Abstract
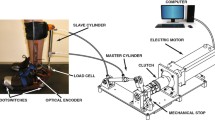
Lower-limb exoskeletons have the potential to improve mobility in individuals with movement disabilities, such as cerebral palsy (CP). The goal of this study was to assess the impact of plantar-flexor assistance from an untethered ankle exoskeleton on dynamic stability during unperturbed and perturbed walking in individuals with CP. Seven participants with CP (Gross Motor Function Classification System levels I-III, ages 6–31 years) completed a treadmill walking protocol under their normal walking condition and while wearing an ankle exoskeleton that provided adaptive plantar-flexor assistance. Pseudo-randomized treadmill perturbations were delivered during stance phase by accelerating one side of a split-belt treadmill. Treadmill perturbations resulted in a significant decrease in anteroposterior minimum margin-of-stability (− 32.1%, p < 0.001), and a significant increase in contralateral limb step length (8.1%, p = 0.005), integrated soleus activity during unassisted walking (23.4%, p = 0.02), and peak biological ankle moment (9.6%, p = 0.03) during stance phase. Plantar-flexor assistance did not significantly alter margin-of-stability, step length, soleus activity, or ankle moments during both unperturbed and perturbed walking. These results indicate that adaptive plantar-flexor assistance from an untethered ankle exoskeleton does not significantly alter dynamic stability maintenance during unperturbed and perturbed walking for individuals with CP, supporting future research in real-world environments.






Similar content being viewed by others
Abbreviations
- CP:
-
Cerebral palsy
- GMFCS:
-
Gross Motor Function Classification System
- EMG:
-
Electromyography
- MoS:
-
Margin-of-stability
- AP:
-
Anteroposterior
- ML:
-
Mediolateral
- CoM:
-
Center of mass
- BoS:
-
Base of support
- g :
-
Gravity
- l :
-
Pendulum length
- iEMG:
-
Integrated EMG
- SL:
-
Step length
- SW:
-
Step width
- ANOVA:
-
Analysis of variance
References
Armand, S., G. Decoulon, and A. Bonnefoy-Mazure. Gait analysis in children with cerebral palsy. EFORT Open Rev. 1:448–460, 2016.
Arnold, A. S., F. C. Anderson, M. G. Pandy, and S. L. Delp. Muscular contributions to hip and knee extension during the single limb stance phase of normal gait: a framework for investigating the causes of crouch gait. J. Biomech. 38:2181–2189, 2005.
Bjornson, K. F., B. Belza, D. Kartin, R. Logsdon, and J. F. McLaughlin. Ambulatory physical activity performance in youth with cerebral palsy and youth who are developing typically. Phys. Ther. 87(3):248–257, 2007.
Boyer, E. R., and A. Patterson. Gait pathology subtypes are not associated with self-reported fall frequency in children with cerebral palsy. Gait Posture 63:189–194, 2018.
Boyle, C. A., S. Boulet, L. A. Schieve, R. A. Cohen, S. J. Blumberg, M. Yeargin-Allsopp, S. Visser, and M. D. Kogan. Trends in the prevalence of developmental disabilities in US children, 1997-2008. Pediatrics 127:1034–1042, 2011.
Bruijn, S. M., O. G. Meijer, P. J. Beek, and J. H. Van Dieen. Assessing the stability of human locomotion: a review of current measures. J. R. Soc. Interface 10(83):20120999, 2013.
Delp, S. L., F. C. Anderson, A. S. Arnold, P. Loan, A. Habib, C. T. John, E. Guendelman, and D. G. Thelen. OpenSim: open-source software to create and analyze dynamic simulations of movement. IEEE Trans. Biomed. Eng. 54:1940–1950, 2007.
Esquenazi, A., M. Talaty, A. Packel, and M. Saulino. The ReWalk powered exoskeleton to restore ambulatory function to individuals with thoracic-level motor-complete spinal cord injury. Am. J. Phys. Med. Rehabil. 91:911–921, 2012.
Gage, J. R., M. H. Schwartz, S. E. Koop, and T. F. Novacheck. The Identification and Treatment of Gait Problems in Cerebral Palsy. London: Mac Keith Press, 2009.
