Abstract
Purpose
To compare the short-term and oncologic outcomes of patients with pancreatic ductal adenocarcinoma (PDAC) undergoing laparoscopic distal pancreatectomy (LDP) and open distal pancreatectomy (ODP).
Methods
Consecutive cases of distal pancreatectomy (DP) (n = 422) were reviewed at a single high-volume institution over a 10-year period (2005–2014). Inclusion criteria consisted of any patient with PDAC by surgical pathology. Ninety-day outcomes were monitored through a prospectively maintained pancreatic resection database. The Social Security Death Index was used for 5-year survival. Two-way statistical analyses were used to compare categories; variance was reported with standard error of the mean; * indicates P value <0.05.
Results
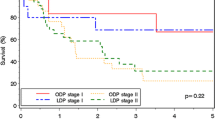
Seventy-nine patients underwent DP for PDAC. Thirty-three underwent LDP and 46 ODP. There were no statistical differences in demographics, BMI, and ASA classification. Intraoperative and surgical pathology variables were comparable for LDP versus ODP: operative time (3.9 ± 0.2 vs. 4.2 ± 0.2 h), duct size, gland texture, stump closure, tumor size (3.3 ± 0.3 vs. 4.0 ± 0.4 cm), lymph node harvest (14.5 ± 1.1 vs. 17.5 ± 1.2), tumor stage (see table), and negative surgical margins (77 vs. 87%). Patients who underwent LDP experienced lower blood loss (310 ± 68 vs. 597 ± 95 ml; P = 0.016*) and required fewer transfusions (0 vs. 13; P = 0.0008*). Patients who underwent LDP had fewer positive lymph nodes (0.8 ± 0.2 vs. 1.6 ± 0.3; P = 0.04*) and a lower incidence of type C pancreatic fistula (0 vs. 13%; P = 0.03*). Median follow-up for all patients was 11.4 months. Long-term oncologic outcomes revealed similar outcomes including distant or local recurrence (30 vs. 52%; P = 0.05) and median survival (18 vs. 15 months), as well as 1-year (73 vs. 59%), 3-year (22 vs. 21%), and 5-year (20 vs. 15%) survival for LDP and ODP, respectively.
Conclusions
The results of this series suggest that LDP is a safe surgical approach that is comparable from an oncologic standpoint to ODP for the management of pancreatic adenocarcinoma.

Similar content being viewed by others
Abbreviations
- ACS-NSQIP:
-
American College of Surgeons National Surgical Quality Improvement Program
- DP:
-
Distal pancreatectomy
- PDAC:
-
Pancreatic adenocarcinoma
- PF:
-
Pancreatic fistula
References
Sharpe SM, Talamonti MS, Wang E, Bentrem DJ, Roggin KK, Prinz RA, Marsh RDW, Stocker SJ, Winchester DJ, Baker MS (2015) The laparoscopic approach to distal pancreatectomy for ductal adenocarcinoma results in shorter lengths of stay without compromising oncologic outcomes. Am J Surg 209:557–663
Shin SH, Kim SC, Song KB, Hwang DW, Lee JH, Lee D, Lee JW, Jun E, Park KM, Lee YJ (2015) A comparative study of laparoscopic vs open distal pancreatectomy for left-sided ductal adenocarcinoma: a propensity score-matched analysis. J Am Coll Surg 220:177–185
Baker MS, Bentrem DJ, Ujiki MB, Stocker SS, Talamonti MS (2009) A prospective single institution comparison of peri-operative outcomes for laparoscopic and open distal pancreatectomy. Surgery 146:635–643
Sui CJ, Li B, Yang JM, Wang SJ, Zhou YM (2012) Laparoscopic versus open distal pancreatectomy: a meta-analysis. Asian J Surg 35:1–8
Limongelli P, Belli A, Russo G, Cioffi L, D’Agostino A, Fantini C, Belli G (2012) Laparoscopic and open surgical treatment of left-sided pancreatic lesions: clinical outcomes and cost-effectiveness analysis. Surg Endosc 26:1830–1836
