Abstract
Background
TME has revolutionized the surgical management of rectal cancer, and since the introduction of robotic TME (RTME), many reports have shown the feasibility and the safety of this approach. However, concerns persist regarding the advantages of robotic in surgery for the completeness of TME. The aim of this review is to compare robotic versus laparoscopic total mesorectal excision (TME) in rectal cancer, focusing on the completeness of TME.
Methods
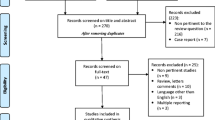
A systematic search was performed in the electronic databases for all available studies comparing RTME versus conventional laparoscopic LTME with declared grade of mesorectum excision. Data regarding sample size, clinical and demographic characteristics, number of complete, nearly complete, and incomplete TME were extracted. Primary outcome was the number of complete TME in robotic and laparoscopic procedures. Secondary outcomes were the numbers of nearly complete and incomplete TME in robotic and laparoscopic rectal resections.
Results
Twelve articles were included in the final analysis. Complete TME was reported by all authors, involving 1510 procedures, showing a significant difference in favor of robotic surgery (OR = 1.83, 95% CI 1.08–3.10, p = 0.03). Nearly complete and incomplete TME showed no significant difference between the procedures. Meta-regression analysis showed that none of patients’ and tumors’ characteristics significantly impacted on complete TME.
Conclusions
Our results underline that the robotic approach to rectal resection is the better way to obtain a complete TME. However, it is mandatory that randomized clinical trials should be performed to assess definitively if robotic minimally invasive surgery is better than a laparoscopic resection.




Similar content being viewed by others
References
Senagore AJ (2015) Adoption of laparoscopic colorectal surgery: it was quite a journey. Clin Colon Rectal Surg 28:131–134
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97:1638–1645
Lee L, Wong-Chong N, Kelly JJ, Nassif GJ, Albert MR, Monson JRT (2018) Minimally invasive surgery for stage III colon adenocarcinoma is associated with less delay to initiation of adjuvant systemic therapy and improved survival. Surg Endosc 2:460–470. https://doi.org/10.1007/s00464-018-6319-5
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgeryethe clue to pelvic recurrence? Br J Surg 69:613–616
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Davies L, Wilson K, Hague W, Simes J, ALaCaRT Investigators (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314(13):1356–1363
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A, Fichera A, Mutch M, Wexner S, Whiteford M, Marks J, Birnbaum E, Margolin D, Larson D, Marcello P, Posner M, Read T, Monson J, Wren SM, Pisters PWT, Nelson H (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Sterne JA, Egger M, Smith GD (2001) Systematic reviews in health care: investigating and dealing with publication and other biases in meta-analysis. BMJ 323:101–105
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455–463
Higgins JP, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of non-randomized studies in meta-analysis. Eur J Epidemiol 25:603–605
Allemann P, Duvoisin C, Di Mare L et al (2016) Robotic-assisted surgery improves the quality of total mesorectal excision for rectal cancer compared to laparoscopy: results of a case-controlled analysis. World J Surg 40(4):1010–1016
Aselmann H, Kersebaum JN, Bernsmeier A et al (2018, 2018) Robotic-assisted total mesorectal excision (TME) for rectal cancer results in a significantly higher quality of TME specimen compared to the laparoscopic approach-report of a single-center experience. Int J Colorectal Dis
Barnajian M, Pettet D 3rd, Kazi E et al (2014) Quality of total mesorectal excision and depth of circumferential resection margin in rectal cancer: a matched comparison of the first 20 robotic cases. Color Dis 16(8):603–609
Colombo PE, Bertrand MM, Alline M, Boulay E, Mourregot A, Carrère S, Quénet F, Jarlier M, Rouanet P (2016) Robotic versus laparoscopic total mesorectal excision (TME) for sphincter-saving surgery: is there any difference in the transanal TME rectal approach? : a single-center series of 120 consecutive patients. Ann Surg Oncol 23(5):1594–1600
