Abstract
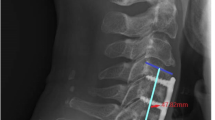
Since the introduction of anterior approaches to the cervical spine for the surgical treatment of degenerative disc disease, controversies have developed regarding the necessity of fusion following anterior cervical discectomy, the use of allografts instead of autologous bone for fusion, and, recently, the employment of anterior cervical plating systems in addition to fusion for uncomplicated disc disease. We reviewed seven clinical papers dealing with these issues; these articles surveyed a total of 1153 patients. Several observations can be made from these reviews. First, there is little or no difference in clinical outcome following single-level anterior discectomy, whether a fusion is performed or not, regardless of whether the operation was for soft discs or osteophytes. Second, most patients who underwent two-level discectomies had outcomes comparable to patients who underwent surgery at one level, regardless of whether they were fused or not. Data from four prospective randomized clinical studies in addition to multiple nonrandomized or retrospective studies support these conclusions. Although the incidence of complications such as persistent postoperative posterior cervical and shoulder pain and kyphotic deformities is higher in unfused patients (and is quite significant in some series), the advantages conferred by interbody fusion such as biomechanical stability, decreased incidence of kyphotic deformity, and decreased pain are offset by graft and donor-site morbidity. Specific indications for fusion include multi-level discectomies, significant straightening of the cervical spine, failed prior fusions, and trauma. It has been demonstrated that comparable fusion rates can be achieved with allografts rather than harvested autologous bone. The advantages of autografts over allografts are relatively slight in most patients who undergo anterior fusion for one- or two-level disc disease, although patients with impaired healing, significant osteopenia, or concomitant microvascular disease, such as chronic smokers, may benefit from autologous bone. The use of allografts avoids donor-site morbidity in patients without these problems. Anterior cervical plates are useful for cases of instability requiring fusion (such as trauma); these implants may decrease reoperation rates and the incidence of delayed instability in select cases. However, the cost-effectiveness of their generalized use for uncomplicated cervical disc disease has not been demonstrated. In conclusion, a general statement regarding the optimal surgical treatment for cervical disc herniations using anterior approaches is difficult to make with this limited review. Surgeons’ experience and familiarity with a particular approach are probably the most important factors in ensuring successful outcomes.
Similar content being viewed by others
Papers reviewed
Pointillart V, Cernier JM, Vital JM, Senegas J (1995) Anterior discectomy without interbody fusion for cervical disc herniation. Eur Spine J 4:45–51
Savolainen S, Rinne J, Hernesniemi J (1998) A prospective randomized study of anterior single-level cervical disc operations with long-term follow-up: surgical fusion is unnecessary. Neurosurgery 43:51–55
Caspar W, Geisler FH, Pitzen T, Johnson TA (1998) Anterior cervical plate stabilization in one- and two-level degenerative disc disease: overtreatment or benefit? J Spinal Disord 11:1–11
Cauthen JC, Kinard RE, Vogler JB, Jackson DE, DePaz OB, Hunter OL, Wasserburger LB, Willimas VM (1998) Outcome analysis of noninstrumented anterior cervical discectomy and interbody fusion in 348 patients. Spine 23:188–192
Maurice-Williams RS, Dorward NL (1996) Extended anterior cervical discectomy without fusion: a simple and sufficient operation for most cases of cervical degenerative disease. Br J Neurosurg 10:261–266
Dowd GC, Wirth FP (1999) Anterior cervical discectomy: is fusion necessary? J Neurosurg 90:8–12
Murphy MA, Trimble MB, Piedmonte MR, Kalfas IA (1994) Changes in the cervical foraminal area after anterior cervical discectomy with and without a graft. Neurosurgery 34:93–96
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Alvarez, J., Hardy, R. Anterior cervical discectomy for one- and two-level cervical disc disease: the controversy surrounding the question of whether to fuse, plate, or both. Crit Rev Neurosurg 9, 234–251 (1999). https://doi.org/10.1007/s003290050138
Published:
Issue Date:
DOI: https://doi.org/10.1007/s003290050138