Abstract
Purpose
The purpose of this study was to determine the heterotopic pregnancy rate using fresh versus frozen-thawed embryo transfers and factors associated with heterotopic pregnancy (HP). Management and clinical outcomes after heterotopic pregnancy were also evaluated.
Methods
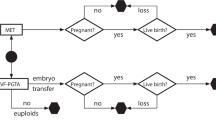
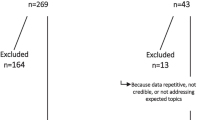
In this retrospective cohort study, we included 12,484 women who had clinical pregnancies after in vitro fertilization treatment at our fertility center between 2012 and 2017. Patients received fresh day 3 embryos (F-D3 group), fresh day 5 blastocysts (F-D5 group), frozen-thawed day 3 embryos (T-D3 group), or frozen-thawed day 5 or 6 blastocysts (T-D5/6 groups) transfers. The primary outcome measure was the occurrence of heterotopic pregnancy. Factors associated with heterotopic pregnancy were analyzed using logistic regression.
Results
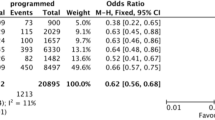
The heterotopic pregnancy rates were 0.58% in the F-D3, 0.39% in F-D5, 0.56% in T-D3, and 0.33% in T-D5/6 groups, but no differences were found between groups. The risk factors of HP included a history of previous ectopic pregnancy (odds ratio [OR] 5.805, 95% CI 4.578–9.553, P = 0.016) and pelvic inflammation diseases (OR 1.129, 95% CI 1.021–3.178, P = 0.047). Salpingectomy was performed in 62.9% patients either through laparoscopy or through laparotomy. The early abortion rate and late abortion rate were 29.03% and 1.61%, respectively. In total, 66.13% of the patients had a live birth, either a singleton (90.24%) or twins (9.76%).
Conclusion
No significant difference in the incidence of heterotopic pregnancy in fresh IVF cycles vs. frozen-thawed cycles could be demonstrated in a large cohort of patients. The risk factors of HP included history of ectopic pregnancy and PID. The clinical outcome after heterotopic pregnancy appears to be favorable.
Similar content being viewed by others
References
Talbot K, Simpson R, Price N, Jackson SR. J Obstet Gynaecol. 2011;31:7–12.
Mustafa KB, Hamid HA, Lim PS, Razi ZR, Omar MH. Heterotopic triplet pregnancy with bilateral tubal ectopic post-IVF-ICSI of two 12-cell embryos. Taiwan J Obstet Gynecol. 2016;55:142–4. https://doi.org/10.1016/j.tjog.2015.04.006.
Liu M, et al. Risk factors and early predictors for heterotopic pregnancy after in vitro fertilization. PLoS One. 2015;10:e0139146. https://doi.org/10.1371/journal.pone.0139146.
Ko JK, Cheung VY. A 12-year experience of the management and outcome of heterotopic pregnancy at Queen Mary Hospital, Hong Kong, China. Int J Gynaecol Obstet. 2012;119:194–5. https://doi.org/10.1016/j.ijgo.2012.06.006.
Yu Y, Xu W, Xie Z, Huang Q, Li S. Management and outcome of 25 heterotopic pregnancies in Zhejiang, China. Eur J Obstet Gynecol Reprod Biol. 2014;180:157–61. https://doi.org/10.1016/j.ejogrb.2014.04.046.
Knopman JM, Talebian S, Keegan DA, Grifo JA. Heterotopic abdominal pregnancy following two-blastocyst embryo transfer. Fertil Steril. 2007;88(1437):e1413–35. https://doi.org/10.1016/j.fertnstert.2006.12.083.
Clayton HB, et al. A comparison of heterotopic and intrauterine-only pregnancy outcomes after assisted reproductive technologies in the United States from 1999 to 2002. Fertil Steril. 2007;87:303–9. https://doi.org/10.1016/j.fertnstert.2006.06.037.
Santos-Ribeiro S, Tournaye H, Polyzos NP. Trends in ectopic pregnancy rates following assisted reproductive technologies in the UK: a 12-year nationwide analysis including 160 000 pregnancies. Hum Reprod. 2016;31:393–402. https://doi.org/10.1093/humrep/dev315.
Li Z, Sullivan EA, Chapman M, Farquhar C, Wang YA. Risk of ectopic pregnancy lowest with transfer of single frozen blastocyst. Hum Reprod. 2015;30:2048–54. https://doi.org/10.1093/humrep/dev168.
