Abstract
Purpose
Sarcopenia is reported to be associated with complications after surgery. However, there is no established optimal parameter to determine sarcopenia affecting surgical outcome. This study investigated whether morphologic change of the psoas muscle (MPM) reflects sarcopenia and could be a predictor of complications after colorectal cancer surgery.
Methods
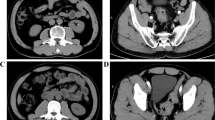
Colorectal cancer patients who underwent primary tumor resection with anastomosis between 2015 and 2016 were analyzed. MPM score was evaluated as the ratio of the short-to-long axis of the psoas muscle in CT images at the L3 vertebrae and classified into five MPM grades. Then, the impact of MPM grade on development of postoperative complications was investigated.
Results
A total of 133 patients were studied. MPM score was significantly correlated to the sectional areas of the psoas muscle at the L3 vertebrae which was evaluated by manual tracing. 21.1% of the subjects were classified into severe MPM (defined as MPM grade 3–4). Overall and infectious complications were noted in 37 (27.8%) and 16 (12.0%) patients. Severe MPM (odds ratio [OR] 2.71, 95% confidence interval [CI] 1.09–6.73), longer operative time (OR 1.01, 95%CI 1.001–1.01), and open surgery (OR 2.73, 95%CI 1.17–6.35) were identified as independent risk factors of overall complications. Severe MPM (OR 4.26,95%CI 1.38–13.10) and open surgery (OR 3.42, 95%CI 1.11–10.48) were identified as independent factors associated with infectious complications.
Conclusions
MPM grade may be used as a simple and convenient marker of sarcopenia and to identify patients at increased risk of complications after colorectal cancer surgery.





Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):359–386. doi:10.1002/ijc.29210
Brown SR, Mathew R, Keding A, Marshall HC, Brown JM, Jayne DG (2014) The impact of postoperative complications on long-term quality of life after curative colorectal cancer surgery. Ann Surg 259(5):916–923. doi:10.1097/SLA.0000000000000407
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinkova E, Vandewoude M, Zamboni M, P. European Working Group on Sarcopenia in Older (2010) Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39(4):412–423. doi:10.1093/ageing/afq034
Reisinger KW, van Vugt JL, Tegels JJ, Snijders C, Hulsewe KW, Hoofwijk AG, Stoot JH, Von Meyenfeldt MF, Beets GL, Derikx JP, Poeze M (2015) Functional compromise reflected by sarcopenia, frailty, and nutritional depletion predicts adverse postoperative outcome after colorectal cancer surgery. Ann Surg 261(2):345–352. doi:10.1097/SLA.0000000000000628
Huang DD, Wang SL, Zhuang CL, Zheng BS, Lu JX, Chen FF, Zhou CJ, Shen X, Yu Z (2015) Sarcopenia, as defined by low muscle mass, strength and physical performance, predicts complications after surgery for colorectal cancer. Color Dis 17(11):256–264. doi:10.1111/codi.13067
Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE (2012) Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer 107(6):931–936. doi:10.1038/bjc.2012.350
Peng PD, van Vledder MG, Tsai S, de Jong MC, Makary M, Ng J, Edil BH, Wolfgang CL, Schulick RD, Choti MA, Kamel I, Pawlik TM (2011) Sarcopenia negatively impacts short-term outcomes in patients undergoing hepatic resection for colorectal liver metastasis. HPB (Oxford) 13(7):439–446. doi:10.1111/j.1477-2574.2011.00301.x
Miyamoto Y, Baba Y, Sakamoto Y, Ohuchi M, Tokunaga R, Kurashige J, Hiyoshi Y, Iwagami S, Yoshida N, Yoshida M, Watanabe M, Baba H (2015) Sarcopenia is a negative prognostic factor after curative resection of colorectal cancer. Ann Surg Oncol 22(8):2663–2668. doi:10.1245/s10434-014-4281-6