Piessen G, Lefevre JH, Cabau M, Duhamal A, Behal H, Perniceni T, Mabrut JY, Regimbeau JM, Bonvalot S, Tiberio GA, Mathonnet M, Regenet N, Guillaud A, Glehen O, Mariani P, Denost Q, Maggiori L, Benhaim L, Manceau G, Mutter D, Bail JP, Meunier B, Porcheron J, Mariette C, Brigand C, AFC and the FREGAT working group, (2015) Laparoscopic versus open surgery for gastric gastrointestinal stromal tumors: what is the impact on postoperative outcome and oncologic results? Ann Surg 262:831–839
Siani LM, Ferranti F, De Carlo A, Quintiliani A (2012) Completely laparoscopic versus open total gastrectomy in stage I-III/C gastric cancer: safety, efficacy and five-year oncologic outcome. Minerva Chir 67:319–326
Siani LM, Ferranti F, Benedetti M, De Carlo A, Quintiliani A (2011) Laparoscopic versus open radical nephrectomy in T1-T2 renal carcinoma: personal 5-year experience about the oncologic outcome. Minerva Chir 66:317–326
The Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Kooby DA (2006) Laparoscopic surgery for cancer: historical, theoretical, and technical considerations. Oncology 20:317–326
Kim SC, Park KT, Hwang JW, Shin HC, Lee SS, Seo DW, Lee SK, Kim MH, Han DK (2008) Comparative analysis of clinical outcomes for laparoscopic distal pancreatic resection and open distal pancreatic resection at a single institution. Surg Endosc 22:2261–2268
Kooby DA, Gillespie T, Bentrem D, Nakeeb A, Schmidt MC, Merchant NB, Parikh AA, Martin RCG, Scoggins CR, Ahmad S, Kim JH, Park JR, McClaine R, Strasberg SM, Talamonti MS, Staley CA, McMasters KM, Lowy AM, Byrd-Sellers J, Wood WC, Hawkins WG (2008) Left-sided pancreatectomy: a multicenter comparison of laparoscopic and open approaches. Ann Surg 248:438–446
Rooij TD, Jilesen AP, Boerma D, Bonsing BA, Bosscha K, van Dam RM, van Dieren S, Dijkgraaf MG, van Eijck CH, Gerhards MF, van Goor H, van der Harst E, de Hingh IH, Kazemier G, Klaase JM, Molenaar IQ, van Dijkum EJN, Patijn GA, van Santvoort HC, Scheepers JJ, van der Schelling GP, Sieders E, Vogel JA, Busch OR, Besselink MG (2015) A nationwide comparison of laparoscopic and open distal pancreatectomy for benign and malignant disease. J Am Coll Surg 220:263–270
Zhang Y, Chen XM, Sun DL (2014) Laparoscopic versus open distal pancreatectomy: a single-institution comparative study. World J Surg Oncol 12:327
Ceppa EP, McCurdy RM, Becerra DC, Kilbane EM, Zyromski NJ, Nakeeb A, Schmidt CM, Lillemoe KD, Pitt HA, House MG (2015) Does pancreatic stump closure method influence distal pancreatectomy outcomes? J Gastrointest Surg 19:1449–1456
Khuri SF (2005) The NSQIP: a new frontier in surgery. Surgery 138:837–843
Fink AS, Campbell DA, Mentzer RM, Henderson WG, Daley J, Bannister J, Hur K, Khuri SF (2002) The national surgical quality improvement program in non-veterans administration hospitals: initial demonstration of feasibility. Ann Surg 236:344–353
Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA, Fink AS, Mentzer RM, Steeger JE (2007) The patient safety in surgery study: background, study design, and patient populations. J Am Coll Surg 204:1089–1102
Daley J, Khuri SF, Henderson W, Hur K, Gibbs JO, Barbour G, Demakis J, Irvin G 3rd, Stremple JF, Grover F, McDonald G, Passaro E Jr, Fabri PJ, Spencer J, Hammermeister K, Aust JB, Oprian C (1997) Risk adjustment of the postoperative morbidity rate for the comparative assessment of the quality of surgical care: result of the national veterans affairs surgical risk study. J Am Coll Surg 185:328–340
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Casadei R, Ricci C, Pezzilli R, Calculli L, D’Ambra M, Taffurelli G, Minni F (2011) Assessment of complications according to the Clavien-Dindo classification after distal pancreatectomy. J Pancreas 12:126–130
