Abstract
Purpose
Understanding breast cancer mortality disparities by race and age is complex due to disease heterogeneity, comorbid disease, and the range of factors influencing access to care. It is important to understand how these factors group together within patients.
Methods
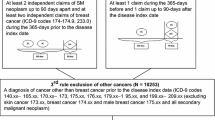
We compared socioeconomic status (SES) and comorbidity factors in the Carolina Breast Cancer Study Phase 3 (CBCS3, 2008–2013) to those for North Carolina using the 2010 Behavioral Risk Factor Surveillance Study. In addition, we used latent class analysis of CBCS3 data to identify covariate patterns by SES/comorbidities, barriers to care, and tumor characteristics and examined their associations with race and age using multinomial logistic regression.
Results
Major SES and comorbidity patterns in CBCS3 participants were generally similar to patterns in the state. Latent classes were identified for SES/comorbidities, barriers to care, and tumor characteristics that varied by race and age. Compared to white women, black women had lower SES (odds ratio (OR) 6.3, 95% confidence interval (CI) 5.2, 7.8), more barriers to care (OR 5.6, 95% CI 3.9, 8.1) and several aggregated tumor aggressiveness features. Compared to older women, younger women had higher SES (OR 0.5, 95% CI 0.4, 0.6), more barriers to care (OR 2.1, 95% CI 1.6, 2.9) and aggregated tumor aggressiveness features.
Conclusions
CBCS3 is representative of North Carolina on comparable factors. Patterns of access to care and tumor characteristics are intertwined with race and age, suggesting that interventions to address disparities will need to target both access and biology.



Similar content being viewed by others
References
DeSantis CE, Fedewa SA, Sauer AG, Kramer JL, Smith RA, Jemal A (2016) Breast cancer statistics, 2015: convergence of incidence rates between black and white women. CA Cancer J Clin 66(1):31–42. https://doi.org/10.3322/caac.21320
DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, Jemal A (2016) Cancer statistics for African Americans, 2016: progress and opportunities in reducing racial disparities. CA Cancer J Clin 66(4):290–308. https://doi.org/10.3322/caac.21340
National Center for Health Statistics, National Vital Statisitcs System Table 26 (2017) Death rates for malignant neoplasm of breast among females, by race, Hispanic origin and age: United States 2017. US Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, MD
Polyak K (2011) Heterogeneity in breast cancer. J Clin Investig 121(10):3786–3788. https://doi.org/10.1172/jci60534
Dunn BK, Agurs-Collins T, Browne D, Lubet R, Johnson KA (2010) Health disparities in breast cancer: biology meets socioeconomic status. Breast Cancer Res Treat 121(2):281–292. https://doi.org/10.1007/s10549-010-0827-x
Bergman LR, Mabnusson D, El-Khouri BM (2003) Studying individual development in an interindividual context: a person-oriented approach. Lawrence Erlbaum Associates, Mahwah, NJ
Rosner B, Colditz GA, Willett WC (1994) Reproductive risk factors in a prospective study of breast cancer: the Nurses' Health Study. Am J Epidemiol 139(8):819–835
Andaya AA, Enewold L, Horner MJ, Jatoi I, Shriver CD, Zhu K (2012) Socioeconomic disparities and breast cancer hormone receptor status. Cancer Causes Control 23(6):951–958. https://doi.org/10.1007/s10552-012-9966-1
Warner ET, Colditz GA, Palmer JR, Partridge AH, Rosner BA, Tamimi RM (2013) Reproductive factors and risk of premenopausal breast cancer by age at diagnosis: are there differences before and after age 40? Breast Cancer Res Treat 142(1):165–175. https://doi.org/10.1007/s10549-013-2721-9
Allott EH, Cohen SM, Geradts J, Sun X, Khoury T, Bshara W, Zirpoli GR, Miller CR, Hwang H, Thorne LB, O'Connor S, Tse CK, Bell MB, Hu Z, Li Y, Kirk EL, Bethea TN, Perou CM, Palmer JR, Ambrosone CB, Olshan AF, Troester MA (2016) Performance of three-biomarker immunohistochemistry for Intrinsic Breast Cancer Subtyping in the AMBER Consortium. Cancer Epidemiol Biomarkers Prev 25(3):470–478. https://doi.org/10.1158/1055-9965.epi-15-0874
Allott EH, Geradts J, Cohen SM, Khoury T, Zirpoli GR, Bshara W, Davis W, Omilian A, Nair P, Ondracek RP, Cheng TD, Miller CR, Hwang H, Thorne LB, O'Connor S, Bethea TN, Bell ME, Hu Z, Li Y, Kirk EL, Sun X, Ruiz-Narvaez EA, Perou CM, Palmer JR, Olshan AF, Ambrosone CB, Troester MA (2018) Frequency of breast cancer subtypes among African American women in the AMBER consortium. Breast Cancer Res 20(1):12. https://doi.org/10.1186/s13058-018-0939-5
PROC LCA, PROC LTA (Version 1.3.2) [Software] (2015) The Methodology Center, Penn State, University Park. https://methodology.psu.edu/.
