Abstract
Patients with conventional pacemakers or implanted defibrillators are often considered for cardiac resynchronization therapy (CRT). Our aim was to summarize the available evidences regarding the clinical benefits of upgrade procedures. A systematic literature search was performed from studies published between 2006 and 2017 in order to compare the outcome of CRT upgrade vs. de novo implantations. Outcome data on all-cause mortality, heart failure events, New York Heart Association (NYHA) Class, QRS narrowing and echocardiographic parameters were analysed. A total of 16 reports were analysed comprising 489,568 CRT recipients, of whom 468,205 patients underwent de novo and 21,363 upgrade procedures. All-cause mortality was similar after CRT upgrade compared to de novo implantations (RR 1.19, 95% CI 0.88–1.60, p = 0.27). The risk of heart failure was also similar in both groups (RR 0.96, 95% CI 0.70–1.32, p = 0.81). There was no significant difference in clinical response after CRT upgrade compared to de novo implantations in terms of improvement in left ventricular ejection fraction (ΔEF de novo − 6.85% vs. upgrade − 9.35%; p = 0.235), NYHA class (ΔNYHA de novo − 0.74 vs. upgrade − 0.70; p = 0.737) and QRS narrowing (ΔQRS de novo − 9.6 ms vs. upgrade − 29.5 ms; p = 0.485). Our systematic review and meta-analysis of currently available studies reports that CRT upgrade is associated with similar risk for all-cause mortality compared to de novo resynchronization therapy. Benefits on reverse remodelling and functional capacity improved similarly in both groups suggesting that CRT upgrade may be safely and effectively offered in routine practice. Clinical Trial Registration: Prospero Database—CRD42016043747
Similar content being viewed by others
Introduction
Cardiac resynchronization therapy (CRT) has been shown to improve cardiac function, symptoms and hospitalization and reduce all-cause mortality in heart failure patients with prolonged QRS and reduced ejection fraction [1]. Since chronic right ventricular pacing could be deleterious by increasing the risk of heart failure, all-cause mortality and atrial fibrillation [2, 3], patients implanted with conventional pacemaker or implantable cardioverter defibrillator (ICD) systems are often considered for upgrading to CRT.
Recent studies suggested that patients with typical left bundle branch block (LBBB) ECG morphology derive the most benefit from CRT [4, 5]. Although right ventricular pacing could trigger similar ventricular dyssynchrony to LBBB, data are scarce regarding the benefits of upgrading to CRT in patients with previously implanted cardiac pacemaker or ICD systems.
The latest ESC guidelines on cardiac pacing and resynchronization therapy recommends CRT upgrade as a class I indication (level B) for symptomatic patients (New York Heart Association (NYHA) III–IVa) with low ejection fraction (LVEF ≤ 35%) [6]; however, the most recent European heart failure guidelines restrict this indication as a class IIb (level B) [7], due to lack of randomized clinical data available. In contrast, ACC guidelines focus mostly on the percentage of right ventricular pacing rather than symptoms or functional status [8].
While we are awaiting further data of prospective clinical trials on the effects of CRT upgrade on left ventricular reverse remodelling and clinical outcomes, we need more data for routine clinical practice. Therefore, we aimed to provide a detailed analysis of the available evidence comparing clinical outcomes and long-term survival between CRT upgrade and de novo implantations.
Methods
Study selection
This systematic review was performed according to the PRISMA statement [9], and a predefined review protocol was published in the PROSPERO database under the registration number of CRD42016043747 [10]. A comprehensive search of PubMed, ResearchGate and GoogleScholar databases was performed from January 2006 to March 2017 focusing on full-sized, peer-reviewed, English language papers reporting data on patient outcomes after upgrade CRT vs. de novo implantations as a comparator group. In order to identify all potentially relevant articles, the search was performed by using the terms of (1) “upgrade” AND “CRT” and (2) “upgrade” AND “cardiac resynchronisation therapy”. The search was also extended by using the name of the most frequently cited authors of the identified studies. In addition, references of relevant review articles were also searched to find appropriate manuscripts.
Potentially relevant articles were evaluated by three independent reviewers (A.K., M.V., R.S.), and additional manuscripts were retrieved that either reviewer felt were potentially relevant. According to our review protocol, studies were accepted for analysis if (i) including heart failure patients with reduced ejection fraction (HFrEF) with de novo and upgrade CRT implantations, (ii) reporting all-cause mortality data or heart failure events and (iii) reporting echocardiographic (i.e. LVEF, end-diastolic volume (EDV)) or clinical (NYHA class) or ECG (QRS width) parameters of reverse remodelling (Supplementary Table 1). Heart failure events were defined as hospitalization due to progression of heart failure. Corresponding authors were contacted for unpublished information and permission in the case of missing relevant data sets. In order to evaluate the heterogeneity of patients who were enrolled into each therapy groups, the most important baseline clinical characteristics were collected and compared. Data on procedure-related complications were also collected if available.