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Khaled YS, Malde DJ, Packer J, De Liguori Carino N, Deshpande R, O’Reilly DA, Sherlock DJ, Ammori BJ (2014) A case-matched comparative study of laparoscopic versus open distal pancreatectomy. Surg Laparosc Endosc 25:363–367
Vijan SS, Ahmed KA, Harmsen WS, Que FG, Reid-Lombardo KM, Nagorney DM, Donohue JH, Farnell MB, Kendrick ML (2010) Laparoscopic vs open distal pancreatectomy a single-institution comparative study. Arch Surg 45:616–621
Kooby DA, Hawkins WG, Schmidt CM, Weber SM, Bentrem DJ, Gillespie TW, Sellers JB, Merchant NB, Scoggins CR, Martin RCG, Kim HJ, Ahmed S, Cho CS, Parikh AA, Chu CK, Hamilton NA, Doyle CJ, Pinchot S, Hayman A, McClaine R, Nakeeb A, Staley CA, McMasters KM, Lillemoe KD (2010) A multicenter analysis of distal pancreatectomy for adenocarcinoma: is laparoscopic resection appropriate? J Am Coll Surg 210:779–787
Kagedan DJ, Raju RS, Dixon ME, Shin E, Li Q, Liu N, Elmi M, El-Sedfy A, Paszat L, Kiss A, Earle CC, Mittmann N, Coburn NG (2016) The association of adjuvant therapy with survival at the population level following pancreatic adenocarcinoma resection. HPB 18:339–347
Katz MHG, Shi Q, Ahmad SA, Herman JM, de Wilton Marsh R, Collisson EA, Schwartz LH, Martin RCG, Conway WC, Truty M, Kindler HL, Lowy AM, Philip PA, Sekaii-Saab TS, Cardin BD, LoConte NK, Venook AP (2015) Preoperative modified FOLFIRINOX (mFOLFIRINOX) followed by chemoradiation (CRT) for borderline resectable (BLR) pancreatic cancer (PDAC): initial results from Alliance Trial A021101. J Clin Oncol 33:4008
Fernandez-Cruz L, Cosa R, Blanco L, Levi S, Lopez-Boado MA, Navarro S (2007) Curative laparoscopic resection for pancreatic neoplasms: a critical analysis from a single institution. J Gastrointest Surg 11:1607–1621
Kang CM, Choi SH, Hwang HK, Kim DH, Yoon CI, Lee WJ (2010) Laparoscopic distal pancreatectomy with division of the pancreatic neck for benign and borderline malignant tumor in the proximal body of the pancreas. J Laparoendosc Adv Surg Tech A 20:581–586
Song KB, Kim SC, Park JB, Kim YH, Jung YS, Kim MH, Lee SK, Seo DW, Lee SS, Park DH (2011) Single-center experience of laparoscopic left pancreatic resection in 359 consecutive patients: changing the surgical paradigm of left pancreatic resection. Surg Endosc 25:3364–3372
Mehta SS, Doumane G, Mura T, Nocca D, Fabre JM (2012) Laparoscopic versus open distal pancreatectomy: a single-institution case-control study. Surg Endosc 26:402–707
Rehman S, John SKP, Lochan R, Jaques BC, Manas DM, Charnley RM, French JJ, White SA (2014) Oncological feasibility of laparoscopic distal pancreatectomy for adenocarcinoma: a single-institution comparative study. World J Surg 38:476–483
Magge D, Gooding W, Choudry H, Steve J, Steel J, Zureikat A, Krasinskas A, Daouadi M, Lee KK, Hughes SJ, Zeh HJ 3rd, Moser AJ (2013) Comparative effectiveness of minimally invasive open distal pancreatectomy for ductal adenocarcinoma. JAMA Surg 148:525–531
Acknowledgements
There are no financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Marita D. Bauman, David G. Becerra, E. Molly Kilbane, RN BSN, Nicholas J. Zyromski, C. Max Schmidt, Henry A. Pitt, Attila Nakeeb, Michael G. House, and Eugene P. Ceppa have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Bauman, M.D., Becerra, D.G., Kilbane, E.M. et al. Laparoscopic distal pancreatectomy for pancreatic cancer is safe and effective. Surg Endosc 32, 53–61 (2018). https://doi.org/10.1007/s00464-017-5633-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5633-7