Abstract
Introduction and hypothesis
To compare the efficacy and safety of iliococcygeus fixation (ICG) and abdominal sacral colpopexy (SCP) in the treatment of vaginal vault prolapse.
Methods
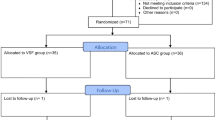
Patients with symptomatic vaginal vault prolapse after hysterectomy were considered in this analysis. Surgical outcomes, i.e., the capacity to restore the anatomy of the vaginal cuff and improvement in the prolapse-related symptoms were compared. Continuous variables were compared using the Student’s t test, while non-continuous variables using a Chi-squared test or Fisher’s exact test.
Results
Sacrocolpopexy was performed in 41 patients, while ICG fixation was carried out in 36 patients. Operative time was significantly shorter (78 vs 140 min, p < 0.001) and median blood loss higher in the ICG group (150 ml vs 100 ml, p=0.01). The rates of postoperative complications of the two groups were not statistically different. Relapse rate was similar in the two groups (15 % in the SCP and 22 % in the ICG group respectively, p=0.36). Considering the POP-Q score, both SCP and ICG achieved a significant and comparable correction of vaginal prolapse. The evaluation of postoperative subjective symptoms revealed a significant improvement in voiding and vaginal bulging related to pelvic organ prolapse in both groups.
Conclusions
Both ICG fixation and SCP are effective in restoring normal anatomy in patients with vaginal vault prolapse and in relieving associated symptoms. Owing to its lower morbidity and to the advantage of not using a synthetic device, ICG might be an excellent option for the treatment of recurrent vaginal vault prolapse following hysterectomy.
Similar content being viewed by others
References
Weber AM, Abrams P, Brubaker L, Cundiff G, Davis G, Dmochowski RR, Fischer J, Hull T, Nygaard I, Weidner AC (2001) The standardization of terminology for researchers in female pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct 12(3):178–186
Maher C (2010) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 14(4), CD004014
Flynn BJ, Webster GD (2002) Surgical management of the apical vaginal defect. Curr Opin Urol 12(4):353–358
Maher CF, Qatawneh AM, Dwyer PL, Carey MP, Cornish A, Schluter PJ (2004) Abdominal sacral colpopexy or vaginal sacrospinous colpopexy for vaginal vault prolapse: a prospective randomized study. Am J Obstet Gynecol 190(1):20–26
Lane FE (1962) Repair of posthysterectomy vaginal-vault prolapse. Obstet Gynecol 20:72–77
Inmon WB (1963) Pelvic relaxation and repair including prolapse of vagina following hysterectomy. South Med J 56:577–582
Shull BL, Capen CV, Riggs MW, Kuehl TJ (1993) Bilateral attachment of the vaginal cuff to iliococcygeus fascia: an effective method of cuff suspension. Am J Obstet Gynecol 168(6 Pt 1):1669–1674
Medina CA, Croce C, Candiotti K, Takacs P (2008) Comparison of vaginal length after iliococcygeus fixation and sacrospinous ligament fixation. Int J Gynaecol Obstet 100(3):267–270
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Amid PK (1997) Classification of biomaterials and their related complications in abdominal wall hernia surgery. Hernia 1:15–21
Benson JT, Lucente V, McClellan E (1996) Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: a prospective randomized study with long-term outcome evaluation. Am J Obstet Gynecol 175:418
Gilleran JP, Zimmern P (2009) Abdominal mesh sacrocolpopexy for recurrent triple-compartment pelvic organ prolapse. BJU Int 103:1090–1094
Scarpero HM, Cespedes RD, Winters JC (2001) Transabdominal approach to repair of vaginal vault prolapse. Tech Urol 7(2):139–145
Addison WA, Timmons MC (1993) Abdominal approach to vaginal eversion. Clin Obstet Gynecol 36:995
Baessler K, Schuessler B (2001) Abdominal sacrocolpopexy and anatomy and function of the posterior compartment. Obstet Gynecol 97(5 Pt 1):678–684
Tan-Kim J, Menefee SA, Luber KM, Nager CW, Lukacz ES (2011) Prevalence and risk factors for mesh erosion after laparoscopic-assisted sacrocolpopexy. Int Urogynecol J 22(2):205–212
Culligan PJ, Blackwell L, Goldsmith LJ et al (2005) A randomized controlled trial comparing fascia lata and synthetic mesh for sacral colpopexy. Obstet Gynecol 106:29–37
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Milani, R., Cesana, M.C., Spelzini, F. et al. Iliococcygeus fixation or abdominal sacral colpopexy for the treatment of vaginal vault prolapse: a retrospective cohort study. Int Urogynecol J 25, 279–284 (2014). https://doi.org/10.1007/s00192-013-2216-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-013-2216-6