Statistical analysis
All statistical analyses were conducted utilizing Comprehensive Meta-Analysis 3.3 (Biostat, Inc., USA) and GraphPad Prism Software Version 7 (GraphPad Prism Inc., San Diego, CA, USA). Heterogeneity between individual trial estimates was assessed using the Q statistic and I 2 statistic [11]. Since there was significant heterogeneity in the design and patient characteristics of the included studies, it was assumed that the true effect size varies from one study to the other, and hence, the random-effect model was used [12]. As a principal yet conservative measurement of the effect size (i.e. all-cause mortality), we calculated risk ratios (RRs) along with a 95% upper and lower confidence interval (CI) and compared the two therapy groups as case-control models. Additionally, meta-analysis was performed for publications where crude and/or adjusted hazard ratios (HRs) were also available. Sensitivity analysis with the inclusion of prospective studies only was performed. Forest plots were constructed showing the individual trials with the pooled estimates. Publication bias was assessed using the funnel plot, the trim and fill method of Duval and Tweedie [13] and an adjusted rank correlation test according to Begg and Mazumdar [14]. Since we did not have access to individual patient data from all studies reviewed, the median of delta values for LVEF, EDV, NYHA and QRS was calculated and compared between the two patient groups by using the Mann-Whitney U test. Methodological quality of all studies was assessed using the methodological index for non-randomized studies (MINORS) [15, 16]. Studies were defined to be low, moderate and high-quality studies based on their MINORS scores of < 8, < 16 and ≥ 16 points (Supplementary Table 2).
Results
Study characteristics
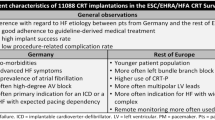
A total of 16 reports were selected for the current analysis comprising 489,568 CRT recipients, of whom 468,205 patients had de novo resynchronization therapy and 21,363 patients underwent an upgrade procedure (Fig. 1). The characteristics of all included studies are shown in Table 1. None of the identified studies was a randomized, controlled trial. Most of them were observational, retrospective [17,18,19,20,21,22,23,24,25,26,27,28] or observational prospective [29,30,31,32] cohort studies. The vast majority were single-centre observations [17, 19,20,21, 23,24,25,26, 29, 30] with the exception of four dual/multicentre studies [18, 22, 28, 32] and two based on high volume registries (European survey [27] and United States National Database [28]). Four [26, 29, 31, 32] from the 16 studies proved to be high-quality reports (average MINORS score 11.4, Supplementary Table 2).
The most important published patient characteristics of the included studies, such as age, gender, aetiology, baseline QRS duration (paced in upgrade, intrinsic in de novo groups), baseline NYHA functional class, baseline left ventricular ejection fraction and dimensions are summarized in Supplementary Table 3. In summary, the mean ejection fraction was by definition lower than 35% in all studies, and there were no significant differences between the de novo and upgrade groups in most of the individual studies. Most of the trials enrolled patients with severe symptoms (NYHA III–IVa); a smaller extent of the studies investigated patients without depicting functional class. More than 50% of the studies found significant differences in the following baseline parameters between the two patient groups: age, atrial fibrillation and QRS duration. In the upgrade group, patients were generally older, more likely to have atrial fibrillation and they had wider (paced) QRS.
All-cause mortality and heart failure events
Crude mortality rates were available in 489,197 patients from 11 studies [17, 19, 21, 22, 24, 26,27,28,29, 31, 32], while unadjusted or adjusted hazard ratios were available for 1734 and 1229 patients in 4 [19, 26, 31, 32] and 3 [19, 31, 32] studies, respectively. All-cause mortality did not differ following upgrade compared to de novo implantations (RR 1.19, 95% CI 0.88 to 1.60, p = 0.27, I 2 = 90.1%, Fig. 2). Pooled analyses of the unadjusted or adjusted hazard ratios revealed similar findings (crude HR 1.07, 95% CI 0.72 to 1.57, p = 0.74, I 2 = 73.6%, Supplementary Fig. 1a) (adjusted HR 0.81, 95% CI 0.36 to 1.81, p = 0.61, I 2 = 88.5%, Supplementary Fig. 1b).
When only prospective studies were analysed, no differences were found between the two groups (RR 1.10, 95% CI 0.76 to 1.60, p = 0.60, I 2 = 54.0%, Supplementary Fig. 1c).
In studies providing appropriate information, the unadjusted risk of heart failure was also similar in de novo and upgrade CRT groups (RR 0.96, 95% CI 0.70 to 1.32, p = 0.81, I 2 = 28.0%, Fig. 3).
Left ventricular reverse remodelling, clinical improvement
The extent of reverse remodelling in terms of improvement in left ventricular ejection fraction and end-diastolic volume was similar in the two patient groups (ΔEF de novo − 6.85% vs. upgrade − 9.35%, p = 0.235; ΔEDV de novo − 23.0 vs. upgrade − 20.0 ml; p = 0.730) (Fig. 4a, b). Regarding symptoms, change in NYHA functional class was also comparable after de novo CRT implantation and upgrade procedures (ΔNYHA de novo − 0.74 vs. upgrade − 0.70 class; p = 0.737) (Fig. 5). When QRS narrowing was compared, no significant difference was found between the two patient groups (ΔQRS de novo − 9.6 vs. upgrade − 29.5 ms; p = 0.485) (Fig. 5b).
