Abstract
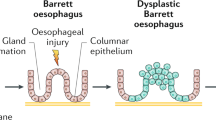
Reflux of bile acid into the esophagus induces esophagitis, inflammation-stimulated hyperplasia, metaplasia such as Barrett’s esophagus (BE), and esophageal adenocarcinoma (EAC). Caudal-type homeobox 2 (Cdx2) via nuclear factor (NF)-κB induced by bile acid is an important factor in the development of BE and EAC. In colorectal cancer, experimental data suggest a chemopreventive effect of ursodeoxycholic acid (UDCA). We hypothesized that UDCA may protect against the esophageal inflammation–metaplasia–carcinoma sequence by decreasing the overall proportion of the toxic bile acids. Wistar male rats that underwent a duodenoesophageal reflux procedure were divided into two groups. One group was given commercial chow (control group), and the other was given experimental chow containing UDCA (UDCA group). The animals were killed at 40 weeks after surgery, and their bile and esophagus were examined. In the UDCA group, the esophagitis was milder and the incidence of BE was significantly lower (p < 0.05) than in the control group, and EAC was not observed (p < 0.05). In analysis of the compartment of bile acid, UDCA was markedly increased in the UDCA group compared with the control group (32.7 ± 11.4 vs. 0.82 ± 0.33 mmol/L, p < 0.05) and cholic acid was decreased (32.7 ± 4.05 vs. 60.9 ± 8.26 mmol/L, p < 0.05). Expression intensity of Cdx2 and NF-κB was greater in the control group than in the UDCA group (p < 0.05). UDCA may be a chemopreventive agent against EAC by varying the bile acid composition.










Similar content being viewed by others
References
Pera M. Epidemiology of esophageal cancer, especially adenocarcinoma of the esophagus and esophagogastric junction. Recent Results Cancer Res. 2000;155:1–14.
Pohl H, Welch HG. The role of overdiagnosis and reclassification in the marked increase of esophageal adenocarcinoma incidence. J Natl Cancer Inst. 2005;97:142–6.
Fujimura T, Oyama K, Sasaki S, Nishijima K, Miyashita T, Ohta T, Miwa K, Hattori T. Inflammation-related carcinogenesis and prevention in esophageal adenocarcinoma using rat duodenoesophageal reflux models. Cancers. 2011;3:3206–24.
Jankowski JA, Harrison RF, Perry I, Balkwill F, Tselepis C. Barrett’s metaplasia. Lancet. 2000;356:2079–85.
Stein HJ, Feussner H, Kauer W, DeMeester TR, Siewert R. Alkaline gastroesophageal reflux: assessment by ambulatory esophageal aspiration and pH monitoring. Am J Surg. 1994;167:163–8.
Gillen P, Keeling P, Byrne PJ, Healy M, O’Moore RR, Hennessy TPJ. Implication of duodenogastric reflux in the pathogenesis of Barrett’s oesophagus. Br J Surg. 1998;75:540–3.
Iftikhar SY, Ledingham S, Steele RJC, Evans DF, Lendrum K, Atkinson M, Hardcastle JD. Bile reflux in columnar-lined Barrett’s oesophagus. Ann R Coll Surg Engl. 1993;75:411–6.
Lagergren J, Bergström R, Lindgren A, Nyrén O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825–31.
Nehra D, Howell P, Williams CP, Pye JK, Beynon J. Toxic bile acids in gastro-oesophageal reflux disease: influence of gastric acidity. Gut. 1999;44:598–602.
Bozikas A, Marsman WA, Rosmolen WD, van Baal JWPM, Kulik W, ten Kate FJW, Krishnadath KK, Bergman JJGHM. The effect of oral administration of ursodeoxycholic acid and high-dose proton pump inhibitors on the histology of Barrett’s esophagus. Dis Esophagus. 2008;21:346–54.
Champion G, Richter JE, Vaezi MF, Singh S, Alexander R. Duodenogastroesophageal reflux: relationship to pH and importance in Barrett’s esophagus. Gastroenterology. 1994;107:747–54.
Kazumori H, Ishihara S, Rumi MAK, Kadowaki Y, Kinoshita Y. Bile acids directly augment caudal related homeobox gene Cdx2 expression in oesophageal keratinocytes in Barrett’s epithelium. Gut. 2006;55:16–25.
Phillips RW, Frierson HF Jr, Moskaluk CA. Cdx2 as a marker of epithelial intestinal differentiation in the esophagus. Am J Surg Pathol. 2003;27:1442–7.
Tamagawa Y, Ishimura N, Uno G, Yuki T, Kazumori H, Ishihara S, Amano Y, Kinoshita Y. Notch signaling pathway and Cdx2 expression in the development of Barrett’s esophagus. Lab Invest. 2012;92:896–909.
Moons LMG, Bax DA, Kuipers EJ, van Dekken H, Haringsma J, van Vliet AHM, Siersema PD, Kusters JG. The homeodomain protein CDX2 is an early marker of Barrett’s oesophagus. J Clin Pathol. 2004;57:1063–8.
Debruyne PR, Witek M, Gong L, Birbe R, Chervoneva I, Jin T, Domon-cell C, Palazzo JP, Freund J, Li P, Pitari GM, Schulz S, Waldman SA. Bile acids induce ectopic expression of intestinal guanylyl cyclase C through nuclear factor-κB and Cdx2 in human esophageal cells. Gastroenterology. 2006;130:1191–206.
