Abstract
Objectives
To assess inter-sonographer reproducibility of ultrasound attenuation coefficient (AC), backscatter coefficient (BSC) and shear wave speed (SWS) in adults with known/suspected non-alcoholic fatty liver disease (NAFLD).
Methods
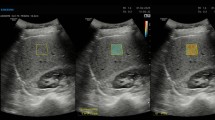
The institutional review board approved this HIPAA-compliant prospective study; informed consent was obtained. Participants with known/suspected NAFLD were recruited and underwent same-day liver examinations with a clinical scanner. Each participant was scanned by two of the six trained sonographers. Each sonographer performed multiple data acquisitions in the right liver lobe using a lateral intercostal approach. A data acquisition was a single operator button press that recorded a B-mode image, radio-frequency data, and the SWS value. AC and BSC were calculated from the radio-frequency data using the reference phantom method. SWS was calculated automatically using product software. Intraclass correlation coefficient (ICC) and within-subject coefficient of variation (wCV) were calculated for applicable metrics.
Results
Sixty-one participants were recruited. Inter-sonographer ICC was 0.86 (95% confidence interval: 0.77–0.92) for AC and 0.87 (0.78–0.92) for log-transformed BSC (logBSC = 10log10BSC) using one acquisition per sonographer. ICC was 0.88 (0.80–0.93) for both AC and logBSC averaging 5 acquisitions. ICC for SWS was 0.57 (0.29–0.74) using one acquisition per sonographer, and 0.84 (0.66–0.93) using 10 acquisitions. The wCV was ~7% for AC, and 19–43% for SWS, depending on number of acquisitions.
Conclusions
Hepatic AC, BSC and SWS measures on a clinical scanner have good inter-sonographer reproducibility in adults with known or suspected NAFLD. Multiple acquisitions are required for SWS but not AC or BSC to achieve good inter-sonographer reproducibility.
Key Points
• AC, BSC and SWS measurements are reproducible in adults with NAFLD.
• Inter-sonographer reproducibility of SWS measurement improves with more acquisitions being averaged.
• Multiple acquisitions are required for SWS but not AC or BSC.




Similar content being viewed by others
Abbreviations
- AC:
-
Attenuation coefficient
- ANOVA:
-
Analysis of variance
- BMI:
-
Body mass index
- BSC:
-
Backscatter coefficient
- CAP:
-
Controlled attenuation parameter
- FOI:
-
Field of interest
- ICC:
-
Intraclass correlation coefficient
- logBSC:
-
log-transformed backscatter coefficient
- MRI:
-
Magnetic resonance imaging
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH CRN:
-
Nonalcoholic Steatohepatitis Clinical Research Network
- PDFF:
-
Proton density fat fraction
- QIB:
-
Quantitative imagine biomarker
- QIBA:
-
Quantitative Imaging Biomarker Alliance
- QUS:
-
Quantitative ultrasound
- RF:
-
Radio-frequency
- ROI:
-
Region of interest
- RSNA:
-
Radiological Society of North America
- SWS:
-
Shear wave speed
- USFDA:
-
United States Food and Drug Administration
- VTQ:
-
Virtual touch quantification
- wCV:
-
within-subject coefficient of variation
References
Shiina T, Nightingale KR, Palmeri ML et al (2015) WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 1: basic principles and terminology. Ultrasound Med Biol 41:1126–1147
Palmeri ML, Wang MH, Rouze NC et al (2011) Noninvasive evaluation of hepatic fibrosis using acoustic radiation force-based shear stiffness in patients with nonalcoholic fatty liver disease. J Hepatol 55:666–672
Ferraioli G, Filice C, Castera L et al (2015) WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 3: liver. Ultrasound Med Biol 41:1161–1179
Ferraioli G, Parekh P, Levitov AB, Filice C (2014) Shear wave elastography for evaluation of liver fibrosis. J Ultrasound Med 33:197–203
Bavu E, Gennisson JL, Couade M et al (2011) Noninvasive in vivo liver fibrosis evaluation using supersonic shear imaging: a clinical study on 113 hepatitis C virus patients. Ultrasound Med Biol 37:1361–1373
Lin SC, Heba E, Wolfson T et al (2015) Noninvasive diagnosis of nonalcoholic fatty liver disease and quantification of liver fat using a new quantitative ultrasound technique. Clin Gastroenterol Hepatol 13:1337–1345.e6
Andre MP, Han A, Heba E, et al (2014) Accurate diagnosis of nonalcoholic fatty liver disease in human participants via quantitative ultrasound. In: 2014 IEEE International Ultrasonics Symposium. pp 2375–2377
Paige JS, Bernstein GS, Heba E et al (2017) A pilot comparative study of quantitative ultrasound, conventional ultrasonography, and magnetic resonance imaging for predicting histology-determined steatosis grade in adult nonalcoholic fatty liver disease. Am J Roentgenol 208:W1–W10
McFarlin BL, Balash J, Kumar V et al (2015) Development of an ultrasonic method to detect cervical remodeling in vivo in full-term pregnant women. Ultrasound Med Biol 41:2533–2539
McFarlin BL, Kumar V, Bigelow TA et al (2015) Beyond cervical length: a pilot study of ultrasonic attenuation for early detection of preterm birth risk. Ultrasound Med Biol 41:3023–3029
