Abstract
Introduction
The purpose of this study was to evaluate the acute fixation strength of fibrin sealant as an alternative fixation method for laparoscopic ventral hernia repair (LVHR) when utilized with absorbable and nonabsorbable barrier meshes.
Methods
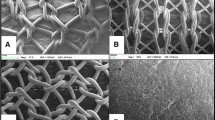
Representative mesh types for LVHR included one nonabsorbable barrier mesh (Bard®Composix™) and three absorbable barrier meshes (Sepramesh™, Proceed™, and Parietex™ Composite Mesh). Macroporous polypropylene mesh (Prolite Ultra™) served as a control. An associated pilot study demonstrated that acute fixation was not achieved with C-Qur™ or Dualmesh®, thus these meshes were not subjected to further analysis. Two fibrin sealants varying in thrombin concentration (TISSEEL™ 500 IU/ml or ARTISS™ 4 IU/ml) were each utilized to secure a 3 × 4 cm piece of mesh to the peritoneal surface of harvested abdominal wall from New Zealand white rabbits. Ten samples were prepared for each mesh and fibrin sealant combination. The resulting mesh-tissue interface (3 × 3 cm) underwent lap shear testing at a rate of 0.42 mm/s using a tensiometer (Instron 5542, Norwood, MA). The maximum load sustained by the construct was recorded as the acute fixation strength in units of Newtons (N). Data are given as means ± SEM. Statistical significance (P < 0.05) was determined using a two-way ANOVA and Bonferroni post-test.
Results
There was no significant difference (P > 0.05) in the acute fixation strength achieved by ARTISS™ versus TISSEEL™ with Composix™, Sepramesh™, Proceed™, and Parietex™ Composite Mesh. However, Prolite Ultra™ fixed with ARTISS™ (7.099 ± 1.01 N) had a significantly higher tensile strength (P < 0.001) than Prolite Ultra™ fixed with TISSEEL™ (3.405 ± 0.72 N). Among meshes fixed with TISSEEL™, Parietex™ Composite (3.936 ± 0.73 N) was significantly stronger than Sepramesh™ (1.760 ± 0.33 N) (P < 0.05).
Conclusions
Acute fixation strength is equivalent for TISSEEL™ and ARTISS™ fibrin sealants for selected nonabsorbable (Composix™) and absorbable barrier-coated (Sepramesh™, Proceed™, and Parietex™ Composite Mesh) meshes. Previous evaluations in this model indicated fibrin sealant alone did not appear to be a suitable method of fixation with C-Qur™ or DualMesh® against the peritoneum. Long-term evaluation is needed to evaluate the efficacy of this method of fixation using absorbable and nonabsorbable barrier-coated meshes in a model of LVHR.



Similar content being viewed by others
References
Pierce RA, Spitler JA, Frisella MM, Matthews BD, Brunt LM (2007) Pooled data analysis of laparoscopic vs open ventral hernia repair: 14 years of patient data accrual. Surg Endosc 21(3):378–386
Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, Stassen LPS, Vente JP, Weidema WF, Schrijvers AJP, van Vroonhoven TJMV (1997) Comparison of conventional anterior surgery and laparoscopic surgery for inguinal hernia repair. N Engl J Med 336(22):1541–1547
Crawford DL, Phillips EH (1998) Laparoscopic repair and groin hernia surgery. Surg Clin North Am 78(6):1047–1062
Knook MT, Weidema WF, Stassen LP, van Steensel CJ (1999) Laparoscopic repair of recurrent inguinal hernias after endoscopic herniorrhaphy. Surg Endosc 13(11):1145–1147
Carbonell AM, Harold KL, Mahmutovic AJ, Hassan R, Matthews BD, Kercher KW, Sing RF, Heniford BT (2003) Local injection for the treatment of suture site pain after laparoscopic ventral hernia repair. Am Surg 69(8):688–691
Heniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Ann Surg 238(3):391–399
Karakousis CP, Volpe C, Tanski J, Colby ED, Winston J, Driscoll DL (1995) Use of a mesh for musculoaponeurotic defects of the abdominal wall in cancer surgery and the risk of bowel fistulas. J Am Coll Surg 181(1):11–16
Katkhouda N, Mavor E, Friedlander MH, Mason RJ, Kiyabu M, Grant SW, Achanta K, Kirkman EL, Narayanan K, Essani R (2001) Use of fibrin sealant for prosthetic mesh fixation in laparoscopic extraperitoneal inguinal hernia repair. Ann Surg 233(1):18–25
Joels CS, Matthews BD, Kercher KW, Austin C, Norton HJ, Williams TC, Heniford BT (2005) Evaluation of adhesion formation, mesh fixation strength, and hydroxyproline content after intraabdominal placement of polytetrafluoroethylene mesh secured using titanium spiral tacks, nitinol anchors, and polypropylene suture or polyglactin 910 suture. Surg Endosc 19(6):780–785
Jourdan IC, Bailey ME (1998) Initial experience with the use of n-butyl 2-cyanoacrylate glue for the fixation of polypropylene mesh in laparoscopic hernia repair. Surg Laparosc Endosc 8(4):291–293
Leggat PA, Kedjarune U, Smith DR (2004) Toxicity of cyanoacrylate adhesives and their occupational impacts for dental staff. Ind Health 42:207–211
Samson D, Marshall D (1986) Carcinogenic potential of isobutyl-2-cyanoacrylate. J Neurosurg 65(4):571–572
Fortelny RH, Petter-Puchner AH, Walder N, Mittermayr R, Ohlinger W, Heinze A, Redl H (2007) Cyanoacrylate tissue sealant impairs tissue integration of macroporous mesh in experimental hernia repair. Surg Endosc 21(10):1781–1785
Chevrel JP, Rath AM (1997) The use of fibrin glues in the surgical treatment of incisional hernias. Hernia 1(1):9–14
Lau H (2005) Fibrin sealant versus mechanical stapling for mesh fixation during endoscopic extraperitoneal inguinal hernioplasty: a randomized prospective trial. Ann Surg 242(5):670–675
Topart P, Vandenbroucke F, Lozac’h P (2005) Tisseel versus tack staples as mesh fixation in totally extraperitoneal laparoscopic repair of groin hernias: a retrospective analysis. Surg Endosc 19(5):724–727
Olmi S, Erba L, Bertolini A, Scaini A, Croce E (2006) Fibrin glue for mesh fixation in laparoscopic transabdominal preperitoneal (TAPP) hernia repair: indications, technique, and outcomes. Surg Endosc 20(12):1846–1850
Schwab R, Willms A, Kröger A, Becker HP (2006) Less chronic pain following mesh fixation using a fibrin sealant in TEP inguinal hernia repair. Hernia 10(3):272–277
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, Faillace G, Longoni M (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg 245(2):222–231
Ceccarelli G, Casciola L, Pisanelli MC, Bartoli A, Di Zitti L, Spaziani A, Biancafarina A, Stefanoni M, Patriti A (2008) Comparing fibrin sealant with staples for mesh fixation in laparoscopic transabdominal hernia repair: a case control-study. Surg Endosc 22(3):668–673
Goldenberg MM (2008) Pharmaceutical approval update. PT 33(5):299–302
Acknowledgments
We would like to acknowledge the efforts of Michael Brodt M.S., Department of Orthopedic Surgery, Washington University School of Medicine, St. Louis, Missouri, for mechanical testing of all samples.
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jenkins, E.D., Melman, L., Frisella, M.M. et al. Evaluation of acute fixation strength of absorbable and nonabsorbable barrier coated mesh secured with fibrin sealant. Hernia 14, 505–509 (2010). https://doi.org/10.1007/s10029-010-0670-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-010-0670-3