Gasparri, G. M., J. Luque, and Z. F. Lerner. Proportional joint-moment control for instantaneously adaptive ankle exoskeleton assistance. IEEE Trans. Neural Syst. Rehabil. Eng. 27:751–759, 2019.
Griffin, R., T. Cobb, T. Craig, M. Daniel, N. van Dijk, J. Gines, K. Kramer, S. Shah, O. Siebinga, J. Smith, and P. Neuhaus. Stepping forward with exoskeletons: team IHMC?s design and approach in the 2016 cybathlon. IEEE Robot. Autom. Mag. 24:66–74, 2017.
Hof, A. L. Scaling gait data to body size. Gait Posture 4:222–223, 1996.
Hof, A. L., M. G. J. Gazendam, and W. E. Sinke. The condition for dynamic stability. J. Biomech. 2005. https://doi.org/10.1016/j.jbiomech.2004.03.025.
Ilmane, N., S. Croteau, and C. Duclos. Quantifying dynamic and postural balance difficulty during gait perturbations using stabilizing/destabilizing forces. J. Biomech. 48:441–448, 2015.
Johnson, D. L., F. Miller, P. Subramanian, and C. M. Modlesky. Adipose tissue infiltration of skeletal muscle in children with cerebral palsy. J. Pediatr. 154:715–720, 2009.
Kang, J., D. Martelli, V. Vashista, I. Martinez-Hernandez, H. Kim, and S. K. Agrawal. Robot-driven downward pelvic pull to improve crouch gait in children with cerebral palsy. Sci. Robot. 2:eaan2634, 2017.
Kerr, C., J. Parkes, M. Stevenson, A. P. Cosgrove, and B. C. Mcdowell. Energy efficiency in gait, activity, participation, and health status in children with cerebral palsy. Dev. Med. Child Neurol. 50:204–210, 2008.
Kurz, M. J., D. J. Arpin, and B. Corr. Differences in the dynamic gait stability of children with cerebral palsy and typically developing children. Gait Posture 36:600–604, 2012.
Lee, S., J. Kim, L. Baker, A. Long, N. Karavas, N. Menard, I. Galiana, and C. J. Walsh. Autonomous multi-joint soft exosuit with augmentation-power-based control parameter tuning reduces energy cost of loaded walking. J. Neuroeng. Rehabil. 15:66, 2018.
Lerner, Z. F., G. M. Gasparri, M. O. Bair, J. L. Lawson, J. Luque, T. A. Harvey, and A. T. Lerner. An untethered ankle exoskeleton improves walking economy in a pilot study of individuals with cerebral palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 26:1985–1993, 2018.
Lerner, Z. F., T. A. Harvey, and J. L. Lawson. A battery-powered ankle exoskeleton improves gait mechanics in a feasibility study of individuals with cerebral palsy. Ann. Biomed. Eng. 2019. https://doi.org/10.1007/s10439-019-02237-w.
Liao, H.-F., and A.-W. Hwang. Relations of balance function and gross motor ability for children with cerebral palsy. Percept. Mot. Skills 96:1173–1184, 2003.
Martelli, D., J. Kang, and S. K. Agrawal. A perturbation-based gait training with multidirectional waist-pulls generalizes to split-belt treadmill slips. In: IEEE/RAS-EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), 2018.
Martelli, D., L. Luo, J. Kang, U. J. Kang, S. Fahn, and S. K. Agrawal. Adaptation of stability during perturbed walking in Parkinson’s disease. Sci. Rep. 7:1–11, 2017.
McAndrew Young, P. M., J. M. Wilken, and J. B. Dingwell. Dynamic margins of stability during human walking in destabilizing environments. J. Biomech. 45:1053–1059, 2012.
Modlesky, C. M., S. A. Kanoff, D. L. Johnson, P. Subramanian, and F. Miller. Evaluation of the femoral midshaft in children with cerebral palsy using magnetic resonance imaging. Osteoporos. Int. 20:609–615, 2009.
Ohtsu, H., S. Yoshida, T. Minamisawa, T. Takahashi, S. Yomogida, and H. Kanzaki. Investigation of balance strategy over gait cycle based on margin of stability. J. Biomech. 95:2019.
