Abstract
Background
The open tension-free mesh-plug hernia technique, transabdominal preperitoneal (TAPP) technique, and totally extraperitoneal (TEP) laparoscopic technique all are common surgical procedures for primary unilateral inguinal hernia repair. However, the choice of the right surgical procedure still is controversial in China. This study aimed to compare open tension-free hernioplasty with two laparoscopic hernia repairs.
Methods
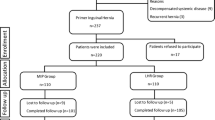
In this study, 164 male patients with primary unilateral inguinal hernia were randomized to undergo an open operation with mesh-plug and patch, TAPP, or TEP.
Results
Completion of the study required 3 years, from February 2006 to February 2009. Of the 164 patients, 62 underwent open repair, 50 had TAPP, and 52 had TEP. The patients then were followed up for 15.6 ± 8.5 months. The average operating time for the open repair group was significantly shorter than for the other two groups (p < 0.001). The cost for the open repair group also was significantly less than for the other two groups (p < 0.001). By contrast, the pain scores in the open mesh group were significantly higher than in the other two groups (p < 0.001). The hospital stay and the recovery time both were significantly longer in open repair group than in the other two groups (p < 0.001). No major complications or recurrence was found in any of the groups.
Conclusions
The findings show that open tension-free mesh-plug hernia repair, TAPP, and TEP are safe and effective for patients with primary unilateral inguinal hernia. Both TAPP and TEP are superior to open repair in terms of less postoperative pain and faster recovery time. The authors therefore recommend laparoscopic repair techniques as the preferable choice of surgical procedure. However, they think open repair will remain a practical solution in China because of its lower cost, short learning period, and need for no special equipment.
Similar content being viewed by others
References
Pavlids TE (2010) Current opinion on laparoscopic repair of inguinal hernia. Surg Endosc 24:974–976
Rutkow IM, Robbins AW (1993) “Tension- free” inguinal herniorrhaphy: a preliminary report on the “mesh plug” technique. Surgery 114:3–8
Rutkow IM, Robbins AW (1998) Classification system and groin hernia. Surg Clin North Am 78:1117–1127
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Vale L, Ludbrook A, Grant A (2003) Assessing the costs and consequences of laparoscopic vs open methods of groin hernia repair: a systematic review. Surg Endosc 17:844–849
Dulucq J-L, Wintringer P, Mahajna (2009) Laparoscopic totally extraperitoneal inguinal hernia repair: lessons learned from 3, 100 hernia repairs over 15 years. Surg Endosc 23:482–486
Eklund AS, Montgomery AK, Rasmussen IC, Sandbue RP, Bergkvist LÅ, Rudberg CR (2009) Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair. Ann Surg 249:33–38
Arregui ME, Young SB (2005) Groin hernia repair by laparoscopic techniques: current status and controversies. World J Surg 29:1052–1057
Schmedt CG, Sauerland S, Bittner R (2005) Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trail. Surg Endosc 19:188–199
O’Dyer PJ (2004) Current status of the debate on laparoscopic hernia repair. Br Med Bull 70:105–118
Pikoulis E, Daskalakis P, Psallidas N, Karavokyros I, Stathoulopolos A, Godevenos D, Leppaniemi A, Tsatsoulis P (2005) Marlex Mesh Prefix Plug hernioplasty: retrospective analysis of 865 operations. World J Surg 29:231–234
Butler RE, Burke B, Schneider JJ, Brar H, Lucha PA Jr (2007) The economic impact of laparoscopic inguinal hernia repair: results of a double-blinded, prospective, randomized trial. Surg Endosc 21:387–390
Reuben B, Neumayer L (2006) Surgical management of inguinal hernia. Adv Surg 40:299–317
Johansson B, Hallerbäck B, Glise H, Anesten B, Smedberg S, Román J (1999) Laparoscopic mesh versus open preperitoneal mesh versus conventional technique for inguinal hernia repair. Ann Surg 230:225–231
Zieren J, Hoksch B, Wenger FA, Opitz I, Müller JM (2001) Inguinal hernia repair in new millennium: plug and patch repair with local anesthesia. World J Surg 25:138–141
van der Pool AEM, Harlaar JJ, den Hoed PT, Weidema WF, van Veen RN (2010) Long-term follow-up evaluation of chronic pain after endoscopic total extraperitoneal repair of primary and recurrent inguinal hernia. Surg Endosc. Published online 7 January
Kocijan R, Sandberg S, Chan Y-W, Hollinsky C (2010) Anatomical changes after inguinal hernia treatment: a reason for chronic pain and recurrent hernia? Surg Endosc 24:395–399
van Veen RN, Wijsmuller AR, Vrijland WW, Hop WC, Lange JF, Jeekel J (2007) Randomized clinical trial of mesh versus nonmesh primary inguinal hernia repair: long-term chronic pain at 10 years. Surgery 142:695–698
Fei L, Filippone G, Trapani V, Cuttitta D, lannuzzi E, lannuzzi M, Galizia G, Moccia F, Signoriello G (2006) Feasibility of primary inguinal hernia repair with a new mesh. World J Surg 30:1055–1062
Sanders DL, Samarakoon DH, Ganshirt SW, Porter CS, Kingsnorth AN (2009) A two-centre blinded randomized control study comparing the Lichtenstein patch, Perfix plug and ProLoop plug in the repair of primary inguinal hernia. Hernia 13:499–503
Disclosures
Ke Gong, Nengwei Zhang, Yiping LU, Bin Zhu, Zhanzhi Zhang, Dexiao Du, Xia Zhao, and Haijun Jiang have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gong, K., Zhang, N., Lu, Y. et al. Comparison of the open tension-free mesh-plug, transabdominal preperitoneal (TAPP), and totally extraperitoneal (TEP) laparoscopic techniques for primary unilateral inguinal hernia repair: a prospective randomized controlled trial. Surg Endosc 25, 234–239 (2011). https://doi.org/10.1007/s00464-010-1165-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1165-0