Abstract
Purpose
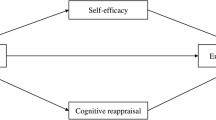
Patients newly diagnosed with cancer are often confronted with feelings of uncertainty and life threat. A significant proportion may report impairments in psychosocial well-being. Previous studies examining protective psychological factors such as hope and emotion regulation (ER) have yet to investigate these processes concurrently within a common self-regulation framework and/or focus on newly diagnosed patients. The present study aimed to examine how hope and ER may relate to psychosocial outcomes of patients newly diagnosed with cancer.
Methods
The present study used a cross-sectional design with self-report questionnaires. Participants were newly diagnosed patients (N = 101) recruited from three cancer therapy clinics in a hospital. Patients completed measures of hope, ER (cognitive reappraisal and expressive suppression), and psychosocial well-being (life satisfaction and negative affectivity).
Results
Findings showed that (1) hope and reappraisal, but not suppression, were associated with well-being and (2) the interaction between hope and reappraisal was associated with well-being; reappraisal was not associated with well-being in high hope patients, while high reappraisal was associated with better well-being in low hope patients.
Conclusion
Individual differences in hope and reappraisal appeared to be associated with psychosocial outcomes in newly diagnosed cancer patients. Hopeful thinking appeared to benefit patients’ psychosocial well-being. In addition, an interaction effect between hope and reappraisal suggested that reappraisal as an ER strategy may be particularly adaptive for patients with low hope.

Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63:11–30. doi:10.3322/caac.21166
Teo MCC, Khee CS (2013) Cancer trends and incidences in Singapore. Jpn J Clin Oncol 43(3):219–224. doi:10.1093/jjco/hys230
Rutten LF, Hesse BW, Moser RP, McCaul KD, Rothman AJ (2009) Public perceptions of cancer prevention, screening, and survival: comparison with state-of-science evidence for colon, skin, and lung cancer. J Cancer Educ 24(1):40–48. doi:10.1080/08858190802664610
Institute of Medicine (US), Committee on Psychosocial Services to Cancer Patients/Families in a Community Setting. (2008). Cancer care for the whole patient: meeting psychosocial health needs. Washington, DC: National Academies Press. Retrieved from: http://www.ncbi.nlm.nih.gov/books/NBK4011/
Carlson LE, Waller A, Groff SL, Giese-Davis J, Bultz BD (2013) What goes up does not always come down: patterns of distress, physical and psychological morbidity in people with cancer over a one year period. Psycho-Oncology 22(1):168–176. doi:10.1002/pon.2068
Institute of Medicine (US), & National Research Council. (2006). From cancer patient to cancer survivor: lost in transition. Washington, DC: National Academies Press
National Cancer Institute. (2004). Living beyond cancer: finding a new balance. President’s cancer panel 2003–2004 annual report. Department of Health and Human Services, National Institutes of Health. Retrieved February 12, 2014, from http://deainfo.nci.nih.gov/advisory/pcp/annualReports/pcp03-04rpt/Survivorship.pdf
Carlson LE, Bultz BD (2004) Efficacy and medical costs’ offset of psychosocial interventions in cancer care: making the case for economic analyses. Psycho-Oncology 13(12):837–849. doi:10.1002/pon.832
Jacobson PB (2007) Screening for psychological distress in cancer patients: challenges and opportunities. J Clin Oncol 25(29):4526–4527. doi:10.1200/JCO.2007.13.1367
National Comprehensive Cancer Network. (2012). NCCN Distress Management Clinical Practice Guidelines in Oncology. Retrieved February 12, 2014, from http://www.nccn.org
Ridner SH (2004) Psychological distress: concept analysis. J Adv Nurs 45(5):536–545. doi:10.1046/j.1365-2648.2003.02938.x
Hegel MT, Moore CP, Collins ED, Kearing S, Gillock KL, Riggs RL, Clay KF, Ahles TA (2006) Distress, psychiatric syndromes, and impairment of function in women with newly diagnosed breast cancer. Cancer 107(12):2924–2931. doi:10.1002/cncr.22335
Kangas M, Henry JL, Bryant RA (2002) Posttraumatic stress disorder following cancer: a conceptual and empirical review. Clin Psychol Rev 22(4):499–524. doi:10.1016/S0272-7358(01)00118-0
Yan H, Sellick K (2004) Symptoms, psychological distress, social support, and quality of life of Chinese patients newly diagnosed with gastrointestinal cancer. Cancer Nurs 27(5):389–399. doi:10.1097/00002820-200409000-00009
Folkman S (2013) Stress, coping, and hope. In: Carr BI, Steel J (eds) Psychological aspects of cancer. Springer, New York, NY, pp 119–127. doi:10.1007/978-1-4614-4866-2_8
Stanton AL, Danoff-Burg S, Cameron CL, Bishop M, Collins CA, Kirk SB, Sworowski LA, Twillman R (2000) Emotionally expressive coping predicts psychological and physical adjustment to breast cancer. J Consult Clin Psychol 68(5):875–882. doi:10.1037/0022-006X.68.5.875
Snyder CR, Irving L, Anderson JR (1991) Hope and health: measuring the will and the ways. In: Snyder CR, Forsyth DR (eds) Handbook of social and clinical psychology: the health perspective. Pegamon, Elmsford, NY, pp 285–305
Snyder CR (2002) Hope theory: rainbows in the mind. Psychol Inq 13(4):249–275. doi:10.1207/S15327965PLI1304_01
Irving LM, Snyder CR, Crowson JJ Jr (1998) Hope and coping with cancer by college women. J Pers 66(2):195–214. doi:10.1111/1467-6494.00009