System-related complications
Based on four studies [24, 27,28,29], where detailed analyses regarding system-related complications were published, fluoroscopic time [27], the rate of phrenic nerve stimulation [24], cardiac perforation, pneumothorax and lead dislocation [28] showed significant difference between the two patient groups (Table 2). In the largest database [28], the most severe complications such as lead revision, pneumothorax or perforation were observed more frequently in the upgrade group.
Another prospective, multicentre registry which was designed to demonstrate complication rates in patients with 6 months after pacemaker or ICD replacement has to be mentioned; however due to its study design, it was not eligible for including in the current analyses [33]. In this registry [33], 713 patients were upgraded, and the most frequent major complication was lead dislodgement or malfunction observed in 7.9% of patients, while 1.5% experienced haematoma and 0.8% infection in the first 6 months after the procedure.
Publication bias
According to the rank correlation test of Begg and Mazumdar, there was no evidence of significant publication bias (mortality RR: τ = − 0.236, p = 0.312; mortality RR in prospective trials: τ = − 0.167, p = 0.734; mortality crude HR: τ = − 0.167, p = 0.734; mortality adjusted HR: τ = 0.333, p = 0.602; HF RR: τ = 0, p = 1.000). Furthermore, corresponding to the Duval and Tweedie’s trim and fill input method, there was no evidence that publication bias would significantly impact on the overall effect sizes observed (Supplementary Figs. 2–6).
Discussion
Main findings
This systematic review of 16 studies comparing data in approximately 500,000 patients undergoing de novo or upgrade CRT implantations revealed no significant difference in all-cause mortality or heart failure events between the two patient groups. Also, no significant differences were found in changes of echocardiographic parameters of reverse remodelling (EF, EDV). Functional changes (i.e. improvement of NYHA functional class) and narrowing of QRS were also similar, suggesting that adding left ventricular pacing in patients with prior cardiac devices may be a safe and feasible procedure with similar clinical benefits as de novo implantations.
Patient population referred to biventricular upgrade
Biventricular upgrade affects roughly 5–10% of patients who underwent ICD or pacemaker implantation [33, 34]. Due to the right ventricular (RV) pacing-induced dyssynchrony, patients with a high percentage of RV pacing are at high risk of adverse clinical outcomes [2, 3] and could become candidates for CRT upgrade. Wilkoff et al. demonstrated in the DAVID trial that the percent of RV pacing correlated with the composite of death or rehospitalizations for HF in ICD recipients with a high rate of DDD pacing compared to patients with the VVI 40/min programming [3]. In addition, echocardiographic and functional parameters (6-min walk test, symptoms) may worsen even in patients with previously preserved ejection fraction [35, 36] or mild heart failure [37] after frequent RV pacing. In the BLOCK-HF [37] trial, patients with atrioventricular (AV) block, mild symptoms (NYHA II–III) and HFmrEF or HFrEF (EF < 50%, the baseline mean EF = 45%) received a CRT device and were randomly assigned to standard right ventricular or biventricular pacing. The primary endpoint (composite of all-cause mortality, HF events, or ≥ 15% increase in LVESV index) occurred in 190 of 342 patients (55.6%) in the RV pacing group, compared to 160 of 349 patients (45.8%) in the CRT group, which first demonstrated the superiority of biventricular pacing over RV pacing in pacemaker-dependent patients.
According to these lines of evidences and considerations, it seems reasonable upgrading to CRT in HF patients with previously implanted cardiac devices and a high percentage of right ventricular pacing. On the other hand, upgrade procedures may be associated with higher surgical risk, such as venous access issues, the risk of damage or extraction of previously implanted leads, higher infection rates and longer procedure times [33, 38], that all together may significantly compromise the success of LV pacing.
It should be also noted that aetiology or the cause of decreased ejection fraction might be different in upgrade vs. de novo CRT groups. Regarding the aetiology, similar percentage of ischemic and non-ischemic heart disease was reported in most of the included studies; however, the baseline QRS was wider (paced QRS), and patients were older and had more often atrial fibrillation in the upgrade group.
Evidence supporting CRT upgrade
The current guideline recommendations are mainly based on some non-randomized, observational prospective “upgrade vs. de novo” studies, which are included in the current analysis [17, 18, 23, 27, 30]. In addition, small observational retrospective [39,40,41,42,43,44,45] and cross-over [46,47,48,49] trials are also referred in the ESC guidelines with a low number of patients.
In most of these trials, only soft endpoints, such as NYHA functional class, 6-min walk test, quality of life or echocardiographic parameters were analysed. Summarizing the most frequently investigated clinical parameters, such as change in NYHA functional class, decrease in QRS duration, changes of left ventricular ejection fraction and end-diastolic volume, no significant differences were observed between the de novo and upgrade groups in our analysis.