Lanza ST, Collins LM, Lemmon DR, Schafer JL (2007) PROC LCA: a SAS procedure for latent class analysis. Struct Equ Model Multidiscip J 14(4):671–694
Hsu CD, Wang X, Habif DV Jr, Ma CX, Johnson KJ (2017) Breast cancer stage variation and survival in association with insurance status and sociodemographic factors in US women 18 to 64 years old. Cancer 123(16):3125–3131. https://doi.org/10.1002/cncr.30722
Mobley LR, Kuo TM, Clayton LJ, Evans WD (2009) Mammography facilities are accessible, so why is utilization so low? Cancer Causes Control 20(6):1017–1028. https://doi.org/10.1007/s10552-009-9295-1
Bigby J, Holmes MD (2005) Disparities across the breast cancer continuum. Cancer Causes Control 16(1):35–44. https://doi.org/10.1007/s10552-004-1263-1
Gerend MA, Pai M (2008) Social determinants of Black-White disparities in breast cancer mortality: a review. Cancer Epidemiol Biomarkers Prev 17(11):2913–2923. https://doi.org/10.1158/1055-9965.epi-07-0633
Parise CA, Caggiano V (2013) Disparities in race/ethnicity and socioeconomic status: risk of mortality of breast cancer patients in the California Cancer Registry, 2000–2010. BMC Cancer 13:449. https://doi.org/10.1186/1471-2407-13-449
Bradley CJ, Given CW, Roberts C (2002) Race, socioeconomic status, and breast cancer treatment and survival. J Natl Cancer Inst 94(7):490–496
Tammemagi CM (2007) Racial/ethnic disparities in breast and gynecologic cancer treatment and outcomes. Curr Opin Obstet Gynecol 19(1):31–36. https://doi.org/10.1097/GCO.0b013e3280117cf8
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371(9612):569–578. https://doi.org/10.1016/s0140-6736(08)60269-x
Munsell MF, Sprague BL, Berry DA, Chisholm G, Trentham-Dietz A (2014) Body mass index and breast cancer risk according to postmenopausal estrogen-progestin use and hormone receptor status. Epidemiol Rev 36:114–136. https://doi.org/10.1093/epirev/mxt010
Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL (2016) Trends in obesity among adults in the United States, 2005 to 2014. JAMA 315(21):2284–2291. https://doi.org/10.1001/jama.2016.6458
Connor Gorber S, Tremblay M, Moher D, Gorber B (2007) A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obesity Rev 8(4):307–326. https://doi.org/10.1111/j.1467-789X.2007.00347.x
Nawaz H, Chan W, Abdulrahman M, Larson D, Katz DL (2001) Self-reported weight and height: implications for obesity research. Am J Prev Med 20(4):294–298
Ashing-Giwa KT, Padilla G, Tejero J, Kraemer J, Wright K, Coscarelli A, Clayton S, Williams I, Hills D (2004) Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psycho-oncology 13(6):408–428. https://doi.org/10.1002/pon.750
Wheeler SB, Spencer JC, Pinheiro LC, Carey LA, Olshan AF, Reeder-Hayes KE (2018) Financial impact of breast cancer in black versus white women. J Clin Oncol 36(17):1695–1701. https://doi.org/10.1200/jco.2017.77.6310
DeSantis C, Jemal A, Ward E (2010) Disparities in breast cancer prognostic factors by race, insurance status, and education. Cancer Causes Control 21(9):1445–1450. https://doi.org/10.1007/s10552-010-9572-z
Anderson WF, Chatterjee N, Ershler WB, Brawley OW (2002) Estrogen receptor breast cancer phenotypes in the surveillance, epidemiology, and end results database. Breast Cancer Res Treat 76(1):27–36
Smith-Bindman R, Miglioretti DL, Lurie N, Abraham L, Barbash RB, Strzelczyk J, Dignan M, Barlow WE, Beasley CM, Kerlikowske K (2006) Does utilization of screening mammography explain racial and ethnic differences in breast cancer? Ann Intern Med 144(8):541–553