Boer BC, de Graaff F, Brusse-Keizer M, Bouman DE, Slump CH, Slee-Valentijn M, Klaase JM (2016) Skeletal muscle mass and quality as risk factors for postoperative outcome after open colon resection for cancer. Int J Color Dis 31(6):1117–1124. doi:10.1007/s00384-016-2538-1
Malietzis G, Aziz O, Bagnall NM, Johns N, Fearon KC, Jenkins JT (2015) The role of body composition evaluation by computerized tomography in determining colorectal cancer treatment outcomes: a systematic review. Eur J Surg Oncol 41(2):186–196. doi:10.1016/j.ejso.2014.10.056
Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, Baracos VE (2008) Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol 9(7):629–635. doi:10.1016/S1470-2045(08)70153-0
Peng P, Hyder O, Firoozmand A, Kneuertz P, Schulick RD, Huang D, Makary M, Hirose K, Edil B, Choti MA, Herman J, Cameron JL, Wolfgang CL, Pawlik TM (2012) Impact of sarcopenia on outcomes following resection of pancreatic adenocarcinoma. J Gastrointest Surg 16(8):1478–1486. doi:10.1007/s11605-012-1923-5
Yoshizumi T, Shirabe K, Nakagawara H, Ikegami T, Harimoto N, Toshima T, Yamashita Y, Ikeda T, Soejima Y, Maehara Y (2014) Skeletal muscle area correlates with body surface area in healthy adults. Hepatol Res 44(3):313–318. doi:10.1111/hepr.12119
Inokuchi S, Sugawara H, Shibata M, Suzuki M, Ito J, Matumura A (2002) Age related changes of the trunk muscle observed by CT image. Anthoropol Sci 109(2):71–83
Onodera T, Goseki N, Kosaki G (1984) Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 85(9):1001–1005
Sagawa M, Yoshimatsu K, Yokomizo H, Yano Y, Nakayama M, Usui T, Yamaguchi K, Shiozawa S, Shimakawa T, Katsube T, Naritaka Y (2014) Onodera’s prognostic nutritional index (PNI) and the modified Glasgow Prognostic Score (mGPS) in colorectal cancer surgery. Gan To Kagaku Ryoho 41(10):1273–1275
McMillan DC, Crozier JE, Canna K, Angerson WJ, McArdle CS (2007) Evaluation of an inflammation-based prognostic score (GPS) in patients undergoing resection for colon and rectal cancer. Int J Color Dis 22(8):881–886. doi:10.1007/s00384-006-0259-6
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Moyes LH, Leitch EF, McKee RF, Anderson JH, Horgan PG, McMillan DC (2009) Preoperative systemic inflammation predicts postoperative infectious complications in patients undergoing curative resection for colorectal cancer. Br J Cancer 100(8):1236–1239. doi:10.1038/sj.bjc.6604997
Tevis SE, Kohlnhofer BM, Stringfield S, Foley EF, Harms BA, Heise CP, Kennedy GD (2013) Postoperative complications in patients with rectal cancer are associated with delays in chemotherapy that lead to worse disease-free and overall survival. Dis Colon rectum 56(12):1339–1348. doi:10.1097/DCR.0b013e3182a857eb
Sawas T, Al Halabi S, Hernaez R, Carey WD, Cho WK (2015) Patients receiving prebiotics and probiotics before liver transplantation develop fewer infections than controls: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 13(9):1567–1574. doi:10.1016/j.cgh.2015.05.027
Mayo NE, Feldman L, Scott S, Zavorsky G, Kim DJ, Charlebois P, Stein B, Carli F (2011) Impact of preoperative change in physical function on postoperative recovery: argument supporting prehabilitation for colorectal surgery. Surgery 150(3):505–514. doi:10.1016/j.surg.2011.07.045
Pouwels S, Stokmans RA, Willigendael EM, Nienhuijs SW, Rosman C, van Ramshorst B, Teijink JA (2014) Preoperative exercise therapy for elective major abdominal surgery: a systematic review. Int J Surg 12(2):134–140. doi:10.1016/j.ijsu.2013.11.018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Hanaoka, M., Yasuno, M., Ishiguro, M. et al. Morphologic change of the psoas muscle as a surrogate marker of sarcopenia and predictor of complications after colorectal cancer surgery. Int J Colorectal Dis 32, 847–856 (2017). https://doi.org/10.1007/s00384-017-2773-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2773-0