Abstract
Background
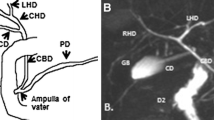
Magnetic resonance imaging/cholangiopancreatography (MRI/MRCP) is now an essential imaging modality for the evaluation of biliary and pancreatic pathology in children, but there are no data depicting the normal diameters of the common bile duct (CBD) and pancreatic duct. Recognition of abnormal duct size is important and the increasing use of MRCP necessitates normal MRI measurements.
Objective
To present normal MRI measurements for the common bile duct and pancreatic duct in children.
Materials and methods
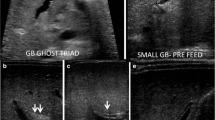
In this retrospective study we searched all children ages birth to 10 years in our MR urography (MRU) database from 2006 until 2013. We excluded children with a history of hepatobiliary or pancreatic surgery. We stratified 204 children into five age groups and retrospectively measured the CBD and the pancreatic duct on 2-D axial and 3-D coronal T2-weighted sequences. We performed statistical analysis, using logistic and linear regressions to detect the age association of the visibility and size of the duct measurements. We used non-parametric tests to detect gender and imaging plane differences.
Results
Our study included 204 children, 106 (52%) boys and 98 (48%) girls, with a median age of 33 months (range 0–119 months). The children were distributed into five age groups. The common bile duct was visible in all children in all age groups. The pancreatic duct was significantly less visible in the youngest children, group 1 (54/67, 80.5%; P = 0.003) than in the oldest children, group 5 (22/22, 100%). In group 2 the pancreatic duct was seen in 19/21 (90.4%), in group 3 52/55 (94.5%), and in group 4 39/39 (100%). All duct measurements increased with age (P < 0.001; r-value > 0.423), and the incremental differences between ages were significant. The measurement variations between the axial and coronal planes were statistically significant (P < 0.001); however these differences were fractions of millimeters. For example, in group 1 the mean coronal measurement of the CBD was 2.1 mm and the axial measurement was 2.0 mm; the mean coronal measurement of the pancreatic duct was 0.9 mm and the axial measurement was 0.8 mm.
Conclusion
Our study provides normative measurements for the common bile duct and pancreatic duct for children up to age 10 years. The upper limits of the CBD and pancreatic duct increase with age, and the values range 1.1–4.0 mm for the CBD and 0.6–1.9 mm for the pancreatic duct.



Similar content being viewed by others
References
Goldman M, Pranikoff T (2011) Biliary disease in children. Curr Gastroenterol Rep 13:193–201
Darge K, Anupindi S (2009) Pancreatitis and the role of US, MRCP and ERCP. Pediatr Radiol 39:S153–157
Darge K, Anupindi SA, Jaramillo D (2011) MR imaging of the abdomen and pelvis in infants, children, and adolescents. Radiology 261:12–29
Anupindi SA, Victoria T (2008) Magnetic resonance cholangiopancreatography: techniques and applications. Magn Reson Imaging Clin N Am 16:453–466
Egbert ND, Bloom DA, Dillman JR (2013) Magnetic resonance imaging of the pediatric pancreaticobiliary system. Magn Reson Imaging Clin N Am 21:681–696
Goske MJ, Applegate KE, Boylan J et al (2008) The Image Gently campaign: working together to change practice. AJR Am J Roentgenol 190:273–274
Konus OL, Ozdemir A, Akkaya A et al (1998) Normal liver, spleen, and kidney dimensions in neonates, infants, and children: evaluation with sonography. AJR Am J Roentgenol 171:1693–1698
Kahramaner Z, Erdemir A, Cicek E et al (2013) Reference ranges for sonographic dimensions of the liver and spleen in preterm infants. Pediatr Radiol 43:1464–1474
Erdemir A, Kahramaner Z, Cicek E et al (2013) Reference ranges for sonographic renal dimensions in preterm infants. Pediatr Radiol 43:1475–1484
Hernanz-Schulman M, Ambrosino MM, Freeman PC et al (1995) Common bile duct in children: sonographic dimensions. Radiology 195:193–195
Siegel MJ, Martin KW, Worthington JL (1987) Normal and abnormal pancreas in children: US studies. Radiology 165:15–18
Chao HC, Lin SJ, Kong MS et al (2000) Sonographic evaluation of the pancreatic duct in normal children and children with pancreatitis. J Ultrasound Med 19:757–763
Mortele KJ, Rocha TC, Streeter JL et al (2006) Multimodality imaging of pancreatic and biliary congenital anomalies. Radiographics 26:715–731
Delaney L, Applegate KE, Karmazyn B et al (2008) MR cholangiopancreatography in children: feasibility, safety, and initial experience. Pediatr Radiol 38:64–75
Arcement CM, Meza MP, Arumanla S et al (2001) MRCP in the evaluation of pancreaticobiliary disease in children. Pediatr Radiol 31:92–97
Almehdar A, Chavhan GB (2013) MR cholangiopancreatography at 3.0 T in children: diagnostic quality and ability in assessment of common paediatric pancreatobiliary pathology. Br J Radiol 86:20130036
Chavhan GB, Almehdar A, Moineddin R et al (2013) Comparison of respiratory-triggered 3-D fast spin-echo and single-shot fast spin-echo radial slab MR cholangiopancreatography images in children. Pediatr Radiol 43:1086–1092
Edelman RR (2007) MR imaging of the pancreas: 1.5 T versus 3 T. Magn Reson Imaging Clin N Am 15:349–353
Trout AT, Podberesky DJ, Serai SD et al (2013) Does secretin add value in pediatric magnetic resonance cholangiopancreatography? Pediatr Radiol 43:479–486
Sandrasegaran K, Cote GA, Tahir B et al (2014) The utility of secretin-enhanced MRCP in diagnosing congenital anomalies. Abdom Imaging 39:979–987
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gwal, K., Bedoya, M.A., Patel, N. et al. Reference values of MRI measurements of the common bile duct and pancreatic duct in children. Pediatr Radiol 45, 1153–1159 (2015). https://doi.org/10.1007/s00247-015-3296-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-015-3296-x