Abstract
Introduction
Complex functional movements such as jumping typically provoke stress urinary incontinence (SUI) in women. The aim of this study was to investigate pelvic floor muscle (PFM) activity in young, healthy women during jumps to explore their activity characteristics.
Methods
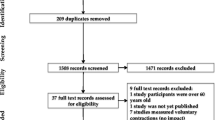
Surface electromyography (EMG) from PFMs was measured in 16 healthy women with a tripolar vaginal probe during drop landings from heights of 15, 30 and 45 cm (DL 15, 30, 45) as well as during mini-trampolining with a pace of 90 and 75 jumps per minute (MT 90, 75). Time of foot strike and body weight force (BWF) in % (= ground reaction force, normalised to body weight) was determined by force plates. Root mean square values of the EMG signals were analyzed from 30 ms before to 150 ms after foot strike. Peak activity during maximum voluntary contraction (MVC) was set as 100% for EMG normalization. The PFM onset threshold was determined as the mean of rest activity plus 2 standard deviations. Data were analysed with non-parametric statistical methods.
Results
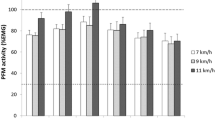
EMG activity during all jumps was above the PFM onset threshold. Mean pre- and reflex activity increased significantly with jumping height (p < 0.05) as well as with increasing BWF. The PFM activation pattern of DL was with peak activity of 115–182 %MVC between 34 and 44 ms after foot strike, which was different from MT with peak PFM activity of 85–115 %MVC reached at 133 ms.
Conclusions
Jumping and mini-trampolining provoked significant PFM activity in healthy volunteers. The next research step will be to examine the PFM activity of women suffering from SUI during jumps.



Similar content being viewed by others
Abbreviations
- AM:
-
Abdominal muscle
- bpm:
-
Beats per minute
- BWF:
-
Body weight force: ground reaction force, normalized to body weight
- DL:
-
Drop landing
- DL 15, 30, 45:
-
Drop landings from heights of 15, 30 and 45 cm
- EMG:
-
Electromyography
- GRF:
-
Ground reaction force
- IAP:
-
Intraabdominal pressure
- MT:
-
Mini-trampolining
- MT 90, 75:
-
Mini-trampolining with a pace of 90 and 75 jumps per minute
- MVC:
-
Maximum voluntary contraction
- % MVC:
-
Maximum voluntary contraction normalised to peak activity
- PFM:
-
Pelvic floor muscle
- PFMT:
-
Pelvic floor muscle training
- RMS:
-
Root mean square
- SUI:
-
Stress urinary incontinence
- TAS:
-
Tegner activity scale (questionnaire)
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20. https://doi.org/10.1002/nau.20798.
Tennstedt SL, Link CL, Steers WD, McKinlay JB. Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults the Boston Area Community Health (BACH) survey. Am J Epidemiol. 2008;167(4):390–9. https://doi.org/10.1093/aje/kwm356.
Bø K. Urinary incontinence, pelvic floor dysfunction, exercise and sport. Sports Med. 2004;34(7):451–64.
Said MLN, Olfa N, Hamda M. Effects of high-impact aerobics vs. low-impact aerobics and strength training in overweight and obese women. J Sports Med Phys Fitness. 2017;57(3):278–88. https://doi.org/10.23736/S0022-4707.16.05857-X.
Fozzatti C, Riccetto C, Herrmann V, Brancalion MF, Raimondi M, Nascif CH, et al. Prevalence study of stress urinary incontinence in women who perform high-impact exercises. Int Urogynecol J. 2012;23(12):1687–91. https://doi.org/10.1007/s00192-012-1786-z.
Eliasson K, Larsson T, Mattsson E. Prevalence of stress incontinence in nulliparous elite trampolinists. Scand J Med Sci Sports. 2002;12(2):106–10.
Kruger JA, Murphy BA, Heap SW. Alterations in levator ani morphology in elite nulliparous athletes: a pilot study. Aust N Z J Obstet Gynaecol. 2005;45(1):42–7. https://doi.org/10.1111/j.1479-828X.2005.00349.x.
Kruger JA, Dietz HP, Murphy BA. Pelvic floor function in elite nulliparous athletes. Ultrasound Obstet Gynecol. 2007;30(1):81–5. https://doi.org/10.1002/uog.4027.
Syan R, Brucker BM. Guideline of guidelines: urinary incontinence. BJU Int. 2016;117(1):20–33. https://doi.org/10.1111/bju.13187.
Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth international consultation on incontinence recommendations of the international scientific committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213–40. https://doi.org/10.1002/nau.20870.
Hay-Smith EJ, Herderschee R, Dumoulin C, Herbison GP. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev. 2011;12:CD009508. https://doi.org/10.1002/14651858.CD009508.
Junginger B, Seibt E, Baessler K. Bladder-neck effective, integrative pelvic floor rehabilitation program: follow-up investigation. Eur J Obstet Gynecol Reprod Biol. 2014;174:150–3. https://doi.org/10.1016/j.ejogrb.2013.12.022.
Leitner M, Moser H, Eichelberger P, Kuhn A, Radlinger L. Evaluation of pelvic floor muscle activity during running in continent and incontinent women: an exploratory study. Neurourol Urodyn. 2016;36(6):1570–6.
Luginbuehl H, Naeff R, Zahnd A, Baeyens JP, Kuhn A, Radlinger L. Pelvic floor muscle electromyography during different running speeds: an exploratory and reliability study. Arch Gynecol Obstet. 2016;293(1):117–24. https://doi.org/10.1007/s00404-015-3816-9.
Morin M, Bourbonnais D, Gravel D, Dumoulin C, Lemieux MC. Pelvic floor muscle function in continent and stress urinary incontinent women using dynamometric measurements. Neurourol Urodyn. 2004;23(7):668–74. https://doi.org/10.1002/nau.20069.
Shishido K, Peng Q, Jones R, Omata S, Constantinou CE. Influence of pelvic floor muscle contraction on the profile of vaginal closure pressure in continent and stress urinary incontinent women. J Urol. 2008;179(5):1917–22. https://doi.org/10.1016/j.juro.2008.01.020.
Luginbuehl H, Lehmann C, Baeyens JP, Kuhn A, Radlinger L. Involuntary reflexive pelvic floor muscle training in addition to standard training versus standard training alone for women with stress urinary incontinence: study protocol for a randomized controlled trial. Trials [Electronic Resource]. 2015;16:524. https://doi.org/10.1186/s13063-015-1051-0.
Laycock J, Jerwood D. Pelvic floor muscle assessment: the PERFECT scheme. Physiotherapy. 2001;87(12):631–42.
Hodges PW, Bui BH. A comparison of computer-based methods for the determination of onset of muscle contraction using electromyography. Electroencephalogr Clin Neurophysiol. 1996;101(6):511–9.
Fleischmann J, Gehring D, Mornieux G, Gollhofer A. Load-dependent movement regulation of lateral stretch shortening cycle jumps. [Erratum appears in Eur J Appl Physiol. 2010 Sep;110(1):189-90]. Eur J Appl Physiol. 2010;110(1):177–87. https://doi.org/10.1007/s00421-010-1476-9.
Kramers-de Quervain IA, Stüssi E, Stacoff A. Ganganalyse beim gehen und laufen. Schweizerische Zeitschrift für Sportmedizin und Sporttraumatologie. 2008;56(2):35–42.
Santello M. Review of motor control mechanisms underlying impact absorption from falls. Gait Posture. 2005;21(1):85–94. https://doi.org/10.1016/j.gaitpost.2004.01.005.
Keshwani N, McLean L. A differential suction electrode for recording electromyographic activity from the pelvic floor muscles: crosstalk evaluation. J Electromyogr Kinesiol. 2013;23(2):311–8. https://doi.org/10.1016/j.jelekin.2012.10.016.
Flury N, Koenig I, Radlinger L. Crosstalk considerations in studies evaluating pelvic floor muscles using surface electromyography in women: a scoping review. Arch Gynecol Obstet. 2017;1-11.
Keshwani N, McLean L. State of the art review: intravaginal probes for recording electromyography from the pelvic floor muscles. Neurourol Urodyn. 2015;34(2):104–12. https://doi.org/10.1002/nau.22529.
Junginger B, Baessler K, Sapsford R, Hodges PW. Effect of abdominal and pelvic floor tasks on muscle activity, abdominal pressure and bladder neck. Int Urogynecol J. 2010;21(1):69–77. https://doi.org/10.1007/s00192-009-0981-z.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Saeuberli, P.W., Schraknepper, A., Eichelberger, P. et al. Reflex activity of pelvic floor muscles during drop landings and mini-trampolining—exploratory study. Int Urogynecol J 29, 1833–1840 (2018). https://doi.org/10.1007/s00192-018-3664-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3664-9