Data regarding long-term mortality were reported only in a few prior trials [17, 19, 21, 22, 24, 26,27,28,29, 31, 32]. The largest report from these was the European Cardiac Resynchronization Survey [27] from 2011 comprising 1489 de novo and 601 upgrade CRT patients. Total mortality at 1 year was low and similar in both groups (8.6 vs. 7.9%, p = 0.57). Although this registry showed representative data about mortality rates with high number of enrolled patients, there are a huge number of potential confounders that may have biased the overall results. Therefore, trials with adjusted analyses are essential to control baseline differences to better assess the effects of CRT upgrade on long-term survival. In the current meta-analysis, three observational studies with adjusted all-cause mortality endpoints were included. Tayal et al. compared 85 patients who underwent de novo CRT implantation and 50 patients with CRT upgrade [31]. During the 4 years of follow-up time, patients with prior right ventricular pacing had a significantly lower risk of fatal events than patients with de novo CRT implantation (adjusted HR 0.25, 95% CI 0.07–0.88, P = 0.03). Gage et al. compared 190 patients with prior high percentage of right ventricular pacing (> 40%) to 465 non-paced patients who underwent CRT implantation [19]. During the median follow-up of 4.2 years, upgrade patients tended to have better outcomes in terms of all-cause mortality (adjusted HR 0.73; 95% CI 0.53–1.01; p = 0.055). In contrast, Vamos et al. recently reported a higher risk for mortality in the upgrade group when compared to de novo implantation in 552 patients [32]. In this multicentre study with a mean follow-up of 37 months, patients who underwent CRT upgrade had a significantly higher risk of all-cause mortality compared to patients with de novo implantations even after adjusting for potential confounders with multivariate Cox regression analysis (adjusted HR 1.68, 95% CI 1.20–2.34, p = 0.002) and after applying propensity score matching (PS-adjusted HR 1.79, 95% CI 1.08–2.95, p = 0.023). Summarizing all these results in our meta-analysis, a similar long-term survival was found between the two patient groups. However, heterogeneities in the results of adjusted studies largely emphasize that randomized controlled trials are needed to objectively clarify this clinical dilemma.
Besides the aforementioned publications until 2016, there is another manuscript released in 2017 which has to be discussed more in details. Cheung et al. recently published a unique data using the US National Database between 2003 and 2013 including 19,546 patients who underwent CRT upgrade vs. 464,246 patients after de novo CRT implantations [28], which was also included in the current analysis. This study found that patients with de novo CRT implantation were older, had more frequent third-degree AV block, LBBB or other comorbidities such as renal failure or ischemic heart disease. The rate of in-hospital mortality of patients undergoing CRT upgrade was significantly higher than in the de novo group (1.9 vs. 0.8%; p < 0.001). Regarding complications, significantly higher rate of pneumothorax, lead revision or perforation were observed in the upgrade group. These results are somewhat different from other trials included in our meta-analysis, where patients undergoing CRT upgrade were generally older and had more frequent atrial fibrillation. Despite potential differences in the lengths of follow-up and baseline patient characteristics, other studies did not reveal a higher risk for mortality, such as the twofold higher risk in the US cohort. This pronounced in-hospital mortality rate might be derived from a de-identified, code-based selection of their database which may not have been representative for the total patient cohort dedicated for CRT upgrade.
Despite the current detailed review and meta-analysis of the available clinical evidence, several questions remain unanswered. Most striking from these include which populations may derive the largest benefits from upgrading and what is the optimal timing for such procedures.
The ongoing BUDAPEST-CRT Upgrade study (NCT02270840) was designed to evaluate the efficacy and safety of CRT upgrade from conventional PM or ICD systems [50]. In this prospective, randomized, multicentre clinical trial symptomatic heart failure patients (NYHA II–IVa) with low ejection fraction (EF ≤ 35%), intermittent (≥ 20%) or permanent right ventricular pacing and wide paced QRS (≥ 150 ms) are randomized to CRT-D or ICD. Based on the primary composite endpoint of all-cause mortality, heart failure events and less than 15% end-systolic volume reduction at 12-month follow-up, we will obtain more definite data on the risks and benefits of CRT upgrade procedures.
Limitations
This meta-analysis shows all potential limitations of such a kind of analysis. Patients in the two groups were not randomly allocated; all included studies were either retrospective studies with historical controls or prospective observational data collections; thus, a residual selection bias could not be excluded. There are remaining clinical issues that have obviously affected the decision-making on upgrading but could not be collected and analysed in a systematic fashion, such as the possibility to avoid RV stimulation by programming appropriately, the patency of the venous system, need for generator or lead replacement due to battery or lead issues and end-stage renal disease on dialysis or other severe comorbidities including age. Second, the comparison of these two groups is partly confusing, while the aetiology of dyssynchrony may be different. In recipients of “de novo” CRT, other underlying cardiac pathophysiological conditions in addition to the initial dyssynchrony may be present, whereas in the upgrade group, patients were initially implanted with a pacemaker for a bradycardia indication. Third, we did not have access to individual patient-level data precluding us from calculating adjusted hazard ratios for all the included studies. Finally, the length of follow-up was also heterogeneous in the included reports. However, so far, this is the largest available comprehensive evidence in this respect, and sensitivity analysis from adjusted results corroborated our initial findings.