Sadeghi-Naini A, Papanicolau N, Falou O et al (2013) Quantitative ultrasound evaluation of tumor cell death response in locally advanced breast cancer patients receiving chemotherapy. Clin Cancer Res 19:2163–2173
Sasso M, Beaugrand M, de Ledinghen V et al (2010) Controlled Attenuation Parameter (CAP): A novel VCTE™ guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: Preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med Biol 36:1825–1835
Caussy C, Alquiraish MH, Nguyen P et al (2017) Optimal threshold of controlled attenuation parameter with MRI-PDFF as the gold standard for the detection of hepatic steatosis. Hepatology. https://doi.org/10.1002/hep.29639
Park CC, Nguyen P, Hernandez C et al (2017) Magnetic resonance elastography vs transient elastography in detection of fibrosis and noninvasive measurement of steatosis in patients with biopsy-proven nonalcoholic fatty liver disease. Gastroenterology 152:598–607
Cui J, Heba E, Hernandez C et al (2016) Magnetic resonance elastography is superior to acoustic radiation force impulse for the diagnosis of fibrosis in patients with biopsy-proven nonalcoholic fatty liver disease: A prospective study. Hepatology 63:453–461
Sullivan DC, Obuchowski NA, Kessler LG et al (2015) Metrology standards for quantitative imaging biomarkers. Radiology 277:813–825
Han A, Andre MP, Erdman JW, Loomba R, Sirlin CB, O’Brien WD (2017) Repeatability and reproducibility of a clinically based QUS phantom study and methodologies. IEEE Trans Ultrason Ferroelectr Freq Control 64:218–231
Han A, Andre MP, Erdman JW, Loomba R, Claude SB, O’Brien WD (2018) Repeatability and reproducibility of ultrasonic attenuation coefficient and backscatter coefficient measured in the right lobe of the liver in adults with known or suspected nonalcoholic fatty liver disease. J Ultrasound Med. https://doi.org/10.1002/jum.14537
Bota S, Sporea I, Sirli R, Popescu A, Danila M, Costachescu D (2012) Intra- and interoperator reproducibility of acoustic radiation force impulse (ARFI) elastography--preliminary results. Ultrasound Med Biol 38:1103–1108
Sporea I, Bota S, Jurchis A et al (2013) Acoustic radiation force impulse and supersonic shear imaging versus transient elastography for liver fibrosis assessment. Ultrasound Med Biol 39:1933–1941
Yao LX, Zagzebski JA, Madsen EL (1990) Backscatter coefficient measurements using a reference phantom to extract depth-dependent instrumentation factors. Ultrason Imaging 12:58–70
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
Raunig DL, McShane LM, Pennello G et al (2015) Quantitative imaging biomarkers: a review of statistical methods for technical performance assessment. Stat Methods Med Res 24:27–67
Trout AT, Serai S, Mahley AD et al (2016) Liver stiffness measurements with MR elastography: agreement and repeatability across imaging systems, field strengths, and pulse sequences. Radiology 281:793–804
Nobili V, Vizzutti F, Arena U et al (2008) Accuracy and reproducibility of transient elastography for the diagnosis of fibrosis in pediatric nonalcoholic steatohepatitis. Hepatology 48:442–448
Kleiner DE, Brunt EM, Van Natta M et al (2005) Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 41:1313–1321
Fraquelli M, Rigamonti C, Casazza G et al (2007) Reproducibility of transient elastography in the evaluation of liver fibrosis in patients with chronic liver disease. Gut 56:968–973
Acknowledgements
We are grateful for the dedicated contributions and expertise of the six sonographers who participated in this study, Lara Callahan, Lisa Deiranieh, Elise Housman, Christopher Lucas, Susan Lynch, and Minaxi Trivedi, without whom this work could not be completed.
Funding
This study has received funding by the National Institutes of Health (R01DK106419) and Siemens Healthineers USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Claude B. Sirlin, MD (University of California at San Diego).
Conflict of interest
The authors of this manuscript declare relationships with the following companies:
One of the authors (YL) is an employee of Siemens Healthineers USA. The work is supported in part by a research grant from Siemens Healthineers USA. The use of the Siemens S3000 scanner was loaned to the University of California San Diego under a research agreement with Siemens Healthineers USA. At all times, the study data was under the control of the other authors, none of whom are employees of Siemens.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional review board approval was obtained.
Methodology
• prospective
• cross-sectional study
• performed at one institution
Electronic supplementary material
ESM 1
(DOCX 1180 kb)
Rights and permissions
About this article
Cite this article
Han, A., Labyed, Y., Sy, E.Z. et al. Inter-sonographer reproducibility of quantitative ultrasound outcomes and shear wave speed measured in the right lobe of the liver in adults with known or suspected non-alcoholic fatty liver disease. Eur Radiol 28, 4992–5000 (2018). https://doi.org/10.1007/s00330-018-5541-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5541-9