Abstract
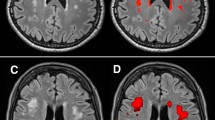
Most studies of white matter hyperintensity volume (WMHV) in stroke patients lack reliable information on antecedent exposure to vascular risk factors. By leveraging prospective cohort data, we explored associations between lifestyle and health factors assessed 1 year prior to stroke and WMHV in individuals who experienced an ischemic stroke. This analysis was nested within two large prospective studies of initially healthy individuals. Information on lifestyle factors and health conditions was collected prior to the stroke event through annual or biannual questionnaires. For individuals who experienced their first confirmed ischemic stroke and had available magnetic resonance imaging, we measured WMHV using a validated semiautomated method. Linear regression was used to explore associations between lifestyle factors and health conditions and log-transformed WMHV. We measured WMHV in 345 participants with a first ischemic stroke event (mean age = 74.4 years; 24.9% male). After multivariate adjustment, history of diabetes was associated with decreased WMHV (p value = 0.06) while history of transient ischemic attack (p value = 0.09) and hypertension (p value = 0.07) were associated with increased WMHV. Most lifestyle factors and health conditions measured 1 year prior to stroke were not associated with WMHV measured at the time of ischemic stroke. Future studies could examine whether long term exposure to these factors impacts diffuse microvascular ischemic brain injury among stroke patients.

Similar content being viewed by others
References
Henon H, Vroylandt P, Durieu I, Pasquier F, Leys D. Leukoaraiosis more than dementia is a predictor of stroke recurrence. Stroke. 2003;34(12):2935–40. https://doi.org/10.1161/01.STR.0000103747.58719.59.
Arsava EM, Rahman R, Rosand J, et al. Severity of leukoaraiosis correlates with clinical outcome after ischemic stroke. Neurology. 2009;72(16):1403–10. https://doi.org/10.1212/WNL.0b013e3181a18823.
Kissela B, Lindsell CJ, Kleindorfer D, et al. Clinical prediction of functional outcome after ischemic stroke: the surprising importance of periventricular white matter disease and race. Stroke. 2009;40(2):530–6. https://doi.org/10.1161/STROKEAHA.108.521906.
Breteler MM, van Swieten JC, Bots ML, et al. Cerebral white matter lesions, vascular risk factors, and cognitive function in a population-based study: the Rotterdam Study. Neurology. 1994;44(7):1246–52.
Jeerakathil T, Wolf PA, Beiser A, et al. Stroke risk profile predicts white matter hyperintensity volume: the Framingham Study. Stroke. 2004;35(8):1857–61. https://doi.org/10.1161/01.STR.0000135226.53499.85.
Liao D, Cooper L, Cai J, et al. Presence and severity of cerebral white matter lesions and hypertension, its treatment, and its control. The ARIC Study. Atherosclerosis Risk in Communities Study. Stroke. 1996;27(12):2262–70.
Torres ER, Strack EF, Fernandez CE, Tumey TA, Hitchcock ME. Physical activity and white matter hyperintensities: a systematic review of quantitative studies. Prev Med Rep. 2015;2:319–25. https://doi.org/10.1016/j.pmedr.2015.04.013.
Williamson W, Lewandowski AJ, Forkert ND, et al. Association of Cardiovascular Risk Factors with MRI indices of cerebrovascular structure and function and white matter hyperintensities in young adults. JAMA. 2018;320(7):665–73. https://doi.org/10.1001/jama.2018.11498.
Cloonan L, Fitzpatrick KM, Kanakis AS, Furie KL, Rosand J, Rost NS. Metabolic determinants of white matter hyperintensity burden in patients with ischemic stroke. Atherosclerosis. 2015;240(1):149–53. https://doi.org/10.1016/j.atherosclerosis.2015.02.052.
Jimenez-Conde J, Biffi A, Rahman R, et al. Hyperlipidemia and reduced white matter hyperintensity volume in patients with ischemic stroke. Stroke. 2010;41(3):437–42. https://doi.org/10.1161/STROKEAHA.109.563502.
