Abstract
Purpose
To use imaging, histology and electrophysiological assessment to compare the Wiltse approach to pedicle fixation with the conventional posterior open approach for thoracolumbar fractures.
Methods
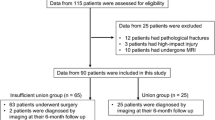
We analyzed clinical and histopathological information of consecutive patients with thoracolumbar fractures who underwent short-segment pedicle fixation using either the Wiltse approach or the posterior open approach. Seventy-five patients were enrolled between June 2010 and August 2014 (Wiltse group 35 cases; posterior open group 40 cases). The two groups were compared for MRI appearance, histological and electrophysiological changes in multifidus muscle.
Results
On MRI, multifidus cross-sectional area (CSA) in the Wiltse group decreased by only 7.6% between pre-op and the last follow-up, compared to 35.4% in the posterior open group, and less fatty infiltration was found in the Wiltse group. Histologically, post-op (removal of internal fixation) tissue from the posterior open group showed disordered myofibrils, with diameter and CSA decreased by 11.6 and 24.3%, respectively; also, the myofibril gap became larger with fat deposition and scar formation. The Wiltse group had no such significant changes. Electrophysiologically, in the posterior open group, median frequency slope (MFs) significantly increased by 67.6% with average amplitude (AA) significantly decreased by 17.5% between pre-op and 12 months post-op. No significant changes were found in the Wiltse group. At 12 months post-op, AA was significantly lower and MFs was higher in the posterior open group than the Wiltse group.
Conclusion
The Wiltse approach showed a lower incidence of multifidus atrophy and denervation, and less fatty infiltration. It is an effective and minimally invasive approach for thoracolumbar fractures.




Similar content being viewed by others
References
Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A (1993) Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine 18:575–581
Taylor H, McGregor AH, Medhi-Zadeh S, Richards S, Kahn N, Zadeh JA et al (2002) The impact of self-retaining retractors on the paraspinal muscles during posterior spinal surgery. Spine 27:2758–2762
Hu ZJ, Fang XQ, Zhou ZJ, Wang JY, Zhao FD, Fan SW (2013) Effect and possible mechanism of muscle-splitting approach on multifidus muscle injury and atrophy after posterior lumbar spine surgery. J Bone Jt Surg Am 95(24):e192 (1–9)
Kim DY, Lee SH, Chung SK, Lee HY (2005) Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine 30:123–129
Mayer TG, Vanharanta H, Gatchel RJ, Mooney V, Barnes D, Judge L (1989) Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine 14(1):33–36
Quint U, Wilke HJ, Shirazi-Adl A, Parnianpour M, Loer F, Claes LE (1998) Importance of the intersegmental trunk muscles for the stability of the lumbar spine: a biomechanical study in vitro. Spine 23(18):1937–1945
Onesti ST (2004) Failed back syndrome. Neurologist 10(5):259–264
Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE (1968) The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Jt Surg Am 50(5):919–926
Ota M, Neo M, Fujibayashi S, Takemoto M, Nakamura T (2010) Advantages of the paraspinal muscle splitting approach in comparison with conventional midline approach for s1 pedicle screw placement. Spine (Phila Pa 1976) 35(11): E452–E457
Mehren C, Siepe CJ (2016) Neuroforaminal decompression and intra-/extraforaminal discectomy via a paraspinal muscle-splitting approach. Eur Spine J 25(Suppl 2):276–277
Choi KC, Kim JS, Lee DC, Park CK (2016) Outcome of decompression alone for foraminal/extraforaminal entrapment of L5 nerve root through Wiltse paraspinal approach. Clin Spine Surg [Epub ahead of print]
Stevens KJ, Spenciner DB, Griffiths KL, Kim KD, ZwienenbergLee M, Alamin T et al (2006) Comparison of minimally invasive and conventional open posterolateral lumbar fusion using magnetic resonance imaging and retraction pressure studies. J Spinal Disord Tech 19:77–86
Isaacs RE, Podichetty VK, Santiago P, Sandhu FA, Spears J, Kelly K et al (2005) Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine 3:98–105
Khoo LT, Palmer S, Laich DT, Fessler RG (2002) Minimally invasive percutaneous posterior lumbar interbody fusion. Neurosurgery 51:S166–S171
Park Y, Ha JW (2007) Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine 32(5):537–543
