Abstract
Background
Research on short-term outcomes and long-term oncological results of laparoscopic pelvic exenteration (LPE) for locally advanced rectal cancer (LARC) is still limited. The purpose of this study was to compare the outcomes of LPE and open pelvic exenteration (OPE).
Methods
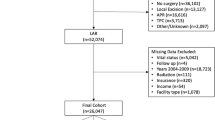
Between January 2010 and December 2019, consecutive LARC patients who underwent radical pelvic exenteration at Peking University First Hospital were enrolled. Groups were matched at a 1:1 ratio using propensity score matching. The primary endpoints were 3 year overall survival (OS) and disease-free survival (DFS). The secondary endpoints were postoperative short-term outcomes.
Results
There were 144 patients (68 males and 76 females, median age 58.5 [range 27.0–86.0] years). After matching, patients were stratified into LPE (n = 48) and OPE (n = 48) groups (LPE: 24 males and 24 females, median age 57.0 [range 27.0-81.0] years; OPE: 26 males and 22 females, median age 58.0[range 36.0-80.0] years). There were no significant differences on baseline data between the two groups. Compared with the OPE group, the LPE group had a significantly lower estimated blood loss (200 vs 500 ml, p = 0.003), less overall postoperative complications (12/48 vs 25/48, p = 0.006), less surgical site infection (8/48 vs 20/48, p = 0.007), shorter length of stay (12 vs. 15 days, p = 0.005), but similar operative time (344 vs. 360 min, p = 0.493). The pathological R0 resection rate (98.0% vs. 93.7%, p = 0.610), 3 year local recurrence (18.4% vs. 23.5, p = 0.140), 3 year OS (74.6% vs. 65.5%, p = 0.290) and 3-year DFS (60.0% vs. 50.3%, p = 0.208) were similar between the two groups. Shorter distance from anal verge (HR = 0.92, p = 0.042), (y) pT4b (HR = 2.45, p = 0.023), (y)pN1-2 (HR = 2.42, p = 0.004) and positive CRM (HR = 6.23, p = 0.004) were independent prognostic risks for 3 year DFS.
Conclusions
LPE can be performed safely and has certain short-term advantages over OPE, most notably less blood loss and surgical site infection. However, LPE does not improve long-term oncological outcomes.



Similar content being viewed by others
References
Yang TX, Morris DL, Chua TC (2013) Pelvic exenteration for rectal cancer: a systematic review. Dis Colon Rectum 56:519–531
Kusters M, Austin KK, Solomon MJ et al (2015) Survival after pelvic exenteration for T4 rectal cancer. Br J Surg 102:125–131
Platt E, Dovell G, Smolarek S (2018) Systematic review of outcomes following pelvic exenteration for the treatment of primary and recurrent locally advanced rectal cancer. Tech Coloproctol 22:835–845
Bonjer HJ, Deijen CL, Abis GA et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Stevenson ARL, Solomon MJ, Brown CSB et al (2019) Disease-free survival and local recurrence after laparoscopic-assisted resection or open resection for rectal cancer: the Australasian Laparoscopic Cancer of the Rectum Randomized Clinical Trial. Ann Surg 269:596–602
Akiyoshi T (2016) Technical feasibility of laparoscopic extended surgery beyond total mesorectal excision for primary or recurrent rectal cancer. World J Gastroenterol 22:718–726
Uehara K, Nakamura H, Yoshino Y et al (2016) Initial experience of laparoscopic pelvic exenteration and comparison with conventional open surgery. Surg Endosc 30:132–138
Kimura K, Ikeda M, Kataoka K et al (2020) Sacrectomy for recurrent rectal cancer using the transanal total mesorectum excision technique. Dis Colon Rectum 63:e566–e573
Kumar NA, Sasi SP, Shinde RS et al (2020) Minimally invasive surgery for pelvic exenteration in primary colorectal cancer. JSLS. https://doi.org/10.4293/JSLS.2020.00026
Shin US, Nancy YY, Nguyen AT et al (2016) Oncologic outcomes of extended robotic resection for rectal cancer. Ann Surg Oncol 23:2249–2257
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Yang K, Cai L, Yao L et al (2015) Laparoscopic total pelvic exenteration for pelvic malignancies: the technique and short-time outcome of 11 cases. World J Surg Oncol 13:301
Zuo S, Chen HK, Zheng LJ et al (2020) Effect of laparoscopic posterior pelvic exenteration for locally advanced rectal cancer. J Colorectal Anal Surg 26:148–153
Collaborative P (2018) Minimally invasive surgery techniques in pelvic exenteration: a systematic and meta-analysis review. Surg Endosc 32:4707–4715
Radwan RW, Jones HG, Rawat N et al (2015) Determinants of survival following pelvic exenteration for primary rectal cancer. Br J Surg 102:1278–1284
