Abstract
Purpose
To determine which indicators, anatomical nodal metastasis (Japan Pancreas Society, JPS), number of positive lymph nodes (PLN), or lymph node ratio (LNR), is the best means of assessing lymph node involvement in pancreatic cancer.
Methods
This retrospective study analyzed 275 patients with pancreatic cancer treated at a single institution. Survival curves according to the JPS, PLN, or LNR were assessed by the Kaplan–Meier method. Prognostic value of each classification was explored by Cox regression analysis after adjustments for clinical factors.
Results
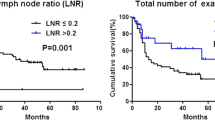
Multivariate analysis showed that, relative to n0 in the JPS, hazard ratios (HR) in n1, n2, and n3 were 1.72, 1.73, and 2.75, respectively, with no difference in survival between n1 and n2. Relative to PLN of 0, the HR in the PLN categories of 1∼2, 3, and >3 were 1.39, 1.65, and 3.03, respectively. Relative to LNR of 0, the HR in the categories of 0 < LNR ≤ 0.1, 0.1 < LNR ≤ 0.2, and LNR > 0.2 were 1.27, 2.00, and 5.58, respectively. An incremental increase in the HR was observed as the LNR category progressed, and differences between the survivals were distinct when stratified by the LNR.
Conclusions
The LNR was an accurate predictor of survival among three assessment strategies and could be proposed as a candidate for use as N categories, pending validation studies.




Similar content being viewed by others
References
Lim JE, Chien MW, Earle CC (2003) Prognostic factors following curative resection for pancreatic adenocarcinoma: a population-based, linked database analysis of 396 patients. Ann Surg 237:74–85
Brennan MF, Kattan MW, Klimstra D, Conlon K (2004) Prognostic nomogram for patients undergoing resection for adenocarcinoma of the pancreas. Ann Surg 240:293–298
Wagner M, Redaelli C, Lietz M, Seiler CA, Friess H, Buchler MW (2004) Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br J Surg 91:586–594
Japanese Gastric Cancer A (2011) Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 14:101–112
Society JP (2011) Classification of pancreatic carcinoma, Third English Editionth edn. Kanehara & Co., Ltd., Tokyo
Smith DD, Schwarz RR, Schwarz RE (2005) Impact of total lymph node count on staging and survival after gastrectomy for gastric cancer: data from a large US-population database. J Clin Oncol 23:7114–7124
Ludwig MS, Goodman M, Miller DL, Johnstone PA (2005) Postoperative survival and the number of lymph nodes sampled during resection of node-negative non-small cell lung cancer. Chest 128:1545–1550
International Union Against Cancer (2009) TNM classification of malignant tumors, Vol 7th edn. Wiley-Blackwell, New York
Bando E, Yonemura Y, Taniguchi K, Fushida S, Fujimura T, Miwa K (2002) Outcome of ratio of lymph node metastasis in gastric carcinoma. Ann Surg Oncol 9:775–784
Marchet A, Mocellin S, Ambrosi A, Morgagni P, Garcea D, Marrelli D et al (2007) The ratio between metastatic and examined lymph nodes (N ratio) is an independent prognostic factor in gastric cancer regardless of the type of lymphadenectomy: results from an Italian multicentric study in 1853 patients. Ann Surg 245:543–552
Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ et al (2003) Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol 21:2912–2919
Wang J, Hassett JM, Dayton MT, Kulaylat MN (2008) Lymph node ratio: role in the staging of node-positive colon cancer. Ann Surg Oncol 15:1600–1608
Petrelli F, Borgonovo K, Barni S (2011) The emerging issue of ratio of metastatic to resected lymph nodes in gastrointestinal cancers: an overview of literature. Eur J Surg Oncol 37:836–847
Hida J, Okuno K, Yasutomi M, Yoshifuji T, Matsuzaki T, Uchida T et al (2005) Number versus distribution in classifying regional lymph node metastases from colon cancer. J Am Coll Surg 201:217–222
Nakao A, Takagi H (1993) Isolated pancreatectomy for pancreatic head carcinoma using catheter bypass of the portal vein. Hepatogastroenterology 40:426–429
Nakao A, Takeda S, Inoue S, Nomoto S, Kanazumi N, Sugimoto H et al (2006) Indications and techniques of extended resection for pancreatic cancer. World J Surg 30:976–982
Murakami Y, Uemura K, Sudo T, Hayashidani Y, Hashimoto Y, Nakashima A et al (2010) Number of metastatic lymph nodes, but not lymph node ratio, is an independent prognostic factor after resection of pancreatic carcinoma. J Am Coll Surg 211:196–204
Massucco P, Ribero D, Sgotto E, Mellano A, Muratore A, Capussotti L (2009) Prognostic significance of lymph node metastases in pancreatic head cancer treated with extended lymphadenectomy: not just a matter of numbers. Ann Surg Oncol 16:3323–3332
Pomianowska E, Westgaard A, Mathisen O, Clausen OP, Gladhaug IP (2013) Prognostic relevance of number and ratio of metastatic lymph nodes in resected pancreatic, ampullary, and distal bile duct carcinomas. Ann Surg Oncol 20:233–241
Berger AC, Watson JC, Ross EA, Hoffman JP (2004) The metastatic/examined lymph node ratio is an important prognostic factor after pancreaticoduodenectomy for pancreatic adenocarcinoma. Am Surg 70:235–240
