Abstract
Objective
The aim of this study was to assess the incidence of de novo stress urinary incontinence (SUI) and sonographic features of implanted transvaginal mesh in continent women treated with Elevate™ anterior/apical [single-incision mesh (SIM-A)] or Perigee™ [transvaginal mesh with sacrospinous fixation (TVM + SSF)] in extensive pelvic organ reconstruction surgery.
Methods
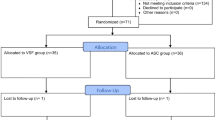
This prospective observational study was done from May 2010 to January 2013. Patients were recruited from two tertiary centers, and the Elevate™ and Perigee™ systems were compared. Patients who had overt or occult SUI, previous prolapse or mesh insertion were excluded.
Result
Fifty-seven patients in the SIM-A group and sixty-one in the TVM + SSF group were analysed. All completed a minimum of 1-year follow-up. Groups were demographically and statistically similar. There was a significantly high incidence of de novo SUI postoperatively in the SIM-A group. The objective and subjective cure rate of pelvic organ prolapse (POP) were comparable between groups, with incidence of mesh erosion in the SIM-A group and three in the TVM + SSF group. Sonographic evaluation showed significant increase in mesh length in the SIM-A group.
Conclusion
Elevate™ a offered lower incidence of mesh erosion and comparable results on anatomical POP correction; however, incidence of de novo SUI was high. There is an apparent lengthening of implanted Elevate® mesh sonographically.

Similar content being viewed by others
References
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89(4):501–506
Wu JM. Mathew CA. Conuvar M (2014) Lifetime Risk of Stress Urinary Incontinence or Pelvic Organ Prolapse Surgery. Obstetrics ang Gynecology. May 6. e published
Blandon RE, Bharuch AE, Melton LJ et al (2007) Incidence of pelvic floor repair after hysterectomy: a population-based cohort study. Am J Obstet Gynecol 197(664):e.1–e.7
Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B (2007) Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (prolift technique)–a case series multicentric study. Int Urogynecol J Pelvic Floor Dysfunct 18(7):743–752
Abdel-Fattah M, Ramsay I (2008) West of scotland study G. retrospective multicentre study of the new minimally invasive mesh repair devices for pelvic organ prolapse. BJOG An Int J Obstet Gynaecol 115(1):22–30
Halaska M, Maxova K, Sottner O, Svabik K, Mlcoch M, Kolarik D et al (2012) A multicenter, randomized, prospective, controlled study comparing sacrospinous fixation and transvaginal mesh in the treatment of posthysterectomy vaginal vault prolapse. Am J Obstet Gynecol 207(4):301, e1–7
Food and Drug Administration (FDA) (2011) FDA Safety Communication: UPDATE on Serious Complications Associated With Transvaginal Placement of Surgical Mesh for Pelvic Organ Prolapse. Silver Spring, MD: FDA; 2011. Available at: http://www.fda.gov/Medical Devices/ Safety/AlertsandNotices/ucm.262435.htm. Accessed
Borstad E, Rud T (1989) The risk of developing urinary stress incontinence after vaginal repair in continent women. a clinical and urodynamic follow-up study. Acta Obstet Gynecol Scand 68:545–549
Brubaker L, Cundiff GW, Fine P et al (2006) Abdominal sacrocolpopexy with Burch colposuspension to reduce urinary stress incontinence. N Engl J Med 354:1557–1566
Ellstrom Engh AM, Ekeryd A, Magnusson A, Olsson I, Otterlind L, Tobiasson G (2011) Can de novo stress incontinence after anterior wall repair be predicted? Acta Obstet Gynecol Scand 90:488–493
Dietz HP, Shek C, Rane A (2006) Perigee transobturator mesh implant for the repair of large and recurrent cystocele. Int Urogynecol J 17:S139
Tunn R, Picot A, Marschke J, Gauruder-Burmester A (2007) Sonomorphological evaluation of polypropylene mesh implants after vaginal mesh repair in women with cystocele or rectocele. Ultrasound Obstet Gynecol 29:449–452
