Abstract
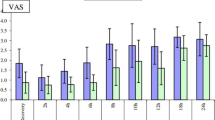
This prospective, randomized, double-blind study was carried out with 320 patients, subdivided into 4 groups of 80 patients each, who underwent arthroscopic knee surgery during the time period from March 1995 to February 1997. Each of the 4 groups received a different solution: 15 ml of bupivacaine 0.5%, 5 mg of morphine in 15 ml of isotonic saline solution, 15 ml of bupivacaine 0.5% with epinephrine 0.0005%, or 15 ml of isotonic saline solution (control group). Within each study group, the following operations were performed: 15 cruciate ligament plasties with autologous patellar tendon grafts, 30 meniscus resections, 15 notch-plasties as preparation for anterior cruciate ligament surgery, and 20 other types of operation (plica resection, diagnostic biopsy, etc.). Pain intensity was assessed with the visual analogue scale obtained from questioning patients at 2, 4, 8, 12, and 24 h postoperatively. In terms of reducing postoperative pain and decreasing the consumption of analgesics after arthroscopic knee surgery, bupivacaine 0.5% with epinephrine 0.0005% was found to be the most effective.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Received: 17 July 2000
Rights and permissions
About this article
Cite this article
Follak, N., Ganzer, D. Postoperative analgesic value of the intra-articular instillation of bupivacaine and morphine after arthroscopic knee surgery. Arch Orth Traum Surg 121, 278–281 (2001). https://doi.org/10.1007/s004020000234
Issue Date:
DOI: https://doi.org/10.1007/s004020000234