Conclusions
Our systematic review and meta-analysis of currently available studies reports that CRT upgrade is associated with similar risk for all-cause mortality compared to de novo resynchronization therapy. Benefits on reverse remodelling and functional capacity improved similarly in both groups suggesting that CRT upgrade may be safely and effectively offered in routine practice. These results should be confirmed in further randomized clinical trials.
Abbreviations
- CI:
-
Confidence interval
- CRT:
-
Cardiac resynchronization therapy
- EDV:
-
End-diastolic volume
- ESV:
-
End-systolic volume
- HF:
-
Heart failure
- HFrEF:
-
Heart failure with reduced ejection fraction
- HFmrEF:
-
Heart failure with mid-range ejection fraction
- HR:
-
Hazard ratio
- LVEF:
-
Left ventricular ejection fraction
- ICD:
-
Implantable cardioverter defibrillator
- LBBB:
-
Left bundle branch block
- NYHA:
-
New York Heart Association Functional Class
- RR:
-
Risk ratio
- VF:
-
Ventricular fibrillation
References
Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, Estes NA 3rd, Foster E, Greenberg H, Higgins SL, Pfeffer MA, Solomon SD, Wilber D, Zareba W (2009) Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med 361(14):1329–1338. https://doi.org/10.1056/NEJMoa0906431
Sweeney MO, Hellkamp AS, Ellenbogen KA, Greenspon AJ, Freedman RA, Lee KL, Lamas GA (2003) Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation 107(23):2932–2937. https://doi.org/10.1161/01.cir.0000072769.17295.b1
Wilkoff BL, Cook JR, Epstein AE, Greene HL, Hallstrom AP, Hsia H, Kutalek SP, Sharma A (2002) Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator: the Dual Chamber and VVI Implantable Defibrillator (DAVID) Trial. JAMA 288(24):3115–3123
Birnie DH, Ha A, Higginson L, Sidhu K, Green M, Philippon F, Thibault B, Wells G, Tang A (2013) Impact of QRS morphology and duration on outcomes after cardiac resynchronization therapy: results from the Resynchronization-Defibrillation for Ambulatory Heart Failure Trial (RAFT). Circ Heart Fail 6(6):1190–1198. https://doi.org/10.1161/circheartfailure.113.000380
Zareba W, Klein H, Cygankiewicz I, Hall WJ, McNitt S, Brown M, Cannom D, Daubert JP, Eldar M, Gold MR, Goldberger JJ, Goldenberg I, Lichstein E, Pitschner H, Rashtian M, Solomon S, Viskin S, Wang P, Moss AJ (2011) Effectiveness of cardiac resynchronization therapy by QRS morphology in the Multicenter Automatic Defibrillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT). Circulation 123(10):1061–1072. https://doi.org/10.1161/circulationaha.110.960898
Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA, Cleland J, Deharo JC, Delgado V, Elliott PM, Gorenek B, Israel CW, Leclercq C, Linde C, Mont L, Padeletti L, Sutton R, Vardas PE, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Kirchhof P, Blomstrom-Lundqvist C, Badano LP, Aliyev F, Bansch D, Baumgartner H, Bsata W, Buser P, Charron P, Daubert JC, Dobreanu D, Faerestrand S, Hasdai D, Hoes AW, Le Heuzey JY, Mavrakis H, McDonagh T, Merino JL, Nawar MM, Nielsen JC, Pieske B, Poposka L, Ruschitzka F, Tendera M, Van Gelder IC, Wilson CM (2013) 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J 34(29):2281–2329. https://doi.org/10.1093/eurheartj/eht150
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27):2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62(16):e147–e239. https://doi.org/10.1016/j.jacc.2013.05.019
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clin Res ed) 339:b2700. https://doi.org/10.1136/bmj.b2700
Merkely B, Kosztin A, Vamos M (2016) De novo implantation vs. upgrade of cardiac resynchronization therapy: a systematic review and meta-analysis. PROSPERO 2016:CRD42016043747. Available from http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016043747. Accessed 29 July 2016
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. https://doi.org/10.1002/sim.1186
Borenstein M, Higgins JP (2013) Meta-analysis and subgroups. Prev Sci: Off J Soc Prev Res 14(2):134–143. https://doi.org/10.1007/s11121-013-0377-7
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2009) Introduction to meta-analysis, 1st edn. John Wiley & Sons, Ltd., Pondicherry