Schwender JD, Holly LT, Rouben DP, Foley KT (2005) Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech 18(Suppl):S1–S6
Kim KT, Lee SH, Suk KS, Bae SC (2006) The quantitative analysis of tissue injury markers after mini-open lumbar fusion. Spine 31:712–716
Reinhold M, Audigé L, Schnake KJ et al (2013) AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. Eur Spine J 22(10):2184–2201
Battaglia PJ, Maeda Y, Welk A, Hough B, Kettner N (2014) Reliability of the Goutallier classification in quantifying muscle fatty degeneration in the lumbar multifidus using magnetic resonance imaging. J Manip Physiol Ther 37(3):190–197
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC (1994) Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res (304):78–83
Biering-Sorensen F (1984) Physical measurements as risk indicators for low-back trouble over a one-year period. Spine 9:106–119
Sihvonen T, Herno A, Paljarvi L et al (1993) Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine 18:575–581
Kawaguchi Y, Matsui H, Tsuji H (1994) Back muscle injury after posterior lumbar spine surgery. Part 2: Histologic and histochemical analyses in humans. Spine 19:2598–2602
Lu WW, Hu Y, Luk KD et al (2002) Paraspinal muscle activities of patients with scoliosis after spine fusion: an electromyographic study. Spine 27:1180–1185
Macdonald DA, Moseley GL, Hodges PW (2009) Why do some patients keep hurting their back? Evidence of ongoing back muscle dysfunction during remission from recurrent back pain. Pain 142(3):183–188
Macdonald DA, Moseley GL, Hodges PW (2010) People with recurrent low back pain respond differently to trunk loading despite remission from symptoms. Spine (Phila Pa 1976) 35:818–824
Macdonald DA, Dawson AP, Hodges PW (2011) Behavior of the lumbar multifidus during lower extremity movements in people with recurrent low back pain during symptom remission. J Orthop Sports Phys Ther 41(3):155–164
Kawaguchi Y, Matsui H, Tsuji H (1997) Changes in serum creatine phosphokinase MM isoenzyme after lumbar spine surgery. Spine 22(9):1018–1023
Nanji AA (1983) Serum creatine kinase isoenzymes: a review. Muscle Nerve 6:83–90
Kim K, Isu T, Sugawara A, Matsumoto R, Isobe M (2008) Comparison of the effect of 3 different approaches to the lumbar spinal canal on postoperative paraspinal muscle damage. Surg Neurol 69(2):109–113
Suwa H, Hanakita J, Ohshita N, Gotoh K, Matsuoka N, Morizane A (2000) Postoperative changes in paraspinal muscle thickness after various lumbar back surgery procedures. Neurol Med Chir (Tokyo) 40(3):151–154 (discussion 154–155)
Cawley DT, Alexander M, Morris S (2014) Multifidus innervation and muscle assessment post-spinal surgery. Eur Spine J 23(2):320–327
Roy SH, Oddsson LI (1998) Classification of paraspinal muscle impairments by surface electromyography. Phys Ther 78:838–851
Kupa EJ, Roy SH, Kandarian SC et al (1995) Effects of muscle fiber type and size on EMG median frequency and conduction velocity. J Appl Physiol 79:23–32
Gamet D, Duchene J, Garapon-Bar C et al (1993) Surface electromyogram power spectrum in human quadriceps muscle during incremental exercise. J Appl Physiol 74:2704–2710
Fan Shunwu, Zhijun Hu, Fang Xiangqian, Zhao Fengdong, Huang Yue, He-jun Yu (2010) Comparison of paraspinal muscle injury in one-level lumbar posterior inter-body fusion: modified minimally invasive and traditional open approaches. Orthop Surg 2:194–200
Acknowledgements
The authors wish to express their gratitude to Prof. Michael Adams and Dr. Patricia Dolan for help with the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
National Natural Science Foundation of China (project number: 31270997); Zhejiang Medical and Health Science and Technology project: (project number: 2016136915, 2013KYA2334).
Additional information
L. Junhui, P. Zhengbao and X. Wenbin contributed equally to this paper and should be considered co-first authors.
Rights and permissions
About this article
Cite this article
Junhui, L., Zhengbao, P., Wenbin, X. et al. Comparison of pedicle fixation by the Wiltse approach and the conventional posterior open approach for thoracolumbar fractures, using MRI, histological and electrophysiological analyses of the multifidus muscle. Eur Spine J 26, 1506–1514 (2017). https://doi.org/10.1007/s00586-017-5010-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5010-1