Abstract
Objectives
To establish the effect of different degrees and kinds of physical activity on bone marrow fat (BMAT) content at different anatomical locations in a population-based cohort study undergoing whole-body MR imaging.
Methods
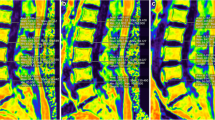
Subjects of the KORA FF4 study without known cardiovascular disease underwent BMAT fat fraction (FF) quantification in L1 and L2 vertebrae and femoral heads/necks (hip) via a 2-point T1-weighted VIBE Dixon sequence. BMAT-FF was calculated as mean value (fat image) divided by mean value (fat + water image). Physical activity was determined by self-assessment questionnaire regarding time spent exercising, non-exercise walking, non-exercise cycling, and job-related physical activity.
Results
A total of 385 subjects (96% of 400 available; 56 ± 9.1 years; 58% male) were included in the analysis. Exercise was distributed quite evenly (29% > 2 h/week; 31% ~ 1 h/week (regularly); 15% ~ 1 h/week (irregularly); 26% no physical activity). BMAT-FF was 52.6 ± 10.2% in L1, 56.2 ± 10.3% in L2, 87.4 ± 5.9% in the right hip, and 87.2 ± 5.9% in the left hip (all p < 0.001). Correlation of BMAT-FF between spine and hip was only moderate (r 0.42 to 0.46). Spinal BMAT-FF, but not hip BMAT-FF, was inversely associated with exercise > 2 h/week (p ≤ 0.02 vs. p ≥ 0.35, respectively). These associations remained significant after adjusting for age, gender, waist circumference, and glucose tolerance. No coherent association was found between BMAT-FF and physical activity in the less active groups.
Conclusions
In our study, exercise was inversely correlated with vertebral BMAT-FF, but not hip BMAT-FF, when exercising for more than 2 h per week. Physical activity seems to affect the spine at least preferentially compared to the hip.
Key Points
• In our population-based cohort, at least 2 h of physical activity per week were required to show lower levels of bone marrow adipose tissue fat fraction in MRI.
• Physical activity seems to affect bone marrow adipose tissue at least preferentially at the spine in contrast to the proximal femur.



Similar content being viewed by others
Abbreviations
- BMAT:
-
Bone marrow adipose tissue
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- FF:
-
Fat fraction
- L1:
-
Lumbar vertebra 1
- L2:
-
Lumbar vertebra 2
- LH:
-
Left hip = left proximal femur
- PDFF:
-
Proton density fat fraction
- RH:
-
Right hip = right proximal femur
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- WC:
-
Waist circumference
References
Al-Nbaheen M, Vishnubalaji R, Ali D et al (2013) Human stromal (mesenchymal) stem cells from bone marrow, adipose tissue and skin exhibit differences in molecular phenotype and differentiation potential. Stem Cell Rev 9:32–43
Gimble JM, Zvonic S, Floyd ZE, Kassem M, Nuttall ME (2006) Playing with bone and fat. J Cell Biochem 98:251–266
Pagnotti GM, Styner M (2016) Exercise regulation of marrow adipose tissue. Front Endocrinol (Lausanne) 7:94
Suchacki KJ, Cawthorn WP (2018) Molecular interaction of bone marrow adipose tissue with energy metabolism. Curr Mol Biol Rep 4:41–49
Ambrosi TH, Scialdone A, Graja A et al (2017) Adipocyte accumulation in the bone marrow during obesity and aging impairs stem cell-based hematopoietic and bone regeneration. Cell Stem Cell 20:771–784 e776
Zhou BO, Yu H, Yue R et al (2017) Bone marrow adipocytes promote the regeneration of stem cells and haematopoiesis by secreting SCF. Nat Cell Biol 19:891–903
Reagan M, Falank C, Fairfield H, McDonald M, Croucher P, Rosen CJ (2016) Multiple myeloma progression: dependence on bone marrow adipose tissue. Blood 128:3262–3262
Kugel H, Jung C, Schulte O, Heindel W (2001) Age- and sex-specific differences in the 1H-spectrum of vertebral bone marrow. J Magn Reson Imaging 13:263–268