Pawlik TM, Gleisner AL, Cameron JL, Winter JM, Assumpcao L, Lillemoe KD et al (2007) Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery 141:610–618
Slidell MB, Chang DC, Cameron JL, Wolfgang C, Herman JM, Schulick RD et al (2008) Impact of total lymph node count and lymph node ratio on staging and survival after pancreatectomy for pancreatic adenocarcinoma: a large, population-based analysis. Ann Surg Oncol 15:165–174
Nakao A, Harada A, Nonami T, Kaneko T, Murakami H, Inoue S et al (1995) Lymph node metastases in carcinoma of the head of the pancreas region. Br J Surg 82:399–402
Nakao A, Harada A, Nonami T, Kaneko T, Nomoto S, Koyama H et al (1997) Lymph node metastasis in carcinoma of the body and tail of the pancreas. Br J Surg 84:1090–1092
Yamada S, Nakao A, Fujii T, Sugimoto H, Kanazumi N, Nomoto S et al (2009) Pancreatic cancer with paraaortic lymph node metastasis: a contraindication for radical surgery? Pancreas 38:e13–e17
Schwarz RE, Smith DD (2006) Extent of lymph node retrieval and pancreatic cancer survival: information from a large US population database. Ann Surg Oncol 13:1189–1200
House MG, Gonen M, Jarnagin WR, D’Angelica M, DeMatteo RP, Fong Y et al (2007) Prognostic significance of pathologic nodal status in patients with resected pancreatic cancer. J Gastrointest Surg 11:1549–1555
Malleo G, Maggino L, Capelli P, Gulino F, Segattini S, Scarpa A et al (2015) Reappraisal of nodal staging and study of lymph node station involvement in pancreaticoduodenectomy with the standard International Study Group of Pancreatic Surgery definition of lymphadenectomy for cancer. J Am Coll Surg 221:367–379
Strobel O, Hinz U, Gluth A, Hank T, Hackert T et al (2015) Pancreatic adenocarcinoma: number of positive nodes allows to distinguish several N categories. Ann Surg 261:961–969
Basturk O, Saka B, Balci S, Postlewait LM, Knight J, Goodman M et al (2015) Substaging of lymph node status in resected pancreatic ductal adenocarcinoma has strong prognostic correlations: proposal for a revised N classification for TNM Staging. Ann Surg Oncol 22:1187–1195
Mariette C, Piessen G, Briez N, Triboulet JP (2008) The number of metastatic lymph nodes and the ratio between metastatic and examined lymph nodes are independent prognostic factors in esophageal cancer regardless of neoadjuvant chemoradiation or lymphadenectomy extent. Ann Surg 247:365–371
Schiffman SC, McMasters KM, Scoggins CR, Martin RC, Chagpar AB (2011) Lymph node ratio: a proposed refinement of current axillary staging in breast cancer patients. J Am Coll Surg 213:45–52
Cheng GZ, Zhang WZ, Sun M, Wang Q, Coppola D, Mansour M et al (2008) Twist is transcriptionally induced by activation of STAT3 and mediates STAT3 oncogenic function. J Biol Chem 283:14665–14673
Pedrazzoli S, DiCarlo V, Dionigi R, Mosca F, Pederzoli P, Pasquali C et al (1998) Standard versus extended lymphadenectomy associated with pancreatoduodenectomy in the surgical treatment of adenocarcinoma of the head of the pancreas: a multicenter, prospective, randomized study. Lymphadenectomy Study Group. Ann Surg 228:508–517
Yeo CJ, Cameron JL, Lillemoe KD, Sohn TA, Campbell KA, Sauter PK et al (2002) Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma, part 2: randomized controlled trial evaluating survival, morbidity, and mortality. Ann Surg 236:355–366
Nimura Y, Nagino M, Takao S, Takada T, Miyazaki K, Kawarada Y et al (2012) Standard versus extended lymphadenectomy in radical pancreatoduodenectomy for ductal adenocarcinoma of the head of the pancreas: long-term results of a Japanese multicenter randomized controlled trial. J Hepatobiliary Pancreat Sci 19:230–241
Adsay NV, Basturk O, Altinel D, Khanani F, Coban I, Weaver DW et al (2009) The number of lymph nodes identified in a simple pancreatoduodenectomy specimen: comparison of conventional vs orange-peeling approach in pathologic assessment. Mod Pathol 22:107–112
Edge SB BD, Compton CC, Fritz AG, Green FL, Trotti A (eds) (2010) AJCC cancer staging manual, Vol 7th edn. Springer, Chicago
Valsangkar NP, Bush DM, Michaelson JS, Ferrone CR, Wargo JA, Lillemoe KD et al (2013) N0/N1, PNL, or LNR? The effect of lymph node number on accurate survival prediction in pancreatic ductal adenocarcinoma. J Gastrointest Surg 17:257–266
Huebner M, Kendrick M, Reid-Lombardo KM, Que F, Therneau T, Qin R et al (2012) Number of lymph nodes evaluated: prognostic value in pancreatic adenocarcinoma. J Gastrointest Surg 16:920–926
Authors’ contributions
• Study conception and design: Yamada S., Hirakawa A.
• Acquisition of data: Fujii T., Kanda M., Sugimoto H.
• Analysis and interpretation of data: Yamada S., Hirakawa A.
• Drafting of manuscript: Yamada S., Kodera Y.
• Critical revision of manuscript: Fujii T.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yamada, S., Fujii, T., Hirakawa, A. et al. Lymph node ratio as parameter of regional lymph node involvement in pancreatic cancer. Langenbecks Arch Surg 401, 1143–1152 (2016). https://doi.org/10.1007/s00423-016-1412-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1412-5