Waters PS, Peacock O, Warrier SK et al (2019) Evolution of pelvic exenteration surgery resectional trends and survival outcomes over three decades. Eur J Surg Oncol 45:2325–2333
Collaborative P (2019) Surgical and survival outcomes following pelvic exenteration for locally advanced primary rectal cancer: results from an international collaboration. Ann Surg 269:315–321
Perez RO, Sao JG, P., Vailati B. B. et al (2018) Lateral Node dissection in rectal cancer in the era of minimally invasive surgery: a step-by-step description for the surgeon unacquainted with this complex procedure with the use of the laparoscopic approach. Dis Colon Rectum 61:1237–1240
Beppu N, Ikeda M, Kimura K et al (2020) Extended total mesorectal excision based on the avascular planes of the retroperitoneum for locally advanced rectal cancer with lateral pelvic sidewall invasion. Dis Colon Rectum 63:1475–1481
Puntambekar S, Sharma V, Jamkar AV et al (2016) Our experience of laparoscopic anterior exenteration in locally advanced cervical carcinoma. J Minim Invasive Gynecol 23:396–403
Juo YY, Hyder O, Haider AH et al (2014) Is minimally invasive colon resection better than traditional approaches?: First comprehensive national examination with propensity score matching. JAMA Surg 149:177–184
Klaver CEL, Kappen TM, Borstlap WAA et al (2017) Laparoscopic surgery for T4 colon cancer: a systematic review and meta-analysis. Surg Endosc 31:4902–4912
Moutardier V, Houvenaeghel G, Lelong B et al (2003) Colorectal function preservation in posterior and total supralevator exenteration for gynecologic malignancies: an 89-patient series. Gynecol Oncol 89:155–159
Liu J, Zheng L, Ren S et al (2021) Nomogram for predicting the probability of permanent stoma after laparoscopic intersphincteric resection. J Gastrointest Surg 25:3218–3229
Roodbeen SX, De Lacy FB, Van Dieren S et al (2019) Predictive factors and risk model for positive circumferential resection margin rate after transanal total mesorectal excision in 2653 patients with rectal cancer. Ann Surg 270:884–891
Leijssen LGJ, Dinaux AM, Amri R et al (2019) The impact of a multivisceral resection and adjuvant therapy in locally advanced colon cancer. J Gastrointest Surg 23:357–366
Dinaux AM, Leijssen LGJ, Bordeianou LG et al (2018) Effects of local multivisceral resection for clinically locally advanced rectal cancer on long-term outcomes. J Surg Oncol 117:1323–1329
Hishida T, Masai K, Kaseda K et al (2021) Debulking surgery for malignant tumors: the current status, evidence and future perspectives. Jpn J Clin Oncol 51:1349–1362
Gunderson LL, Jessup JM, Sargent DJ et al (2010) Revised tumor and node categorization for rectal cancer based on surveillance, epidemiology, and end results and rectal pooled analysis outcomes. J Clin Oncol 28:256–263
Rottoli M, Vallicelli C, Boschi L et al (2017) Outcomes of pelvic exenteration for recurrent and primary locally advanced rectal cancer. Int J Surg 48:69–73
Keller DS, Khorgami Z, Swendseid B et al (2014) Laparoscopic and converted approaches to rectal cancer resection have superior long-term outcomes: a comparative study by operative approach. Surg Endosc 28:1940–1948
Funding
This study was supported by grants from the National Natural Science Foundation of China (No. 81272710) and Wu Jieping’s Foundation Special for Clinical Research (No. 320.6750.2021–04-02).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Dr Jianqiang Tang, Junguang Liu, Binbin Du, Junling Zhang, Lijun Zheng, Xin Wang, and Yuanlian Wan have no conflict of interest or financial ties to disclose.
Ethical approval
All work was carried out in compliance with the Ethical Principles for Medical Research Involving Human Subjects outlined in the Helsinki Declaration in 1975 (revised in 2000).
Informed consent
All patients enrolled provided written informed consent, and this study was approved by Peking University First Hospital ethics committee of biomedical research (2021–351).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tang, J., Liu, J., Du, B. et al. Short- and long-term outcomes of laparoscopic versus open pelvic exenteration for locally advanced rectal cancer: a single-center propensity score matching analysis. Tech Coloproctol 27, 43–52 (2023). https://doi.org/10.1007/s10151-022-02691-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-022-02691-0