Andrews CL (2000) From the RSNA Refresher Courses. Radiological Society of North America. Evaluation of the marrow space in the adult hip. Radiographics 20:S27-S42
Li Z, Hardij J, Bagchi DP, Scheller EL, MacDougald OA (2018) Development, regulation, metabolism and function of bone marrow adipose tissues. Bone 110:134–140
Ricci C, Cova M, Kang YS et al (1990) Normal age-related patterns of cellular and fatty bone marrow distribution in the axial skeleton: MR imaging study. Radiology 177:83–88
Ishijima H, Ishizaka H, Horikoshi H, Sakurai M (1996) Water fraction of lumbar vertebral bone marrow estimated from chemical shift misregistration on MR imaging: normal variations with age and sex. AJR Am J Roentgenol 167:355–358
Bredella MA, Fazeli PK, Miller KK et al (2009) Increased bone marrow fat in anorexia nervosa. J Clin Endocrinol Metab 94:2129–2136
Adler BJ, Kaushansky K, Rubin CT (2014) Obesity-driven disruption of haematopoiesis and the bone marrow niche. Nat Rev Endocrinol 10:737–748
Bredella MA, Torriani M, Ghomi RH et al (2011) Vertebral bone marrow fat is positively associated with visceral fat and inversely associated with IGF-1 in obese women. Obesity (Silver Spring) 19:49–53
Veldhuis-Vlug AG, Rosen CJ (2018) Clinical implications of bone marrow adiposity. J Intern Med 283:121–139
Sasai H, Katayama Y, Nakata Y et al (2010) The effects of vigorous physical activity on intra-abdominal fat levels: a preliminary study of middle-aged Japanese men. Diabetes Res Clin Pract 88:34–41
Verheggen RJ, Maessen MF, Green DJ, Hermus AR, Hopman MT, Thijssen DH (2016) A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: distinct effects on body weight and visceral adipose tissue. Obes Rev 17:664–690
Kuhle CL, Steffen MW, Anderson PJ, Murad MH (2014) Effect of exercise on anthropometric measures and serum lipids in older individuals: a systematic review and meta-analysis. BMJ Open 4:e005283
Miyamoto-Mikami E, Sato K, Kurihara T et al (2015) Endurance training-induced increase in circulating irisin levels is associated with reduction of abdominal visceral fat in middle-aged and older adults. PLoS One 10:e0120354
Tong TK, Zhang H, Shi H et al (2018) Comparing time efficiency of sprint vs. high-intensity interval training in reducing abdominal visceral fat in obese young women: a randomized, controlled trial. Front Physiol 9:1048
Gappmaier E, Lake W, Nelson AG, Fisher AG (2006) Aerobic exercise in water versus walking on land: effects on indices of fat reduction and weight loss of obese women. J Sports Med Phys Fitness 46:564–569
Maillard F, Rousset S, Pereira B et al (2016) High-intensity interval training reduces abdominal fat mass in postmenopausal women with type 2 diabetes. Diabetes Metab 42:433–441
Ross R, Janssen I, Dawson J et al (2004) Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes Res 12:789–798
Leon AS, Conrad J, Hunninghake DB, Serfass R (1979) Effects of a vigorous walking program on body composition, and carbohydrate and lipid metabolism of obese young men. Am J Clin Nutr 32:1776–1787
Pollock ML, Dimmick J, Miller HS Jr, Kendrick Z, Linnerud AC (1975) Effects of mode of training on cardiovascular function and body composition of adult men. Med Sci Sports 7:139–145
Trapp EG, Chisholm DJ, Freund J, Boutcher SH (2008) The effects of high-intensity intermittent exercise training on fat loss and fasting insulin levels of young women. Int J Obes (Lond) 32:684–691
Wronski TJ, Morey ER (1982) Skeletal abnormalities in rats induced by simulated weightlessness. Metab Bone Dis Relat Res 4:69–75
David V, Martin A, Lafage-Proust MH et al (2007) Mechanical loading down-regulates peroxisome proliferator-activated receptor gamma in bone marrow stromal cells and favors osteoblastogenesis at the expense of adipogenesis. Endocrinology 148:2553–2562
Styner M, Pagnotti GM, Galior K et al (2015) Exercise regulation of marrow fat in the setting of PPARgamma agonist treatment in female C57BL/6 mice. Endocrinology 156:2753–2761