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Vamos M, Cappato R, Marchlinski FE, Natale A, Hohnloser SH (2016) Efficacy and safety of rivaroxaban compared with vitamin K antagonists for peri-procedural anticoagulation in catheter ablation of atrial fibrillation: a systematic review and meta-analysis. Europace : European Pacing Arrhythmias Card Electrophysiol: J Work Groups Card Pacing Arrhythmias Card Cell Electrophysiol Eur Soc Cardiol 18(12):1787–1794. https://doi.org/10.1093/europace/euv408
Foley PW, Muhyaldeen SA, Chalil S, Smith RE, Sanderson JE, Leyva F (2009) Long-term effects of upgrading from right ventricular pacing to cardiac resynchronization therapy in patients with heart failure. Europace : Eur Pacing Arrhythmias Card Electrophysiol: J Work Groups Card Pacing Arrhythmias Card Cell Electrophysiol Eur Soc Cardiol 11(4):495–501. https://doi.org/10.1093/europace/eup037
Frohlich G, Steffel J, Hurlimann D, Enseleit F, Luscher TF, Ruschitzka F, Abraham WT, Holzmeister J (2010) Upgrading to resynchronization therapy after chronic right ventricular pacing improves left ventricular remodelling. Eur Heart J 31(12):1477–1485. https://doi.org/10.1093/eurheartj/ehq065
Gage RM, Burns KV, Bank AJ (2014) Echocardiographic and clinical response to cardiac resynchronization therapy in heart failure patients with and without previous right ventricular pacing. Eur J Heart Fail 16(11):1199–1205. https://doi.org/10.1002/ejhf.143
Kabutoya T, Mitsuhashi T, Hata Y, Hashimoto T, Nakagami R, Osada J, Watanabe T, Shimada K, Kario K (2010) Beneficial effects of upgrading from right ventricular pacing to cardiac resynchronization therapy in patients with heart failure compared to de novo cardiac resynchronization therapy. J Arrhythmia 22(1):16–20. https://doi.org/10.1016/S1880-4276(10)80031-6
Lipar L, Srivathsan K, Scott LR (2016) Short-term outcome of cardiac resynchronization therapy—a comparison between newly implanted and chronically right ventricle-paced patients. Int J Cardiol 219:195–199. https://doi.org/10.1016/j.ijcard.2016.06.054
Nagele H, Dodeck J, Behrens S, Azizi M, Hashagen S, Eisermann C, Castel MA (2008) Hemodynamics and prognosis after primary cardiac resynchronization system implantation compared to “upgrade” procedures. Pacing Clin Electrophysiol: PACE 31(10):1265–1271. https://doi.org/10.1111/j.1540-8159.2008.01176.x
Paparella G, Sciarra L, Capulzini L, Francesconi A, De Asmundis C, Sarkozy A, Cazzin R, Brugada P (2010) Long-term effects of upgrading to biventricular pacing: differences with cardiac resynchronization therapy as primary indication. Pacing Clin Electrophysiol: PACE 33(7):841–849. https://doi.org/10.1111/j.1540-8159.2010.02701.x
Ter Horst IA, Kuijpers Y, van’t Sant J, Tuinenburg AE, Cramer MJ, Meine M (2016) “Are CRT upgrade procedures more complex and associated with more complications than de novo CRT implantations?” A single centre experience. Neth Heart J: Monthly J Neth Soc Cardiol Neth Heart Found 24(1):75–81. https://doi.org/10.1007/s12471-015-0771-9
Witte KK, Pipes RR, Nanthakumar K, Parker JD (2006) Biventricular pacemaker upgrade in previously paced heart failure patients—improvements in ventricular dyssynchrony. J Card Fail 12(3):199–204. https://doi.org/10.1016/j.cardfail.2005.12.003
Wokhlu A, Rea RF, Asirvatham SJ, Webster T, Brooke K, Hodge DO, Wiste HJ, Dong Y, Hayes DL, Cha YM (2009) Upgrade and de novo cardiac resynchronization therapy: impact of paced or intrinsic QRS morphology on outcomes and survival. Heart Rhythm : Off J Heart Rhythm Soc 6(10):1439–1447. https://doi.org/10.1016/j.hrthm.2009.07.009
Bogale N, Witte K, Priori S, Cleland J, Auricchio A, Gadler F, Gitt A, Limbourg T, Linde C, Dickstein K (2011) The European Cardiac Resynchronization Therapy Survey: comparison of outcomes between de novo cardiac resynchronization therapy implantations and upgrades. Eur J Heart Fail 13(9):974–983. https://doi.org/10.1093/eurjhf/hfr085
Cheung JW, Ip JE, Markowitz SM, Liu CF, Thomas G, Feldman DN, Swaminathan RV, Lerman BB, Kim LK (2017) Trends and outcomes of cardiac resynchronization therapy upgrade procedures: a comparative analysis using a United States National Database 2003-2013. Heart Rhythm : Off J Heart Rhythm Soc. https://doi.org/10.1016/j.hrthm.2017.02.017
Duray GZ, Israel CW, Pajitnev D, Hohnloser SH (2008) Upgrading to biventricular pacing/defibrillation systems in right ventricular paced congestive heart failure patients: prospective assessment of procedural parameters and response rate. Europace : Eur Pacing Arrhythmias Card Electrophysiol: J Work Groups Card Pacing Arrhythmias Card Cell Electrophysiol Eur Soc Cardiol 10(1):48–52. https://doi.org/10.1093/europace/eum259
