Abstract
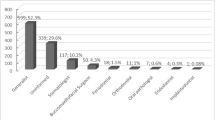
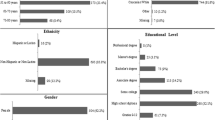
The present study analyzed history of smoking and willingness to quit smoking in patients referred for diagnosis and treatment of different oral mucosal lesions. Prior to the initial clinical examination, patients filled in a standardized questionnaire regarding their current and former smoking habits and willingness to quit. Definitive diagnoses were classified into three groups (benign/reactive lesions, premalignant lesions and conditions, and malignant diseases) and correlated with the self-reported data in the questionnaires. Of the 980 patients included, 514 (52%) described themselves as never smokers, 202 (21%) as former smokers, and 264 (27%) as current smokers. In the group of current smokers, 23% thought their premalignant lesions/conditions were related to their smoking habit, but only 15% of the patients with malignant mucosal diseases saw that correlation. Only 14% of the smokers wanted to commence smoking cessation within the next 30 days. Patients with malignant diseases (31%) showed greater willingness to quit than patients diagnosed with benign/reactive lesions (11%). Future clinical studies should attempt (1) to enhance patients’ awareness of the negative impact of smoking on the oral mucosa and (2) to increase willingness to quit in smokers referred to a dental/oral medicine setting.
Similar content being viewed by others
References
Patel RR, Ryu JH, Vassallo R (2008) Cigarette smoking and diffuse lung disease. Drugs 68:1511–1527
Gupta PC, Murti PR, Bhonsle RB (1996) Epidemiology of cancer by tobacco products and the significance of TSNA. Crit Rev Toxicol 26:183–198
Gandini S, Botteri E, Iodice S, Boniol M, Lowenfels AB, Maisonneuve P, Boyle P (2008) Tobacco smoking and cancer: a meta-analysis. Int J Cancer 122:155–164
Johnson NW, Bain CA (2000) Tobacco and oral disease. EU-Working Group on Tobacco and Oral Health. Br Dent J 189:200–206
Warnakulasuriya S, Dietrich T, Bornstein MM, Peidró EC, Preshaw PM, Walter C, Wennström JL, Bergström J (2010) Oral health risks of tobacco use and effects of cessation. Int Dent J 60:7–30
Reichart PA (2001) Identification of risk groups for oral precancer and cancer and preventive measures. Clin Oral Invest 5:307–213
Needleman I, Warnakulasuriya S, Sutherland G, Bornstein MM, Casals E, Dietrich T, Suvan J (2006) Evaluation of tobacco use cessation (TUC) counselling in the dental office. Oral Health Prev Dent 4:27–47
Johnson NW (2004) The role of the dental team in tobacco cessation. Eur J Dent Educ 8(suppl 4):18–24
Ramseier CA, Mattheos N, Needleman I, Watt R, Wickholm S (2006) Consensus report: first European workshop on tobacco use prevention and cessation for oral health professionals. Oral Health Prev Dent 4:7–18
Ramseier CA, Bornstein MM, Saxer UP, Klingler K, Walter C (2007) Tobacco use prevention and cessation in the dental practice. Schweiz Monatsschr Zahnmed 117:253–278 (in German)
Watt RG, Benzian H, Binnie V, Gafner C, Hovius M, Newton TJ, Mecklenburg RE (2006) Public health aspects of tobacco control: setting the agenda for action by oral health profession across Europe. Oral Health Prev Dent 4:19–26
Gallagher JE, Alajbeg I, Büchler S, Carrassi A, Hovius M, Jacobs A, Jenner M, Kinnunen T, Ulbricht S, Zoitopoulos L (2010) Public health aspects of Tobacco control revisited. Int Dent J 60:31–49
La Vecchia C, Tavani A, Franceschi S, Levi F, Corrao G, Negri E (1997) Epidemiology and prevention of oral cancer. Oral Oncol 33:302–312
Reichart PA, Way TH (2006) Oral cancer and pre-cancer in Myanmar: a short review. J Oral Pathol Med 35:193–196
Zhang X, Reichart PA (2007) A review of betel quid chewing, oral cancer and precancer in mainland China. Oral Oncol 43:424–430
Blot WJ, McLaughlin JK, Winn DM, Austin DF, Greenberg RS, Preston-Martin S, Bernstein L, Schoenberg JB, Stemhagen A, Fraumeni JF Jr (1988) Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res 48:3282–3287
Negri E, La Vecchia C, Franceschi S, Tavani A (1993) Attributable risk for oral cancer in northern Italy. Cancer Epidemiol Biomarkers Prev 2:189–193
Gillison ML (2007) Current topics in the epidemiology of oral cavity and oropharyngeal cancers. Head Neck 29:779–792
Klesges RC, Somes G, Pascale RW, Klesges LM, Murphy M, Brown K, Williams E (1988) Knowledge and beliefs regarding the consequences of cigarette smoking and their relationships to smoking status in a biracial sample. Health Psychol 7:387–401
