Abstract
Background
The professional impact of upper limb lymphedema, which affects 15–20% of women after breast cancer treatment, has been poorly evaluated.
Objective
To analyze lymphedema characteristics and global lymphedema- and/or sleeve-attributed impact (mildly inconvenient to severely debilitating) on professional activities, workplace relationships, and workstation ergonomics.
Methods
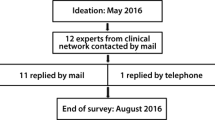
Patients received a standardized, anonymous, self-administered questionnaire at consultation/hospitalization for treatment in a specialized lymphedema management center.
Results
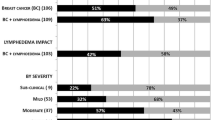
All 134 consecutive women (March/2015–March/2017; median age 54), with 53-month median lymphedema duration and 34% median excess volume, were included; 35% considered global impact (arm-use impairment) high. For high vs. low global impact during occupational activities, univariate analyses identified global impairment as being associated with the low (23.8%), intermediate (60%), or high (63.2%) (p < 0.01) arm-use level, while multivariate analyses retained intermediate (OR 6.9 [95% CI 1.1–118.1], p < 0.01) and high (OR 4.5 [95% CI 1.5–37.3], p < 0.05) vs. low arm-use level. Lymphedema affected the careers of 70 (52.2%) patients, mostly those with severely impaired arm movement (53.8% vs. 10.2, p < 0.001), without modifying their relationships with colleagues and superiors for 84 (62.7%). Highly impaired women reported changed relationships with colleagues (45% vs. 20%, p < 0.01) and superiors (43.6% vs. 16.9%, p < 0.01). Only 10 women’s (7.5%) job changes reflected lymphedema or its treatment. Workplace adaptations (53% ergonomic) were made for 36 (26.9%) patients, mostly those with greater arm-movement impairment (43.6% vs. 25.3%, p < 0.05), who were highly satisfied (86%).
Conclusion
Upper limb lymphedema can significantly impact work, sometimes upending careers. The rare workstation adaptations were beneficial. Occupational physicians should assess lymphedema-attributed difficulties to improve working conditions.
Similar content being viewed by others
References
DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14(6):500–515. https://doi.org/10.1016/S1470-2045(13)70076-7
Velanovich V, Szymanski W (1999) Quality of life of breast cancer patients with lymphedema. Am J Surg 177(3):184–188
Engel J, Kerr J, Schlesinger-Raab A, Eckel R, Sauer H, Hölzel D (2003) Predictors of quality of life of breast cancer patients. Acta Oncol 42(7):710–718
Pyszel A, Malyszczak K, Pyszel K, Andrzejak R, Szuba A (2006) Disability, psychological distress and quality of life in breast cancer survivors with arm lymphedema. Lymphology 39(4):185–192
Fu MR, Ridner SH, Stewart BR, Cormier JN, Armer JM (2013) Psychosocial impact of lymphedema: a systematic review of literature from 2004 to 2011. Psychooncology 22(7):1466–1484. https://doi.org/10.1002/pon.3201
Mehnert A (2011) Employment and work-related issues in cancer survivors. Crit Rev Oncol Hematol 77(2):109–130. https://doi.org/10.1016/j.critrevonc.2010.01.004
Fantoni SQ, Peugniez C, Duhamel A, Skrzypczak J, Frimat P, Leroyer A (2010) Factors related to return to work by women with breast cancer in northern France. J Occup Rehabil 20(1):49–58. https://doi.org/10.1007/s10926-009-9215-y
Boyages J, Kalfa S, Xu Y, Koelmeyer L, Mackie H, Viveros H, Taksa L, Gollan P (2016) Worse and worse off: the impact of lymphedema on work and career after breast cancer. Springerplus 5:657. https://doi.org/10.1186/s40064-016-2300-8 eCollection 2016
Lasinski BB, McKillip Thrift K, Squire D, Austin MK, Smith KM, Wanchai A, Green JM, Stewart BR, Cormier JN, Armer JM (2012) A systematic review of the evidence for complete decongestive therapy in the treatment of lymphedema from 2004 to 2011. PM R 4(8):580–601. https://doi.org/10.1016/j.pmrj.2012.05.00
Armer JM, Stewart BR (2005) A comparison of four diagnostic criteria for lymphedema in a post-breast cancer population. Lymphat Res Biol 3(4):208–217
International Society of Lymphology (2013) The diagnosis and treatment of peripheral lymphedema: 2013 consensus document of the International Society of Lymphology. Lymphology 46(4):1–11
Soran A, D’Angelo G, Begovic M, Ardic F, Harlak A, Samuel Wieand H, Vogel VG, Johnson RR (2006) Breast cancer-related lymphedema – what are the significant predictors and how they affect the severity of lymphedema? Breast J 12(6):536–543
Sitzia J (1995) Volume measurement in lymphoedema treatment: examination of formulae. Eur J Cancer Care 4(1):11–16
