Abstract
Introduction
In order to avoid pseudarthrosis in adolescent idiopathic (AIS) patients, it is recommended to bring additional bone graft or substitute. Modern rigid instrumentations have been shown to provide less pseudarthroses even without bone substitutes. The aim of our study was to determine the impact of using bones substitutes on fusion rates in adolescent idiopathic scoliosis patients undergoing PSF with sublaminar bands.
Method
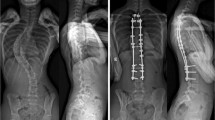
AIS patients scheduled to undergo PSF with sublaminar bands were prospectively enrolled into this study and not given any bone substitutes (no-substitute group). Data were collected and analyzed in patients with at least two years of follow-up. Pseudarthrosis was diagnosed if at least one of the following was present: persistent back pain, hardware failure, loss of correction greater than 10°. The results were compared to a control group who received bone substitutes for the same surgical procedure.
Results
Eighty-eight patients were included. For the whole cohort, the mean age was 14.8 years old and the mean follow-up was 30.9 months. For the ‘no-substitute’ group (n = 44), the mean Cobb angle was 56° pre-operatively, 20.1° post-operatively, and 22° at final follow-up. The fusion rate was not statistically different between the two groups (97.7% vs 95.5%, p = 0.56). At last follow-up, one pseudarthrosis occurred in the ‘no substitute’ group and two in the control group.
Discussion
This is the first study to determine the impact of bone substitutes in AIS fusion using sublaminar bands. In our study, the use of local autologous bone graft alone resulted in a fusion rate of 97.7% despite the use of more flexible instrumentation. The high rate of fusion in AIS patients is more probably due to the healing potential of these young patients rather than to the type of instrumentation.
Conclusion
The use of additional bone graft or bone substitutes may not be mandatory when managing AIS.
Level of evidence: 4.



Similar content being viewed by others
References
Dawson EG, Clader TJ, Bassett LW (1985) A comparison of different methods used to diagnose pseudarthrosis following posterior spinal fusion for scoliosis. J Bone Jt Surg Am 67:1153–1159
Bridwell KH, O’Brien MF, Lenke LG, Baldus C, Blanke K (1994) Posterior spinal fusion supplemented with only allograft bone in paralytic scoliosis. Does it work? Spine (Phila Pa 1976) 19:2658–2666
Betz RR, Lavelle WF, Samdani AF (2010) Bone grafting options in children. Spine 35:1648–1654
Theologis AA, Tabaraee E, Lin T et al (2015) Type of bone graft or substitute does not affect outcome of spine fusion with instrumentation for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 40:1345–1351. doi:10.1097/BRS.0000000000001002
Betz RR, Petrizzo AM, Kerner PJ, Falatyn SP, Clements DH, Huss GK (2006) Allograft versus no graft with a posterior multisegmented hook system for the treatment of idiopathic scoliosis. Spine (Phila Pa 1976) 31:121–127
Lykissas MG, Jain VV, Nathan ST et al (2013) Mid- to long-term outcomes in adolescent idiopathic scoliosis after instrumented posterior spinal fusion: a meta-analysis. Spine (Phila Pa 1976) 38:E113–E119. doi:10.1097/BRS.0b013e31827ae3d0
Mazda K, Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Penneçot GF (2009) Efficacy and safety of posteromedial translation for correction of thoracic curves in adolescent idiopathic scoliosis using a new connection to the spine: the Universal Clamp. Eur Spine J 18:158–169. doi:10.1007/s00586-008-0839-y
Jouve JL, de Gauzy JS, Blondel B, Launay F, Accadbled F, Bollini G (2010) Use of the Universal Clamp for deformity correction and as an adjunct to fusion: preliminary results in scoliosis. J Child Orthop 4:73–80. doi:10.1007/s11832-009-0221-6
La Rosa G, Giglio G, Oggiano L (2013) The Universal Clamp hybrid system: a safe technique to correct deformity and restore kyphosis in adolescent idiopathic scoliosis. Eur Spine J 22:S823–S828. doi:10.1007/s00586-013-3014-z