Marai I, Gurevitz O, Carasso S, Nof E, Bar-Lev D, Luria D, Arbel Y, Freimark D, Feinberg MS, Eldar M, Glikson M (2006) Improvement of congestive heart failure by upgrading of conventional to resynchronization pacemakers. Pacing Clin Electrophysiol: PACE 29(8):880–884. https://doi.org/10.1111/j.1540-8159.2006.00455.x
Tayal B, Gorcsan J 3rd, Delgado-Montero A, Goda A, Ryo K, Saba S, Risum N, Sogaard P (2016) Comparative long-term outcomes after cardiac resynchronization therapy in right ventricular paced patients versus native wide left bundle branch block patients. Heart Rhythm: Off J Heart Rhythm Soc 13(2):511–518. https://doi.org/10.1016/j.hrthm.2015.11.001
Vamos M, Erath JW, Bari Z, Vagany D, Linzbach SP, Burmistrava T, Israel CW, Duray GZ, Hohnloser SH (2017) Effects of upgrade versus de novo cardiac resynchronization therapy on clinical response and long-term survival: results from a multicenter study. Circ Arrhythmia Electrophysiol 10(2):e004471. https://doi.org/10.1161/circep.116.004471
Poole JE, Gleva MJ, Mela T, Chung MK, Uslan DZ, Borge R, Gottipaty V, Shinn T, Dan D, Feldman LA, Seide H, Winston SA, Gallagher JJ, Langberg JJ, Mitchell K, Holcomb R (2010) Complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures: results from the REPLACE registry. Circulation 122(16):1553–1561. https://doi.org/10.1161/circulationaha.110.976076
Scott IC, Masri B, D’Amico LA, Jin SW, Jungblut B, Wehman AM, Baier H, Audigier Y, Stainier DY (2007) The g protein-coupled receptor agtrl1b regulates early development of myocardial progenitors. Dev Cell 12(3):403–413. https://doi.org/10.1016/j.devcel.2007.01.012
Doshi RN, Daoud EG, Fellows C, Turk K, Duran A, Hamdan MH, Pires LA (2005) Left ventricular-based cardiac stimulation post AV nodal ablation evaluation (the PAVE study). J Cardiovasc Electrophysiol 16(11):1160–1165. https://doi.org/10.1111/j.1540-8167.2005.50062.x
Yu CM, Chan JY, Zhang Q, Omar R, Yip GW, Hussin A, Fang F, Lam KH, Chan HC, Fung JW (2009) Biventricular pacing in patients with bradycardia and normal ejection fraction. N Engl J Med 361(22):2123–2134. https://doi.org/10.1056/NEJMoa0907555
Curtis AB, Worley SJ, Adamson PB, Chung ES, Niazi I, Sherfesee L, Shinn T, Sutton MS (2013) Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med 368(17):1585–1593. https://doi.org/10.1056/NEJMoa1210356
Kirkfeldt RE, Johansen JB, Nohr EA, Jorgensen OD, Nielsen JC (2014) Complications after cardiac implantable electronic device implantations: an analysis of a complete, nationwide cohort in Denmark. Eur Heart J 35(18):1186–1194. https://doi.org/10.1093/eurheartj/eht511
Baker CM, Christopher TJ, Smith PF, Langberg JJ, Delurgio DB, Leon AR (2002) Addition of a left ventricular lead to conventional pacing systems in patients with congestive heart failure: feasibility, safety, and early results in 60 consecutive patients. Pacing Clin Electrophysiol: PACE 25(8):1166–1171
Eldadah ZA, Rosen B, Hay I, Edvardsen T, Jayam V, Dickfeld T, Meininger GR, Judge DP, Hare J, Lima JB, Calkins H, Berger RD (2006) The benefit of upgrading chronically right ventricle-paced heart failure patients to resynchronization therapy demonstrated by strain rate imaging. Heart Rhythm: Off J Heart Rhythm Soc 3(4):435–442. https://doi.org/10.1016/j.hrthm.2005.12.003
Laurenzi F, Achilli A, Avella A, Peraldo C, Orazi S, Perego GB, Cesario A, Valsecchi S, De Santo T, Puglisi A, Tondo C (2007) Biventricular upgrading in patients with conventional pacing system and congestive heart failure: results and response predictors. Pacing Clin Electrophysiol: PACE 30(9):1096–1104. https://doi.org/10.1111/j.1540-8159.2007.00819.x
Leon AR, Greenberg JM, Kanuru N, Baker CM, Mera FV, Smith AL, Langberg JJ, DeLurgio DB (2002) Cardiac resynchronization in patients with congestive heart failure and chronic atrial fibrillation: effect of upgrading to biventricular pacing after chronic right ventricular pacing. J Am Coll Cardiol 39(8):1258–1263
Shimano M, Tsuji Y, Yoshida Y, Inden Y, Tsuboi N, Itoh T, Suzuki H, Muramatsu T, Okada T, Harata S, Yamada T, Hirayama H, Nattel S, Murohara T (2007) Acute and chronic effects of cardiac resynchronization in patients developing heart failure with long-term pacemaker therapy for acquired complete atrioventricular block. Europace : Eur Pacing Arrhythmias Card Electrophysiol : J Work Groups Card Pacing Arrhythmias Card Cell Electrophysiol Eur Soc Cardiol 9(10):869–874. https://doi.org/10.1093/europace/eum119