Gorgun E, Ozben V, Costedio M, Stocchi L, Kalady M, Remzi F (2016) Robotic versus conventional laparoscopic rectal cancer surgery in obese patients. Color Dis 18(11):1063–1071
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, Quirke P, West N, Rautio T, Thomassen N, Tilney H, Gudgeon M, Bianchi PP, Edlin R, Hulme C, Brown J (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318(16):1569–1580
Kim YS, Kim MJ, Park SC, Sohn DK, Kim DY, Chang HJ, Nam BH, Oh JH (2016) Robotic versus laparoscopic surgery for rectal cancer after preoperative chemoradiotherapy: case-matched study of short-term outcomes. Cancer Res Treat 48(1):225–231
Lim DR, Bae SU, Hur H, Min BS, Baik SH, Lee KY, Kim NK (2017) Long-term oncological outcomes of robotic versus laparoscopic total mesorectal excision of mid-low rectal cancer following neoadjuvant chemoradiation therapy. Surg Endosc 31(4):1728–1737
Ramji KM, Cleghorn MC, Josse JM, MacNeill A, O’Brien C, Urbach D, Quereshy FA (2016) Comparison of clinical and economic outcomes between robotic, laparoscopic, and open rectal cancer surgery: early experience at a tertiary care center. Surg Endosc 30(4):1337–1343
Serin KR, Gultekin FA, Batman B, Ay S, Kapran Y, Saglam S, Asoglu O (2015) Robotic versus laparoscopic surgery for mid or low rectal cancer in male patients after neoadjuvant chemoradiation therapy: comparison of short-term outcomes. J Robot Surg 9(3):187–194
Silva-Velazco J, Dietz DW, Stocchi L, Costedio M, Gorgun E, Kalady MF, Kessler H, Lavery IC, Remzi FH (2017) Considering value in rectal cancer surgery: an analysis of costs and outcomes based on the open, laparoscopic, and robotic approach for proctectomy. Ann Surg 265(5):960–968
Valverde A, Goasguen N, Oberlin O, Svrcek M, Fléjou JF, Sezeur A, Mosnier H, Houdart R, Lupinacci RM (2017) Robotic versus laparoscopic rectal resection for sphincter-saving surgery: pathological and short-term outcomes in a single-center analysis of 130 consecutive patients. Surg Endosc 31(10):4085–4091
van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, Bonjer HJ, COlorectal cancer Laparoscopic or Open Resection II (COLOR II) Study Group (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218
Martínez-Pérez A, Carra MC, Brunetti F, de’Angelis N (2017) Short-term clinical outcomes of laparoscopic vs open rectal excision for rectal cancer: a systematic review and meta-analysis. World J Gastroenterol 23(44):7906–7916
Creavin B, Kelly ME, Ryan E, Winter DC (2017) Meta-analysis of the impact of surgical approach on the grade of mesorectal excision in rectal cancer. Br J Surg 104(12):1609–1619
Li X, Wang T, Yao L, Hu L, Jin P, Guo T, Yang K (2017) The safety and effectiveness of robot-assisted versus laparoscopic TME in patients with rectal cancer: a meta-analysis and systematic review. Medicine (Baltimore) 96(29):e7585
Prete FP, Pezzolla A, Prete F, Testini M, Marzaioli R, Patriti A, Jimenez-Rodriguez RM, Gurrado A, Strippoli GFM (2018) Robotic versus laparoscopic minimally invasive surgery for rectal cancer: a systematic review and meta-analysis of randomized controlled trials. Ann Surg 267(6):1034–1046
Wang Y, Zhao GH, Yang H, Lin J (2016) A pooled analysis of robotic versus laparoscopic surgery for total mesorectal excision for rectal cancer. Surg Laparosc Endosc Percutan Tech 26(3):259–264
Xiong B, Ma L, Huang W, Zhao Q, Cheng Y, Liu J (2015) Robotic versus laparoscopic total mesorectal excision for rectal cancer: a meta-analysis of eight studies. J Gastrointest Surg 19(3):516–526
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Fig. 5a
Quality assessment of the included studies: a Cochrane Collaboration tool for assessing risk of bias (JPG 241 kb)
Fig. 5b
Newcastle-Ottawa Scale (NOS) quality assessment of nRCTs (JPG 244 kb)
Fig. 6
Publication bias of primary outcomes (PNG 380 kb)
Fig. 7
Publication bias of secondary outcomes (PNG 700 kb)
Fig. 8
Publication bias of combined analysis (PNG 696 kb)
Rights and permissions
About this article
Cite this article
Milone, M., Manigrasso, M., Velotti, N. et al. Completeness of total mesorectum excision of laparoscopic versus robotic surgery: a review with a meta-analysis. Int J Colorectal Dis 34, 983–991 (2019). https://doi.org/10.1007/s00384-019-03307-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03307-0