Styner M, Thompson WR, Galior K et al (2014) Bone marrow fat accumulation accelerated by high fat diet is suppressed by exercise. Bone 64:39–46
Ahdjoudj S, Lasmoles F, Holy X, Zerath E, Marie PJ (2002) Transforming growth factor beta2 inhibits adipocyte differentiation induced by skeletal unloading in rat bone marrow stroma. J Bone Miner Res 17:668–677
Styner M, Pagnotti GM, McGrath C et al (2017) Exercise decreases marrow adipose tissue through ss-oxidation in obese running mice. J Bone Miner Res 32:1692–1702
Menuki K, Mori T, Sakai A et al (2008) Climbing exercise enhances osteoblast differentiation and inhibits adipogenic differentiation with high expression of PTH/PTHrP receptor in bone marrow cells. Bone 43:613–620
Trudel G, Coletta E, Cameron I et al (2012) Resistive exercises, with or without whole body vibration, prevent vertebral marrow fat accumulation during 60 days of head-down tilt bed rest in men. J Appl Physiol (1985) 112:1824–1831
Trudel G, Payne M, Madler B et al (2009) Bone marrow fat accumulation after 60 days of bed rest persisted 1 year after activities were resumed along with hemopoietic stimulation: the women international space simulation for exploration study. J Appl Physiol (1985) 107:540–548
Belavy DL, Quittner MJ, Ridgers ND, Shiekh A, Rantalainen T, Trudel G (2018) Specific modulation of vertebral marrow adipose tissue by physical activity. J Bone Miner Res 33:651–657
Casazza K, Hanks LJ, Hidalgo B, Hu HH, Affuso O (2012) Short-term physical activity intervention decreases femoral bone marrow adipose tissue in young children: a pilot study. Bone 50:23–27
Rantalainen T, Nikander R, Heinonen A, Cervinka T, Sievanen H, Daly RM (2013) Differential effects of exercise on tibial shaft marrow density in young female athletes. J Clin Endocrinol Metab 98:2037–2044
Huovinen V, Viljakainen H, Hakkarainen A et al (2015) Bone marrow fat unsaturation in young adults is not affected by present or childhood obesity, but increases with age: a pilot study. Metabolism 64:1574–1581
Holle R, Happich M, Lowel H, Wichmann HE, MONICA/KORA Study Group (2005) KORA--a research platform for population based health research. Gesundheitswesen 67(Suppl 1):S19–S25
Bamberg F, Hetterich H, Rospleszcz S et al (2017) Subclinical disease burden as assessed by whole-body MRI in subjects with prediabetes, subjects with diabetes, and normal control subjects from the general population: the KORA-MRI study. Diabetes 66:158–169
Karl FM, Tremmel M, Luzak A et al (2018) Direct healthcare costs associated with device assessed and self-reported physical activity: results from a cross-sectional population-based study. BMC Public Health 18:966
Li GW, Xu Z, Chen QW et al (2014) Quantitative evaluation of vertebral marrow adipose tissue in postmenopausal female using MRI chemical shift-based water-fat separation. Clin Radiol 69:254–262
Singhal V, Maffazioli GDN, Cano Sokoloff N et al (2015) Regional fat depots and their relationship to bone density and microarchitecture in young oligo-amenorrheic athletes. Bone 77:83–90
Statistisches Bundesamt W (2014) Microzensus - Fragen zur Gesundheit - Körpermaße der Bevölkerung. Statistisches Bundesamt, Wiesbaden
Fryar CD, Kruszon-Moran D, Gu Q, Ogden CL (2018) Mean body weight, height, waist circumference, and body mass index among adults: United States, 1999–2000 Through 2015–2016. Natl Health Stat Report:1–16
(2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:i-xii, 1–253
UK NHS (2019) Why is my waist size important? NHS UK, UK. Available via https://www.nhs.uk/common-health-questions/lifestyle/why-is-my-waist-size-important/. Accessed February 11 2019
Maillard F, Pereira B, Boisseau N (2018) Effect of high-intensity interval training on total, abdominal and visceral fat mass: a meta-analysis. Sports Med 48:269–288