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, Karaca G, Troester MA, Tse CK, Edmiston S, Deming SL, Geradts J, Cheang MCU, Nielsen TO, Moorman PG, Earp HS, Millikan RC (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295(21):2492–2502. https://doi.org/10.1001/jama.295.21.2492
Dunnwald LK, Rossing MA, Li CI (2007) Hormone receptor status, tumor characteristics, and prognosis: a prospective cohort of breast cancer patients. Breast Cancer Res 9(1):R6. https://doi.org/10.1186/bcr1639
Daly B, Olopade OI (2015) A perfect storm: how tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J Clin 65(3):221–238. https://doi.org/10.3322/caac.21271
Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, Ghafoor A, Thun M (2004) Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin 54(2):78–93
Williams DR, Mohammed SA, Shields AE (2016) Understanding and effectively addressing breast cancer in African American women: unpacking the social context. Cancer 122(14):2138–2149. https://doi.org/10.1002/cncr.29935
Williams DR, Mohammed SA, Leavell J, Collins C (2010) Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci 1186:69–101. https://doi.org/10.1111/j.1749-6632.2009.05339.x
Tobacco use among US Racial/Ethnic Minority Groups‐Africian‐Americans, American Indians, and Alaska Natives, Asian‐Americans and Pacific Islanders, and Hispanics: a report of the surgeon general (1998)
Hill JO, Wyatt HR, Reed GW, Peters JC (2003) Obesity and the environment: where do we go from here? Science 299(5608):853–855. https://doi.org/10.1126/science.1079857
Akinyemiju TF, Pisu M, Waterbor JW, Altekruse SF (2015) Socioeconomic status and incidence of breast cancer by hormone receptor subtype. Springerplus 4:508. https://doi.org/10.1186/s40064-015-1282-2
Sineshaw HM, Gaudet M, Ward EM, Flanders WD, Desantis C, Lin CC, Jemal A (2014) Association of race/ethnicity, socioeconomic status, and breast cancer subtypes in the National Cancer Data Base (2010–2011). Breast Cancer Res Treat 145(3):753–763. https://doi.org/10.1007/s10549-014-2976-9
Messer LC, Laraia BA, Kaufman JS, Eyster J, Holzman C, Culhane J, Elo I, Burke JG, O'Campo P (2006) The development of a standardized neighborhood deprivation index. J Urban Health 83(6):1041–1062. https://doi.org/10.1007/s11524-006-9094-x
Palumbo A, Michael Y, Hyslop T (2016) Latent class model characterization of neighborhood socioeconomic status. Cancer Causes Control 27(3):445–452. https://doi.org/10.1007/s10552-015-0711-4
Acknowledgments
This work was supported by a Grant from the UNC Lineberger Comprehensive Cancer Center funded by the University Cancer Research Fund (LCCC2017T204), Susan G. Komen Graduate Training in Disparities Research, the National Cancer Institute of the National Institutes of Health (P50-CA58223, U01-CA179715, T32-CA057726), and the National Institute of Environmental Health Sciences of the National Institutes of Health (P30-ES010126).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Emerson, M.A., Golightly, Y.M., Tan, X. et al. Integrating access to care and tumor patterns by race and age in the Carolina Breast Cancer Study, 2008–2013. Cancer Causes Control 31, 221–230 (2020). https://doi.org/10.1007/s10552-019-01265-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-019-01265-0