Valls-Bertault V, Fatemi M, Gilard M, Pennec PY, Etienne Y, Blanc JJ (2004) Assessment of upgrading to biventricular pacing in patients with right ventricular pacing and congestive heart failure after atrioventricular junctional ablation for chronic atrial fibrillation. Europace : Eur Pacing Arrhythmias Card Electrophysiol : J Work Groups Card Pacing Arrhythmias Card Cell Electrophysiol Eur Soc Cardiol 6(5):438–443. https://doi.org/10.1016/j.eupc.2004.04.004
Vatankulu MA, Goktekin O, Kaya MG, Ayhan S, Kucukdurmaz Z, Sutton R, Henein M (2009) Effect of long-term resynchronization therapy on left ventricular remodeling in pacemaker patients upgraded to biventricular devices. Am J Cardiol 103(9):1280–1284. https://doi.org/10.1016/j.amjcard.2009.01.023
Delnoy PP, Ottervanger JP, Vos DH, Elvan A, Misier AR, Beukema WP, Steendijk P, van Hemel NM (2011) Upgrading to biventricular pacing guided by pressure-volume loop analysis during implantation. J Cardiovasc Electrophysiol 22(6):677–683. https://doi.org/10.1111/j.1540-8167.2010.01968.x
Hoijer CJ, Meurling C, Brandt J (2006) Upgrade to biventricular pacing in patients with conventional pacemakers and heart failure: a double-blind, randomized crossover study. Europace : Eur Pacing Arrhythmias Card Electrophysiol: J Work Groups Card Pacing Arrhythmias Card Cell Electrophysiol Eur Soc Cardiol 8(1):51–55. https://doi.org/10.1093/europace/euj014
Leclercq C, Cazeau S, Lellouche D, Fossati F, Anselme F, Davy JM, Sadoul N, Klug D, Mollo L, Daubert JC (2007) Upgrading from single chamber right ventricular to biventricular pacing in permanently paced patients with worsening heart failure: the RD-CHF study. Pacing Clin Electrophysiol: PACE 30(Suppl 1):S23–S30. https://doi.org/10.1111/j.1540-8159.2007.00598.x
van Geldorp IE, Vernooy K, Delhaas T, Prins MH, Crijns HJ, Prinzen FW, Dijkman B (2010) Beneficial effects of biventricular pacing in chronically right ventricular paced patients with mild cardiomyopathy. Europace : Eur Pacing Arrhythmias Card Electrophysiol: J Work Groups Card Pacing Arrhythmias Card Cell Electrophysiol Eur Soc Cardiol 12(2):223–229. https://doi.org/10.1093/europace/eup378
Merkely B, Kosztin A, Roka A, Geller L, Zima E, Kovacs A, Boros AM, Klein H, Wranicz JK, Hindricks G, Clemens M, Duray GZ, Moss AJ, Goldenberg I, Kutyifa V (2016) Rationale and design of the BUDAPEST-CRT Upgrade Study: a prospective, randomized, multicentre clinical trial. Europace : Eur Pacing Arrhythmias Card Electrophysiol: J Work Groups Card Pacing Arrhythmias Card Cell Electrophysiol Eur Soc Cardiol. https://doi.org/10.1093/europace/euw193
Funding
This study was supported by the National Research, Development and Innovation Office (NKFIH) of Hungary (NVKP_16-1-2016-0017 to B. M.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mate Vamos reports lecture fees from Bayer, Pfizer and Spectranetics and support attending scientific meetings from Bayer, Boston Scientific, Pfizer and SJM, outside the submitted work. Endre Zima reports consulting fees and honoraria from Bayer, Biotronik, Boston Scientific, Innomed, Medtronic and St. Jude Medical for lectures, training and participation in clinical trials. Laszlo Geller reports consulting fees/honoraria from Biotronik, Medtronic, St. Jude Medical and Johnson & Johnson. Gabor Z. Duray served as a member of the steering committee of the Micra Study and reports research grants from Boston Scientific, Biotronik and Medtronic and speakers bureau/consulting fees from Biotronik, Medtronic, St. Jude Medical, Bayer and Boehringer Ingelheim. Bela Merkely reports consulting/lecture fees from Biotronik, Boston Scientific, Medtronic, St. Jude Medical and Terumo.
Annamaria Kosztin, Daniel Aradi, Attila Kovacs, Richard Schwertner, Valentina Kutyifa and Klaudia Vivien Nagy have nothing to disclose.
Electronic supplementary material
ESM 1
(DOCX 4.53 mb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kosztin, A., Vamos, M., Aradi, D. et al. De novo implantation vs. upgrade cardiac resynchronization therapy: a systematic review and meta-analysis. Heart Fail Rev 23, 15–26 (2018). https://doi.org/10.1007/s10741-017-9652-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-017-9652-1