Zhang CR, Cloonan L, Fitzpatrick KM, et al. Determinants of white matter hyperintensity burden differ at the extremes of ages of ischemic stroke onset. J Stroke Cerebrovasc Dis. 2015;24(3):649–54. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.10.016.
Manson JE, Bassuk SS, Lee IM, et al. The VITamin D and OmegA-3 TriaL (VITAL): rationale and design of a large randomized controlled trial of vitamin D and marine omega-3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease. Contemp Clin Trials. 2012;33(1):159–71. https://doi.org/10.1016/j.cct.2011.09.009.
Lee IM, Cook NR, Gaziano JM, et al. Vitamin E in the primary prevention of cardiovascular disease and cancer: the Women’s Health Study: a randomized controlled trial. JAMA. 2005;294(1):56–65. https://doi.org/10.1001/jama.294.1.56.
Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352(13):1293–304. https://doi.org/10.1056/NEJMoa050613.
Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41.
Irizarry MC, Gurol ME, Raju S, et al. Association of homocysteine with plasma amyloid beta protein in aging and neurodegenerative disease. Neurology. 2005;65(9):1402–8. https://doi.org/10.1212/01.wnl.0000183063.99107.5c.
Rost NS, Rahman RM, Biffi A, et al. White matter hyperintensity volume is increased in small vessel stroke subtypes. Neurology. 2010;75(19):1670–7. https://doi.org/10.1212/WNL.0b013e3181fc279a.
Rost NS, Rahman R, Sonni S, et al. Determinants of white matter hyperintensity volume in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis. 2010;19(3):230–5. https://doi.org/10.1016/j.jstrokecerebrovasdis.2009.05.007.
Rost NS, Sadaghiani S, Biffi A, et al. Setting a gold standard for quantification of leukoaraiosis burden in patients with ischemic stroke: the Atherosclerosis Risk in Communities Study. J Neurosci Methods. 2014;221:196–201. https://doi.org/10.1016/j.jneumeth.2013.10.009.
Gurol ME, Irizarry MC, Smith EE, et al. Plasma beta-amyloid and white matter lesions in AD, MCI, and cerebral amyloid angiopathy. Neurology. 2006;66(1):23–9. https://doi.org/10.1212/01.wnl.0000191403.95453.6a.
Smith EE, Gurol ME, Eng JA, et al. White matter lesions, cognition, and recurrent hemorrhage in lobar intracerebral hemorrhage. Neurology. 2004;63(9):1606–12. https://doi.org/10.1212/01.wnl.0000142966.22886.20.
Nandigam RN, Chen YW, Gurol ME, Rosand J, Greenberg SM, Smith EE. Validation of intracranial area as a surrogate measure of intracranial volume when using clinical MRI. J Neuroimaging. 2007;17(1):74–7. https://doi.org/10.1111/j.1552-6569.2006.00069.x.
Ferguson KJ, Wardlaw JM, Edmond CL, Deary IJ, Maclullich AM. Intracranial area: a validated method for estimating intracranial volume. J Neuroimaging. 2005;15(1):76–8. https://doi.org/10.1177/1051228404270243.
Young VG, Halliday GM, Kril JJ. Neuropathologic correlates of white matter hyperintensities. Neurology. 2008;71(11):804–11. https://doi.org/10.1212/01.wnl.0000319691.50117.54.
Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S76–99. https://doi.org/10.1161/01.cir.0000437740.48606.d1.
Funding
This work was supported by the National Institutes of Health (CA047988, HL043851, HL080467, HL099355, CA182913, U01 CA138962, R01 CA138962 and HL128791).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rist, P.M., Buring, J.E., Rexrode, K.M. et al. Prospectively collected lifestyle and health information as risk factors for white matter hyperintensity volume in stroke patients. Eur J Epidemiol 34, 957–965 (2019). https://doi.org/10.1007/s10654-019-00546-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-019-00546-x