Snyder CR, Sympson SC, Ybasco FC, Borders TF, Babyak MA, Higgins RL (1996) Development and validation of the State Hope Scale. J Pers Soc Psychol 70(2):321–335. doi:10.1037/0022-3514.70.2.321
Berendes D, Keefe FJ, Somers TJ, Kothadia SM, Porter LS, Cheavens JS (2010) Hope in the context of lung cancer: relationships of hope to symptoms and psychological distress. J Pain Symptom Manag 40(2):174–182. doi:10.1016/j.jpainsymman.2010.01.014
Blank TO, Bellizzi KM (2006) After prostate cancer: predictors of well-being among long-term prostate cancer survivors. Cancer 106(10):2128–2135. doi:10.1002/cncr.21865
Ai AL, Pargament KI, Appel HB, Kronfol Z (2010) Depression following open-heart surgery: a path model involving interleukin-6, spiritual struggle, and hope under preoperative distress. J Clin Psychol 66(10):1057–1075. doi:10.1002/jclp.20716
Billington E, Simpson J, Unwin J, Bray D, Giles D (2008) Does hope predict adjustment to end-stage renal failure and consequent dialysis? Br J Health Psychol 13(4):683–699. doi:10.1348/135910707X248959
Stanton AL, Danoff-Burg S, Huggins ME (2002) The first year after breast cancer diagnosis: hope and coping strategies as predictors of adjustment. Psycho-Oncology 11(2):93–102. doi:10.1002/pon.574
Gross JJ, John OP (2003) Individual differences in two emotion regulation processes: implication for affect, relationships, and well-being. J Pers Soc Psychol 85(2):348–362. doi:10.1037/0022-3514.85.2.348
Gross JJ, Richards JM, John OP (2006) Emotion regulation in everyday life. In: Snyder DK, Simpson JA, Hughes JN (eds) Emotion regulation in families: pathways to dysfunction and health. American Psychological Association, Washington DC, pp 13–35
Gross JJ (1998) Antecedent- and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. J Pers Soc Psychol 74(1):224–237. doi:10.1037/0022-3514.74.1.224
John OP, Gross JJ (2004) Healthy and unhealthy emotion regulation: personality processes, individual differences, and life span development. J Pers 72(6):1301–1333. doi:10.1111/j.1467-6494.2004.00298.x
Gilanders S, Wild M, Deighan C, Gillanders D (2008) Emotion regulation, affect, psychosocial functioning, and well-being in hemodialysis patients. Am J Kidney Dis 51(4):651–662. doi:10.1053/j.ajkd.2007.12.023
Karademas EC, Tsalikou C, Tallarou MC (2011) The impact of emotion regulation and illness-focused coping strategies on the relation of illness-related negative emotions to subjective health. J Health Psychol 16(3):510–519. doi:10.1177/1359105310392093
Schroevers M, Kraaij V, Garnefski N (2008) How do cancer patients manage unattainable personal goals and regulate their emotions? Br J Health Psychol 13(Pt 3):551–562. doi:10.1348/135910707X241497
Schlatter MC, Cameron LD (2010) Emotional suppression tendencies as predictors of symptoms, mood, and coping appraisals during AC chemotherapy for breast cancer treatment. Ann Behav Med 40(1):15–29. doi:10.1007/s12160-010-9204-6
Urry HL (2009) Using reappraisal to regulate unpleasant emotional episodes: goals and timing matter. Emotion 9(6):782–797. doi:10.1037/a0017109
McRae K, Ciesielski B, Gross J (2012) Unpacking cognitive reappraisal: goals, tactics, and outcomes. Emotion 12(2):250–255. doi:10.1037/a0026351
Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K (1991) The Edmonton Symptom Assessment System (ESAS): a simple method of the assessment of palliative care patients. J Palliat Care 7(2):6–9
Snyder CR, Harris C, Anderson JR, Holleran SA, Irving LM, Sigmon ST, Yoshinobu L, Gibb J, Langelle C, Harney P (1991) The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol 60(4):570–585. doi:10.1037/0022-3514.60.4.570
Diener E, Emmons RA, Larsen RJ, Griffin S (1985) The Satisfaction with Life Scale. J Pers Assess 49(1):71–75
Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
Hayes AF (2013) Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford Press, New York, NY
Aiken LS, West SG (1991) Multiple regression: testing and interpreting interactions. Sage Publications, Thousand Oaks, CA
Hayes AF, Matthes J (2009) Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behav Res Methods 41(3):924–936. doi:10.3758/BRM.41.3.924
Hirokawa K, Nagata C, Takatsuka N, Shimizu H (2004) The relationships of a rationality/antiemotionality personality scale to mortalities of cancer and cardiovascular disease in a community population in Japan. J Psychosom Res 56(1):103–111. doi:10.1016/S0022-3999(03)00046-1
Kruijver IPM, Garssen B, Visser AP, Kuiper AJ (2006) Signalising psychosocial problems in cancer care: the structural use of a short psychosocial checklist during medical or nursing visits. Patient Educ Couns 62(2):163–177. doi:10.1016/j.pec.2005.10.001
Garnefski N, Kraaij V, Spinhoven P (2001) Negative life events, cognitive emotion regulation, and emotional problems. Personal Indicid Differ 30(8):1311–1327. doi:10.1016/S0191-8869(00)00113-6
Acknowledgments
We would like to thank Professor George Bishop for his inputs on emotion regulation and research assistants for helping with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Peh, C.X., Kua, E.H. & Mahendran, R. Hope, emotion regulation, and psychosocial well-being in patients newly diagnosed with cancer. Support Care Cancer 24, 1955–1962 (2016). https://doi.org/10.1007/s00520-015-2989-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2989-x