Pesenti S, Chalopin A, Peltier E, Choufani E, Ollivier M, Fuentes S, Blondel B, Jouve JL (2016) How sublaminar bands affect postoperative sagittal alignment in AIS patients with preoperative hypokyphosis? Results of a series of 34 patients with 2-year follow-up. Biomed Res Int 1954712. doi: 10.1155/2016/1954712
Rodriguez-Martinez NG, Safavi-Abbasi S, Perez-Orribo L et al (2015). Biomechanics of a flexible sublaminar connector in long-segment thoracic fixation. J Neurosurg Spine 1–7. doi: 10.3171/2015.4.spine14999
Fleming JE Jr, Cornell CN, Muschler GF (2000) Bone cells and matrices in orthopedic tissue engineering. Orthop Clin North Am 31:357–374
Sandhu HS, Grewal HS, Parvataneni H (1999) Bone grafting for spinal fusion. Orthop Clin North Am 30:685–698
Costa Mendes L, Sauvigné T, Guiol J (2016) Morbidity of autologous bone harvesting in implantology: literature review from 1990 to 2015. Rev Stomatol Chir Maxillofac Chir Orale 117:388–402. doi:10.1016/j.revsto.2016.09.003
Kim DH, Rhim R, Li L et al (2009) Prospective study of iliac crest bone graft harvest site pain and morbidity. Spine J 9:886–892. doi:10.1016/j.spinee.2009.05.006
Fabry G (1991) Allograft versus autograft bone in idiopathic scoliosis surgery: a multivariate statistical analysis. J Pediatr Orthop 11:465–468
Crawford CH, Carreon LY, Lenke LG et al (2013) Outcomes following posterior fusion for adolescent idiopathic scoliosis with and without autogenous iliac crest bone graft harvesting. Spine Deform 1:144–147. doi:10.1016/j.jspd.2012.12.001
Lansford TJ, Burton DC, Asher MA et al (2013) Radiographic and patient-based outcome analysis of different bone-grafting techniques in the surgical treatment of idiopathic scoliosis with a minimum 4-year follow-up: allograft versus autograft/allograft combination. Spine J 13:523–529. doi:10.1016/j.spinee.2013.01.025
Devine JG (2013) Bone grafting techniques in idiopathic scoliosis: a confirmation that allograft is as good as autograft but dispels the purported pain associated with the iliac crest bone graft harvest. Spine J 13:530–531. doi:10.1016/j.spinee.2013.02.047
Mroz TE, Joyce MJ, Lieberman IH et al (2009) The use of allograft bone in spine surgery: is it safe? Spine J 9:303–308. doi:10.1016/j.spinee.2008.06.452
Lerner T, Bullmann V, Schulte TL, Schneider M, Liljenqvist U (2009) A level-1 pilot study to evaluate of ultraporous beta-tricalcium phosphate as a graft extender in the posterior correction of adolescent idiopathic scoliosis. Eur Spine J 18:170–179. doi:10.1007/s00586-008-0844-1
Muschik M, Ludwig R, Halbhubner S et al (2001) Beta/tricalcium phosphate as a bone substitute for dorsal spinal fusion in adolescent idiopathic scoliosis: preliminary results of a prospective clinical study. Eur Spine J 10:S178–S184
Ilharreborde B, Morel E, Fitoussi F (2008) Bioactive glass as a bone substitute for spinal fusion in adolescent idiopathic scoliosis: a comparative study with iliac crest autograft. J Pediatr Orthop 28:347–351. doi:10.1097/BPO.0b013e318168d1d4
Ransford AO, Morley T, Edgar MA et al (1998) Synthetic porous ceramic compared with autograft in scoliosis surgery. A prospective, randomized study of 341 patients. J Bone Joint Surg Br 80:13–18
Faundez A, Tournier C, Garcia M, Aunoble S, Le Huec JC (2016) Bone morphogenetic protein use in spine surgery-complications and outcomes: a systematic review. Int Orthop 40:1309–1319. doi:10.1007/s00264-016-3149-8
Kamerlink JR, Quirno M, Auerbach JD et al (2010) Hospital cost analysis of adolescent idiopathic scoliosis correction surgery in 125 consecutive cases. J Bone Joint Surg Am 92:1097–1104. doi:10.2106/JBJS.I.00879
Lindaman LM (2001) Bone healing in children. Clin Podiatr Med Surg 18:97–108
Acknowledgements
SP received a grant from the SOFCOT and the SOFOP.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests regarding this study.
Rights and permissions
About this article
Cite this article
Pesenti, S., Ghailane, S., Varghese, J.J. et al. Bone substitutes in adolescent idiopathic scoliosis surgery using sublaminar bands: is it useful? A case-control study. International Orthopaedics (SICOT) 41, 2083–2090 (2017). https://doi.org/10.1007/s00264-017-3512-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3512-4