Galland C, Auvert JF, Flahault A, Vayssairat M (2002) Why and how post-mastectomy edema should be quantified in patients with breast cancer. Breast Cancer Res Treat 75(1):87–89
Hauglann B, Benth JŠ, Fosså SD, Dahl AA (2012) A cohort study of permanently reduced work ability in breast cancer patients. J Cancer Surviv 6(3):345–356. https://doi.org/10.1007/s11764-012-0215-0
Mock V (1998) Breast cancer and fatigue: issues for the workplace. AAOHN J 46(9):425–431
Maunsell E, Drolet M, Brisson J, Brisson C, Mâsse B, Deschênes L (2004) Work situation after breast cancer: results from a population-based study. J Natl Cancer Inst 96(24):1813–1822
Wang L, Hong BY, Kennedy SA, Chang Y, Hong CJ, Craigie S, Kwon HY, Romerosa B, Couban RJ, Reid S, Khan JS, McGillion M, Blinder V, Busse JW (2018) Predictors of unemployment after breast cancer surgery: a systematic review and meta-analysis of observational studies. J Clin Oncol 36(18):1868–1879. https://doi.org/10.1200/JCO.2017.77.3663
O’Toole JA, Ferguson CM, Swaroop MN, Horick N, Skolny MN, Brunelle CL, Miller CL, Jammallo LS, Specht MC, Taghian AG (2015) The impact of breast cancer-related lymphedema on the ability to perform upper extremity activities of daily living. Breast Cancer Res Treat 150(2):381–388. https://doi.org/10.1007/s10549-015-3325-3
Showalter SL, Brown JC, Cheville AL, Fisher CS, Sataloff D, Schmitz KH (2013) Lifestyle risk factors associated with arm swelling among women with breast cancer. Ann Surg Oncol 20(3):842–849. https://doi.org/10.1245/s10434-012-2631-9
Neubauer M, Schoberwalter D, Cenik F, Keilani M, Crevenna R (2017) Lymphedema and employability – review and results of a survey of Austrian experts. Wien Klin Wochenschr 129(5–6):186–191. https://doi.org/10.1007/s00508-017-1167-1
Belmonte R, Messaggi-Sartor M, Ferrer M, Pont A, Escalada F (2018) Prospective study of shoulder strength, shoulder range of motion, and lymphedema in breast cancer patients from pre-surgery to 5 years after ALND or SLNB. Support Care Cancer 26(9):3277–3287. https://doi.org/10.1007/s00520-018-4186-1
Timperi AW, Ergas IJ, Rehkopf DH, Roh JM, Kwan ML, Kushi LH (2013) Employment status and quality of life in recently diagnosed breast cancer survivors. Psychooncology 22(6):1411–1420. https://doi.org/10.1002/pon.3157
Paterson CL, Lengacher CA, Donovan KA, Kip KE, Tofthagen CS (2016) Body image in younger breast cancer survivors: a systematic review. Cancer Nurs 39(1):E39–E58. https://. https://doi.org/10.1097/NCC.0000000000000251
Chachaj A, Małyszczak K, Pyszel K, Lukas J, Tarkowski R, Pudełko M, Andrzejak R, Szuba A (2010) Physical and psychological impairments of women with upper limb lymphedema following breast cancer treatment. Psychooncology 19(3):299–305. https://doi.org/10.1002/pon.1573
Ridner SH (2005) Quality of life and a symptom cluster associated with breast cancer treatment-related lymphedema. Support Care Cancer 13(11):904–911
Taghian NR, Miller CL, Jammallo LS, O’Toole J, Skolny MN (2014) Lymphedema following breast cancer treatment and impact on quality of life: a review. Crit Rev Oncol Hematol 92(3):227–234. https://doi.org/10.1016/j.critrevonc.2014.06.004
Maxeiner S, Downer A (2009) Comparing the psychosocial issues experienced by individuals with primary vs secondary lymphedema. Rehab Oncol 27(2):9–15
Kennedy F, Haslam C, Munir F, Pryce J (2007) Returning to work following cancer: a qualitative exploratory study into the experience of returning to work following cancer. Eur J Cancer Care (Engl) 16(1):17–25
Kalfa S, Koelmeyer L, Taksa L, Winch C, Viveros H, Gollan PJ, Mackie H, Boyages J (2019) Work experiences of Australian cancer survivors with lymphoedema: a qualitative study. Health Soc Care Community. https://doi.org/10.1111/hsc.12698
Spelten ER, Sprangers MA, Verbeek JH (2002) Factors reported to influence the return to work of cancer survivors: a literature review. Psychooncology 11(2):124–131
Buijs P, van Amstel R, van Dijk F (1999) Dutch occupational physicians and general practitioners wish to improve cooperation. Occup Environ Med 56(10):709–713
Steiner JF, Cavender TA, Main DS, Bradley CJ (2004) Assessing the impact of cancer on work outcomes: what are the research needs? Cancer 101(8):1703–1711
Crevenna R (2019) Aspects of cancer rehabilitation: an Austrian perspective. Disabil Rehabil:1. https://doi.org/10.1080/09638288.2018.1522554
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vignes, S., Fau-Prudhomot, P., Simon, L. et al. Impact of breast cancer–related lymphedema on working women. Support Care Cancer 28, 79–85 (2020). https://doi.org/10.1007/s00520-019-04804-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04804-2