Strecher VJ, Kreuter MW, Kobrin SC (1995) Do cigarette smokers have unrealistic perceptions of their heart attack, cancer, and stroke risks? J Behav Med 18:45–54
Brownson RC, Jackson-Thompson J, Wilkerson JC, Davis JR, Owens NW, Fisher EB Jr (1992) Demographic and socioeconomic differences in beliefs about the health effects of smoking. Am J Public Health 82:99–103
Demierre MF, Brooks D, Koh HK, Geller AC (1999) Public knowledge, awareness, and perceptions of the association between skin aging and smoking. J Am Acad Dermatol 41:27–30
Oncken C, McKee S, Krishnan-Sarin S, O’Malley S, Mazure CM (2005) Knowledge and perceived risk of smoking-related conditions: a survey of cigarette smokers. Prev Med 40:779–784
Al-Shammari KF, Moussa MA, Al-Ansari JM, Al-Duwairy YS, Honkala EJ (2006) Dental patient awareness of smoking effects on oral health: comparison of smokers and non-smokers. J Dent 34:173–178
Lung ZH, Kelleher MG, Porter RW, Gonzalez J, Lung RF (2005) Poor patient awareness of the relationship between smoking and periodontal diseases. Br Dent J 199:731–737
Kerawala CJ (1999) Oral cancer, smoking and alcohol: the patients’ perspective. Br J Oral Maxillofac Surg 37:374–376
Christen AG (1970) The dentist’s role in helping patients to stop smoking. J Am Dent Assoc 81:1146–1152
Nohlert E, Tegelberg A, Tillgren P, Johansson P, Rosenblad A, Helgason AR (2009) Comparison of a high and a low intensity smoking cessation intervention in a dentistry setting in Sweden: a randomized trial. BMC Public Health 9:121
Needleman I, Binnie VI, Ainamo A, Carr AB, Fundak A, Koeber A, Öhrn K, Rosseel J (2010) Improving the effectiveness of tobacco use cessation (TUC). Int Dent J 60:50–59
Campbell HS, Sletten M, Petty T (1999) Patient perceptions of tobacco cessation services in dental offices. J Am Dent Assoc 130:219–226
Victoroff KZ, Lewis R, Ellis E, Ntragatakis M (2006) Patient receptivity to tobacco cessation counseling in an academic dental clinic: a patient survey. J Public Health Dent 66:209–211
Martinelli E, Palmer RM, Wilson RF, Newton JT (2008) Smoking behaviour and attitudes to periodontal health and quit smoking in patients with periodontal disease. J Clin Periodontol 35:944–954
Ramseier CA, Warnakulasuriya S, Needleman IG, Gallagher JE, Lahtinen A, Ainamo A, Alajbeg I, Albert D, Al-Hazmi N, Antohe E, Beck-Mannagetta J, Benzian H, Bergstrom J, Binnie V, Bornstein MM, Buchler S, Carr A, Carrassi A, Peidro EC, Compton S, Crail J, Crews K, Davis JM, Dietrich T, Enmark B, Fine J, Gallagher J, Jenner T, Forna D, Fundak A, Gyenes M, Hovius M, Jacobs A, Kinnunen T, Knevel R, Koerer A, Labella R, Lulic M, Mattheor N, McEwen A, Ohrn K, Polychronopoulou A, Preshaw P, Radley N, Rosseel J, Schoonheim-Klein M, Suvan J, Ulbricht S, Verstappen P, Walter C, Wennstrom J, Wickholm S, Zoitopoulos L (2010) Consensus report: 2nd European workshop on tobacco use prevention and cessation for oral health professionals. Int Dent J 60:3–6
Davies JM, Ramseier CA, Mattheos N, Schoonheim-Klein M, Compton S, Al-Hazmi N, Polychronopoulou A, Suvan J, Antohé ME, Forna D, Radley N (2010) Education of tobacco use prévention and cessation for dental professionals—a paradigm shift. Int Dent J 60:50–59
Severson HH, Andrews JA, Lichtenstein E, Gordon JS, Barckley MF (1998) Using the hygiene visit to deliver a tobacco cessation program: results of a randomized clinical trial. J Am Dent Assoc 129:993–999
Ebbert JO, Carr AB, Patten CA, Morris RA, Schroeder DR (2007) Tobacco use quitline enrollment through dental practices: a pilot study. J Am Dent Assoc 138:595–601
Binnie VI, McHugh S, Jenkins W, Borland W, Macpherson LM (2007) A randomised controlled trial of a smoking cessation intervention delivered by dental hygienists: a feasibility study. BMC Oral Health 7:5
Acknowledgments
The study was supported by University of Bern departmental funds.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bornstein, M.M., Frei, M., Sendi, P. et al. Patients’ awareness of the potential benefit of smoking cessation. A study evaluating self-reported and clinical data from patients referred to an oral medicine unit. Clin Oral Invest 16, 55–62 (2012). https://doi.org/10.1007/s00784-010-0488-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-010-0488-5