Ishihara O, Kuwahara A, Saitoh H. Frozen-thawed blastocyst transfer reduces ectopic pregnancy risk: an analysis of single embryo transfer cycles in Japan. Fertil Steril. 2011;95:1966–9. https://doi.org/10.1016/j.fertnstert.2011.02.015.
Kwon YS, Lee SH, Im KS, Ro JH. Laparoscopic management of heterotopic interstitial pregnancy with subsequent term delivery. Int J Fertil Steril. 2015;9:265–7.
Goldman KN, Keltz J, Berg RE, Noyes NL. Heterotopic gestation with twin intrauterine implantation following transfer of three developmentally-delayed embryos from cryopreserved oocytes: a case report. J Reprod Med. 2015;60:436–40.
Buca DI, et al. Early diagnosis of heterotopic triplet pregnancy with an intrauterine and bilateral tubal pregnancy after IVF: a case report. J Obstet Gynaecol. 2015;35:755–6. https://doi.org/10.3109/01443615.2014.993940.
Shavit T, Paz-Shalom E, Lachman E, Fainaru O, Ellenbogen A. Unusual case of recurrent heterotopic pregnancy after bilateral salpingectomy and literature review. Reprod BioMed Online. 2013;26:59–61. https://doi.org/10.1016/j.rbmo.2012.10.006.
Shapiro BS, et al. Frozen-thawed embryo transfer is associated with a significantly reduced incidence of ectopic pregnancy. Fertil Steril. 2012;98:1490–4. https://doi.org/10.1016/j.fertnstert.2012.07.1136.
Bu Z, Xiong Y, Wang K, Sun Y. Risk factors for ectopic pregnancy in assisted reproductive technology: a 6-year, single-center study. Fertil Steril. 2016;106:90–4. https://doi.org/10.1016/j.fertnstert.2016.02.035.
Polyzos NP, Devroey P. Significantly lower ectopic pregnancy rates after frozen embryo transfer: implications toward segmentation of in vitro fertilization treatment. Fertil Steril. 2012;98:1419–20. https://doi.org/10.1016/j.fertnstert.2012.08.044.
Jun SH, Milki AA. Ectopic pregnancy rates with frozen compared with fresh blastocyst transfer. Fertil Steril. 2007;88:629–31. https://doi.org/10.1016/j.fertnstert.2006.12.005.
Jee BC, Suh CS, Kim SH. Ectopic pregnancy rates after frozen versus fresh embryo transfer: a meta-analysis. Gynecol Obstet Investig. 2009;68:53–7. https://doi.org/10.1159/000213048.
Londra L, et al. Ectopic pregnancy after in vitro fertilization: differences between fresh and frozen-thawed cycles. Fertil Steril. 2015;104:110–8. https://doi.org/10.1016/j.fertnstert.2015.04.009.
Evans J, et al. Fresh versus frozen embryo transfer: backing clinical decisions with scientific and clinical evidence. Hum Reprod Update. 2014;20:808–21. https://doi.org/10.1093/humupd/dmu027.
Horcajadas JA, et al. Controlled ovarian stimulation induces a functional genomic delay of the endometrium with potential clinical implications. J Clin Endocrinol Metab. 2008;93:4500–10. https://doi.org/10.1210/jc.2008-0588.
Haouzi D, et al. Controlled ovarian hyperstimulation for in vitro fertilization alters endometrial receptivity in humans: protocol effects. Biol Reprod. 2010;82:679–86. https://doi.org/10.1095/biolreprod.109.081299.
Jeon JH, et al. The risk factors and pregnancy outcomes of 48 cases of heterotopic pregnancy from a single center. J Korean Med Sci. 2016;31:1094–9. https://doi.org/10.3346/jkms.2016.31.7.1094.
Acknowledgements
Address all correspondence and requests for reprints to Yongzeng, Shenzhen Key Laboratory of Reproductive Immunology for Peri-implantation, Shenzhen Zhongshan Institute for Reproduction and Genetics, Fertility Center, Shenzhen Zhongshan Urology Hospital, Guangdong, People’s Republic of China. 510080. E-mail:zengyong1966@gmail.com.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure statement
The authors have nothing to disclose.
Rights and permissions
About this article
Cite this article
Xiao, S., Mo, M., Hu, X. et al. Study on the incidence and influences on heterotopic pregnancy from embryo transfer of fresh cycles and frozen-thawed cycles. J Assist Reprod Genet 35, 677–681 (2018). https://doi.org/10.1007/s10815-017-1109-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-017-1109-x