Liu T, Zhang X, So C, Wang S, Wang P, Yan L, Myers R, Chen Z, Patterson AP, Yang CS, Chen X. Regulation of Cdx2 expression by promoter methylation, and effects of Cdx2 transfection on morphology and gene expression of human esophageal epithelial cells. Carcinogenesis. 2007;28:488–96.
Paumgartner G, Beuers U. Ursodeoxycholic acid in cholestatic liver disease: mechanisms of action and therapeutic use revisited. Hepatology. 2002;36:525–31.
Goldman A, Condon A, Adler E, Minnella M, Bernstein C, Bernstein H, Dvorak K. Protective effects of glycoursodeoxycholic acid in Barrett’s esophagus cells. Dis Esophagus. 2010;23:83–93.
Thomas C, Pellicciari R, Pruzanski M, Auwerx J, Schoonjans K. Targeting bile-acid signaling for metabolic diseases. Nat Rev Drug Discov. 2008;7:678–93.
Earnest DL, Holubec H, Wali RK, Jolley CS, Bissonette M, Bhattacharyya AK, Roy H, Khare S, Brasitus TA. Chemoprevention of azoxymethane-induced colonic carcinogenesis by supplemental dietary ursodeoxycholic acid. Cancer Res. 1994;54:5071–4.
Loddenkemper C, Keller S, Hanski M, Cao M, Jahreis G, Stein H, Zeitz M, Hanski C. Prevention of colitis-associated carcinogenesis in a mouse model by diet supplementation with ursodeoxycholic acid. Int J Cancer. 2006;118:2750–7.
Alberts DS, Martínez ME, Hess LM, Einspahr JG, Green SB, Bhattacharyya AK, Guillen J, Krutzsch M, Batta AK, Salen G, Fales L, Koonce K, Parish D, Clouser M, Roe D, Lance P. Phase III trial of ursodeoxycholic acid to prevent colorectal adenoma recurrence. J Natl Cancer Inst. 2005;97:846–53.
Miwa K, Sahara H, Segawa M, Kinami S, Sato T, Miyazaki I, Hattori T. Reflux of duodenal or gastro-duodenal contents induces esophageal carcinoma in rats. Int J Cancer. 1996;67:269–74.
Chen K, Mukaisho K, Sugihara H, Araki Y, Yamamoto G, Hattori T. High animal-fat intake changes the bile-acid composition of bile juice and enhances the development of Barrett’s esophagus and esophageal adenocarcinoma in a rat duodenal-contents reflux model. Cancer Sci. 2007;98:1683–8.
Jenkins GJS, Harries K, Doak SH, Wilmes A, Griffiths AP, Baxter JN, Parry JM. The bile acid deoxycholic acid (DCA) at neutral pH, activates NF-κB and induces IL-8 expression in oesophageal cells in vitro. Carcinogenesis. 2004;25:317–23.
Oyama K, Fujimura T, Ninomiya I, Miyashita T, Kinami S, Fushida S, Ohta T, Miwa K. A COX-2 inhibitor prevents the esophageal inflammation–metaplasia–adenocarcinoma sequence in rats. Carcinogenesis. 2005;26:565–70.
Rost D, Rudolph G, Kloeters-Plachky P, Stiehl A. Effect of high-dose ursodeoxycholic acid on its biliary enrichment in primary sclerosing cholangitis. Hepatology. 2004;40:693–8.
Eda A, Osawa H, Satoh K, Yanaka I, Kihira K, Ishino Y, Mutoh H, Sugano K. Aberrant expression of CDX2 in Barrett’s epithelium and inflammatory esophageal mucosa. J Gastroenterol. 2003;38:14–22.
Burnat G, Majka J, Konturek PC. Bile acids are multifunctional modulators of the Barrett’s carcinogenesis. J Physiol Pharmacol. 2010;61:185–92.
Rayet B, Gélinas C. Aberrant rel/nfκb genes and activity in human cancer. Oncogene. 1999;18:6938–47.
O’Riordan JM, Abdel-Latif MM, Ravi N, McNamara D, Byrne PJ, McDonald GS, Keeling PW, Kelleher D, Reynolds JV. Proinflammatory cytokine and nuclear factor kappa-B expression along the inflammation–metaplasia–dysplasia–adenocarcinoma sequence in the esophagus. Am J Gastroenterol. 2005;100:1257–64.
Cronin J, Williams L, McAdam E, Eltahir Z, Griffiths P, Baxter J, Jenkins G. The role of secondary bile acids in neoplastic development in the esophagus. Biochem Soc Trans. 2010;38:337–42.
Miura T, Ouchida R, Yoshikawa N, Okamoto K, Makino Y, Nakamura T, Morimoto C, Makino I, Tanaka H. Functional modulation of the glucocorticoid receptor and suppression of NF-κB-dependent transcription by ursodeoxycholic acid. J Biol Chem. 2001;276:47371–8.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ojima, E., Fujimura, T., Oyama, K. et al. Chemoprevention of esophageal adenocarcinoma in a rat model by ursodeoxycholic acid. Clin Exp Med 15, 343–350 (2015). https://doi.org/10.1007/s10238-014-0301-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-014-0301-x