japan Psychiatr Q. 2019;90(3):507–18. https://doi.org/10.1007/s11126-019-09646-z.
Bazan D, Nowicki M, Rzymski P. Medical students as the volunteer workforce during the COVID-19 pandemic: Polish experience. Int J Disaster Risk Reduct. 2021;55: 102109. https://doi.org/10.1016/j.ijdrr.2021.102109.
Katz CL, Gluck N, Maurizio A, DeLisi LE. The medical student experience with disasters and disaster response. CNS Spectr. 2002;7(8):604–10. https://doi.org/10.1017/s1092852900018216.
Davidson JR, Book SW, Colket JT, Tupler LA, Roth S, David D, Hertzberg M, Mellman T, Beckham JC, Smith RD, Davison RM, Katz R, Feldman ME. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychol Med. 1997;27(1):153–60. https://doi.org/10.1017/s0033291796004229.
Cann A, Calhoun LG, Tedeschi RG, Taku K, Vishnevsky T, Triplett KN, Danhauer SC. A short form of the Posttraumatic Growth Inventory. Anxiety Stress Coping. 2010;23(2):12737. https://doi.org/10.1080/10615800903094273.
Tedeschi RG, Cann A, Taku K, Senol-Durak E, Calhoun LG. The Posttraumatic Growth Inventory: A Revision Integrating Existential and Spiritual Change. J Trauma Stress. 2017;30(1):11–8. https://doi.org/10.1002/jts.22155.
Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J Trauma Stress. 2007;20(6):1019–28. https://doi.org/10.1002/jts.20271.
Southwick S, Charney D. Resilience: The Science of Mastering Life’s Greatest Challenges. England: Cambridge University Press; 2018. https://books.google.com/books/about/Resilience.html?hl=&id=7JheDwAAQBAJ.
Hwang T-J, Rabheru K, Peisah C, Reichman W, Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. Int Psychogeriatr. 2020;32(10):1217–20. https://doi.org/10.1017/s1041610220000988.
Fares J, Al Tabosh H, Saadeddin Z, El Mouhayyar C, Aridi H. Stress Burnout and Coping Strategies in Preclinical Medical Students. N Am J Med Sci. 2016;8(2):75–81. https://doi.org/10.4103/1947-2714.177299.
Kashani F, Kashani P, Moghimian M, Shakour M. Effect of stress inoculation training on the levels of stress anxiety and depression in cancer patients. Iran J Nurs Midwifery Res. 2015;20(3):359–64. https://www.ncbi.nlm.nih.gov/pubmed/26120337.
Miechenbau D. Stress Inoculation Training. Boston: Allyn & Bacon; 1985. https://books.google.com/books/about/Stress_Inoculation_Training.html?hl=&id=cBJrPwAACAAJ.
Fernandez CA, Choi KW, Marshall BDL, Vicente B, Saldivia S, Kohn R, Koenen KC, Arheart KL, Buka SL. Assessing the relationship between psychosocial stressors and psychiatric resilience among Chilean disaster survivors. Br J Psychiatry. 2020;217(5):630–7. https://doi.org/10.1192/bjp.2020.88.
Hamam AA, Milo S, Mor I, Shaked E, Eliav AS, Lahav Y. Peritraumatic reactions during the COVID-19 pandemic - The contribution of posttraumatic growth attributed to prior trauma. J Psychiatr Res. 2021;132:23–31. https://doi.org/10.1016/j.jpsychires.2020.09.029.
Funding
This study was funded by the Mount Sinai Department of Global Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed Consent
Informed consent was obtained from all participants, and participants consented to participating in the study by indicating consent on the first page of the survey.
Research Involving Human Participants
All procedures were determined to be exempt from institutional review board review by the Mount Sinai Grants and Contracts Office, under Exempt Category 2(i): “Research involving the use of educational tests, survey procedures, interview procedures or observation of public behavior and information obtained is recorded by the investigator in such a manner that the identity of the human subjects cannot readily be ascertained.”
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luo, C., Santos-Malave, G., Taku, K. et al. Post-traumatic Growth and Resilience among American Medical Students during the COVID-19 Pandemic. Psychiatr Q 93, 599–612 (2022). https://doi.org/10.1007/s11126-022-09981-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-022-09981-8