Moore S, Dawson LK (1990) Red and yellow marrow in the femur: age-related changes in appearance at MR imaging. Radiology 175:219–223
Di Iorgi N, Rosol M, Mittelman SD, Gilsanz V (2008) Reciprocal relation between marrow adiposity and the amount of bone in the axial and appendicular skeleton of young adults. J Clin Endocrinol Metab 93:2281–2286
Shen W, Chen J, Punyanitya M, Shapses S, Heshka S, Heymsfield SB (2007) MRI-measured bone marrow adipose tissue is inversely related to DXA-measured bone mineral in Caucasian women. Osteoporos Int 18:641–647
Post S, Abdallah BM, Bentzon JF, Kassem M (2008) Demonstration of the presence of independent pre-osteoblastic and pre-adipocytic cell populations in bone marrow-derived mesenchymal stem cells. Bone 43:32–39
Goffrier B, Schulz M, Bätzing-Feigenbaum J (2017) Administrative Prävalenzen und Inzidenzen des Diabetes mellitus von 2009 bis 2015. Versorgungsatlas-Bericht, Zentralinstitut für die kassenärztliche Versorgung in Deutschland 17/03
Centers for Disease Control and Prevention (2017) National Diabetes Statistics Report, 2017
Rathmann W, Haastert B, Icks A et al (2003) High prevalence of undiagnosed diabetes mellitus in southern Germany: target populations for efficient screening. The KORA survey 2000. Diabetologia 46:182–189
Karampinos DC, Melkus G, Baum T, Bauer JS, Rummeny EJ, Krug R (2014) Bone marrow fat quantification in the presence of trabecular bone: initial comparison between water-fat imaging and single-voxel MRS. Magn Reson Med 71:1158–1165
Acknowledgments
The KORA study was initiated and financed by the Helmholtz Zentrum München, German Research Center for Environmental Health, which is funded by the German Federal Ministry of Education and Research (BMBF) and by the State of Bavaria. The MRI study and in part this analysis were funded by the German Research Foundation (DFG, Bonn, Germany), the German Centre for Diabetes Research (DZD, Neuherberg Germany), and the German Centre for Cardiovascular Disease Research (DZHK, Berlin, Germany).
Funding
The KORA study was initiated and financed by the Helmholtz Zentrum München, German Research Center for Environmental Health, which is funded by the German Federal Ministry of Education and Research (BMBF) and by the State of Bavaria. The MRI study and in part this analysis were funded by the German Research Foundation (DFG, Bonn, Germany), the German Centre for Diabetes Research (DZD, Neuherberg Germany), and the German Centre for Cardiovascular Disease Research (DZHK, Berlin, Germany).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Christopher L. Schlett, MD MPH, Department of Diagnostic and Interventional Radiology, Medical Center—University of Freiburg.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in several studies, however not in relation to bone marrow adipose tissue, so there is no overlap.
Methodology
• retrospective
• cross-sectional study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 38 kb)
Fig. 4
Scatter plots of the correlation between different BMAT-FF measurements. Top row: spine vs. spine and hip vs. hip. Bottom rows: spine vs. hip. All p < 0.001 (PNG 102 kb)
ESM 2
(EPS 4.01 mb)
Fig. 5
Change of BMAT-FF associated with active exercise. The reported changes were absolute numbers and adjusted for age and gender. Subjects with high active exercise (“≥ 2h per week, regularly”) were compared to subjects with low exercise (“no or nearly no exercise”) (PNG 111 kb)
ESM 2
(EPS 3.23 mb)
Rights and permissions
About this article
Cite this article
Bertheau, R.C., Lorbeer, R., Nattenmüller, J. et al. Bone marrow fat fraction assessment in regard to physical activity: KORA FF4–3-T MR imaging in a population-based cohort. Eur Radiol 30, 3417–3428 (2020). https://doi.org/10.1007/s00330-019-06612-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06612-y