Abstract
Background
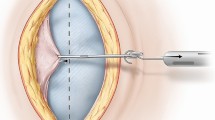
During hiatal hernia repair there are two vectors of tension: axial and radial. An optimal repair minimizes the tension along these vectors. Radial tension is not easily recognized. There are no simple maneuvers like measuring length that facilitate assessment of radial tension. The aims of this project were to: (1) establish a simple intraoperative method to evaluate baseline tension of the diaphragmatic hiatal muscle closure; and, (2) assess if tension is reduced by relaxing maneuvers and if so, to what degree.
Methods
Diaphragmatic characteristics and tension were assessed during hiatal hernia repair with a tension gage. We compared tension measured after hiatal dissection and after relaxing maneuvers were performed.
Results
Sixty-four patients (29 M:35F) underwent laparoscopic hiatal hernia repair. Baseline hiatal width was 2.84 cm and tension 13.6 dag. There was a positive correlation between hiatal width and tension (r = 0.55) but the strength of association was low (r 2 = 0.31). Four different hiatal shapes (slit, teardrop, “D”, and oval) were identified and appear to influence tension and the need for relaxing incision. Tension was reduced by 35.8 % after a left pleurotomy (12 patients); by 46.2 % after a right crural relaxing incision (15 patients); and by 56.1 % if both maneuvers were performed (6 patients).
Conclusions
Tension on the diaphragmatic hiatus can be measured with a novel device. There was a limited correlation with width of the hiatal opening. Relaxing maneuvers such as a left pleurotomy or a right crural relaxing incision reduced tension. Longer term follow-up will determine whether outcomes are improved by quantifying and reducing radial tension









Similar content being viewed by others
References
Huntington TR (1997) Laparoscopic mesh repair of the esophageal hiatus. J Am Coll Surg 184(4):399–400
Greene CL, DeMeester SR, Zehetner J, Worrell SG, Oh DS, Hagen JA (2013) Diaphragmatic relaxing incisions during laparoscopic paraesophageal hernia repair. Surg Endosc 27:4532–4538
Louie BE, Blitz M, Farivar AS, Orlina J, Aye RW (2011) Repair of symptomatic giant paraesophageal hernias in elderly (>70 years) patients results in improved quality of life. J Gastrointest Surg 15:389–396
Qureshi AP, Aye RW, Buduhan G, Knight A, Orlina J, Farivar AS, Wagner OJ, McHugh S, Louie BE (2013) The laparoscopic Nissen-Hill hybrid: pilot study of a combined antireflux procedure. Surg Endosc 27:1945–1952
Oelschlager BK, Pellegrini CA, Hunter JG, Brunt ML, Soper NJ, Sheppard BC, Polissar NL, Neradilek MB, Mitsumori LM, Rohrmann CA, Swanstrom LL (2011) Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg 213:461–468
Granderath FA, Schweiger UM, Pointner R (2007) Laparoscopic antireflux surgery: tailoring the hiatal closure to the size of hiatal surface area. Surg Endosc 21:542–548
DeMeester TR, Bonavina L, Albertucci M (1986) Nissen fundoplication for gastroesophageal reflux disease. Evaluation of primary repair in 100 consecutive patients. Ann Surg 204:9–20
Luketich JD, Raja S, Fernando HC, Campbell W, Christie NA, Buenaventura PO, Weigel TL, Keenan RJ, Schauer PR (2000) Laparoscopic repair of giant paraesophageal hernia: 100 consecutive cases. Ann Surg 232:608–618
Oelschlager BKI, Pellegrini CA, Hunter J, Soper N, Brunt M, Sheppard B, Jobe B, Polissar N, Mitsumori L, Nelson J, Swanstrom L (2006) Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg 244:481–490
Marcus DR, Lau WM, Swanstrom LL (1996) Carbon dioxide pneumothorax in laparoscopic surgery. Am J Surg 171:464–466
Disclosures
Daniel Davila Bradley, Candice L. Wilshire, Peter Baik, Alexander S. Farivar, and Ralph W. Aye have no conflict of interest. Brian E. Louie reports a relationship with Torax Medical Incorporated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bradley, D.D., Louie, B.E., Farivar, A.S. et al. Assessment and reduction of diaphragmatic tension during hiatal hernia repair. Surg Endosc 29, 796–804 (2015). https://doi.org/10.1007/s00464-014-3744-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3744-y