Svabik K, Martan A, Masata J, El Haddad R (2011) Ultrasound appearances after mesh implantation – evidence of mesh contraction or folding? Int Urogynecol J 22:529
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175(1):10–17
Shumaker SA, Wyman JF, Uebersax JS, McClish D, Fantl JA (1994) Health-related quality of life measures for women with urinary incontinence: the incontinence impact questionnaire and the urogenital distress inventory. continence program in women (CPW) research group. Qual Life Res Int J Qual Life Asp Treat Care Rehabil 3(5):291–306
Barber MD, Walters MD, Bump RC (2005) Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193(1):103–113
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C (2003) A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct 14(3):164–168, discussion 8
Su TH, Lau HH (2010) Validation of a Chinese version of the short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire. J Sex Med 7(12):3940–3945
Lo TS, Pue LB, Tan YL, Wu PY (2014) Long-term outcomes of synthetic transobturator nonabsorbable anterior mesh versus anterior colporrhaphy in symptomatic, advanced pelvic organ prolapse surgery. Int Urogynecol J 25(2):257–264
Miyazaki FS (1987) Miya Hook ligature carrier for sacrospinous ligament suspension. Obstet Gynecol 70(2):286–288
Lo TS, Ashok K (2011) Combined anterior trans-obturator mesh and sacrospinous ligament fixation in women with severe prolapse–a case series of 30 months follow-up. Int Urogynecol J 22(3):299–306
Lo TS, Ashok K (2011) Recurrent mesh erosion and retro pubic abscess following anterior intravaginal slingplasty. J Obstet Gynaecol Res 37(4):363–365
Azais H, Charles CJ, Delporte P, Debodinance P (2012) Prolapse repair using the Elevate kit: prospective study on 70 patients. Int Urogynecol J 23(10):1421–1428
Wei JT, Nygaard I, Richter HE et al (2012) A midurethral sling to reduced incontinence after vaginal prolapse repair. N Engl J Med 366:2358
Al-Mandeel H, Ross S, Robert M, Milne J (2011) Incidence of stress urinary incontinence following vaginal repair of pelvic organ prolapse in objectively continent women. Neurourol Urodyn 30(3):390–394
Kasturi S, Diaz SI, McDermott CD, Woodman PJ, Bump RC, Terry CL et al (2011) De novo stress urinary incontinence after negative prolapse reduction stress testing for total vaginal mesh procedures: incidence and risk factors. Am J Obstet Gynecol 205(5):487, e1–4
Aungst MJ, Friedman EB, von Pechmann WS, Horbach NS, Welgoss JA (2009) De novo stress incontinence and pelvic muscle symptoms after transvaginal mesh repair. Am J Obstet Gynecol 201(1):73, e1–7
Hafidh BA. Chou Q. Khalil MM. Al-Mandeel H. De novo stress urinary incontinence after vaginal repair for pelvic organ prolapse: one-year follow-up. European journal of obstetrics, gynecology, and reproductive biology. 2013;168(2):227-30.of obstetrics and gynecology. 2009;201(1):73 e1-e7.
Lo TS (2010) One-year outcome of concurrent anterior and posterior transvaginal mesh surgery for treatment of advanced urogenital prolapse: case series. J Minim Invasive Gynecol 17(4):473–479
Jelovsek JE, Chagin K, Brubaker L et al (2014) A model for predicting the risk of de novo stress urinary incontinence in women undergoing pelvic organ prolapse surgery. Am Coll Obstet Gynecol 123:279–287. doi:10.1097/AOG.000000000000094
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lo, TS., bt Karim, N., Cortes, E.F.M. et al. Comparison between Elevate Anterior/Apical system and Perigee system in pelvic organ prolapse surgery: clinical and sonographic outcomes. Int Urogynecol J 26, 391–400 (2015). https://doi.org/10.1007/s00192-014-2492-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2492-9