Okubo, Y., M. A. Brodie, D. L. Sturnieks, C. Hicks, H. Carter, B. Toson, and S. R. Lord. Exposure to trips and slips with increasing unpredictability while walking can improve balance recovery responses with minimum predictive gait alterations. PLoS ONE 13:2018.
Orekhov, G., Y. Fang, J. Luque, and Z. F. Lerner. Ankle exoskeleton assistance can improve over-ground walking economy in individuals with cerebral palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 28:461–467, 2020.
Owings, T. M., M. J. Pavol, and M. D. Grabiner. Mechanisms of failed recovery following postural perturbations on a motorized treadmill mimic those associated with an actual forward trip. Clin. Biomech. 16:813–819, 2001.
Rethwilm, R., H. Böhm, M. Haase, D. Perchthaler, C. U. Dussa, and P. Federolf. Dynamic stability in cerebral palsy during walking and running: predictors and regulation strategies. Gait Posture 84:329–334, 2021.
Rose, J., J. G. Gamble, A. Burgos, J. Medeiros, and W. L. Haskell. Energy expenditure index of walking for normal children and for children with cerebral palsy. Dev. Med. Child Neurol. 32:333–340, 1990.
Sawicki, G. S., and D. P. Ferris. Mechanics and energetics of level walking with powered ankle exoskeletons. J. Exp. Biol. 211:1402–1413, 2008.
Sessoms, P. H., M. Wyatt, M. Grabiner, J. D. Collins, T. Kingsbury, N. Thesing, and K. Kaufman. Method for evoking a trip-like response using a treadmill-based perturbation during locomotion. J. Biomech. 47:277–280, 2014.
Stevenson, R. D., M. Conaway, J. W. Barrington, S. L. Cuthill, G. Worley, and R. C. Henderson. Fracture rate in children with cerebral palsy. Pediatr. Rehabil. 9:396–403, 2006.
Süptitz, F., K. Karamanidis, M. M. Catalá, and G. P. Brüggemann. Symmetry and reproducibility of the components of dynamic stability in young adults at different walking velocities on the treadmill. J. Electromyogr. Kinesiol. 22:301–307, 2012.
Tracy, J. B., D. A. Petersen, J. Pigman, B. C. Conner, H. G. Wright, C. M. Modlesky, F. Miller, C. L. Johnson, and J. R. Crenshaw. Dynamic stability during walking in children with and without cerebral palsy. Gait Posture 72:182–187, 2019.
Van Dijsseldonk, R. B., L. A. F. De Jong, B. E. Groen, M. V. Van Der Hulst, A. C. H. Geurts, and N. L. W. Keijsers. Gait stability training in a virtual environment improves gait and dynamic balance capacity in incomplete spinal cord injury patients. Front. Neurol. 9:1–12, 2018.
Vouga, T., R. Baud, J. Fasola, M. Bouri, and H. Bleuler. TWIICE—a lightweight lower-limb exoskeleton for complete paraplegics. In: The IEEE International Conference on Rehabilitation Robotics, vol. 1000, pp. 1639–1645, 2017. https://doi.org/10.1109/icorr.2017.8009483.
Woollacott, M. H., and A. Shumway-Cook. Postural dysfunction during standing and walking in children with cerebral palsy: what are the underlying problems and what new therapies might improve balance? Neural Plasticity 12:211–219, 2005.
Acknowledgments
This research was supported in part by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R15HD099664. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work was also supported in part by the University of Arizona College of Medicine – Phoenix MD/PhD Program. The authors would like to thank James Babers and Leah Liebelt for their assistance with device manufacturing. The authors would also like to thank the participants and their families for their involvement in the study.
Competing interest
ZFL is a named inventor on pending utility patent applications that describe the exoskeleton utilized in the study. ZFL is a co-founder of a company seeking to commercialize the device. The other authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Stefan M Duma oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Video 1 Representative perturbations during unassisted and assisted conditions (MP4 8606 kb)
Rights and permissions
About this article
Cite this article
Harvey, T.A., Conner, B.C. & Lerner, Z.F. Does Ankle Exoskeleton Assistance Impair Stability During Walking in Individuals with Cerebral Palsy?. Ann Biomed Eng 49, 2522–2532 (2021). https://doi.org/10.1007/s10439-021-02822-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-021-02822-y