Abstract
Purpose
The aim of the present study was to evaluate the impact of the coronavirus (COVID-19) pandemic on joint arthroplasty service in Europe by conducting an online survey of arthroplasty surgeons.
Methods
The survey was conducted in the European Hip Society (EHS) and the European Knee Associates (EKA). The survey consisted of 20 questions (single, multiple choice, ranked). Four topics were addressed: (1) origin and surgical experience of the participant (four questions); (2) potential disruption of arthroplasty surgeries (12 questions); (3) influence of the COVID-19 pandemic on the particular arthroplasty surgeon (four questions); (4) a matrix provided 14 different arthroplasty surgeries and the participant was asked to state whether dedicated surgery was stopped, delayed or cancelled.
Results
Two-hundred and seventy-two surgeons (217 EHS, 55 EKA) from 40 different countries participated. Of the respondents, 25.7% stated that all surgeries were cancelled in their departments, while 68.4% responded that elective inpatient procedures were no longer being performed. With regard to the specific surgical procedures, nearly all primary TJA were cancelled (92.6%) as well as aseptic revisions (94.7%). In most hospitals, periprosthetic fractures (87.2%), hip arthroplasty for femoral neck fractures and septic revisions for acute infections (75.8%) were still being performed.
Conclusion
During the current 2020 COVID-19 pandemic, we are experiencing a near-total shutdown of TJA. A massive cutback was observed for primary TJA and revision TJA, even in massively failed TJA with collapse, dislocation, component failure or imminent dislocation. Only life-threatening pathologies like periprosthetic fractures and acute septic TJA are currently undergoing surgical treatment.
Level of evidence
V.
Similar content being viewed by others
Introduction
The public health disruption in Europe caused by the Coronavirus disease 2019 (COVID-19) pandemic has resulted in a significant reallocation of health care resources with the focus on the management of COVID 19 patients [16]. COVID-19 has rapidly become a global public health threat, endangering the health and well-being of all people, but especially vulnerable older populations [13]. The pandemic is also causing social disruption, exceptional healthcare utilization, and economic instability worldwide. The Organisation for Economic Co-operation and Development (OECD) recently reported that for each month of containment, there is a loss of 2 percentage points in annual GDP (growth domestic product) growth. OECD further stated that the tourism sector alone is facing a decrease up to 70% [6].
Controlling the spread of COVID-19 has become the singular focus of most countries in Europe, with unprecedented international collaboration and rapid dissemination of emerging scientific evidence. Until now, most publications have described demographic characteristics, clinical symptoms, biological behaviour, and radiological or pathological findings associated with COVID-19 [17].
Pandemics like the COVID-19 disease or the Spanish flu have wrought massive changes in patient care [19]. Most healthcare resources as well as medical staff are needed to take care of COVID-19 infections. Hence, it can be presumed that joint arthroplasty service has substantially declined over recent weeks throughout Europe [5]. Asian orthopaedic surgeons based on the lessons learned from SARS in 2003 postponed or cancelled all elective surgeries requiring > 23 h of hospitalization which predominantly affected joint arthroplasty [3].
It is well known from other medical disciplines that a reduction in major organ transplantation (> 25%) as well as a significant reduction in colorectal surgery, and concerns about urology patients, especially in those with a malignant tumour, have already been reported during the COVID-19 pandemic [2, 4, 10].
Over the last decades, total joint arthroplasty (TJA) has grown rapidly and proved its added value for the benefit of nationwide healthcare and patients [14]. The outbreak of COVID-19 in Europe has potentially influenced the frequency of elective surgeries, like primary and revision arthroplasty. The members of the European Hip Society (EHS) and the European Knee Associates (EKA) are predominantly arthroplasty surgeons and a cohort with great expertise in arthroplasty. Consequently, we surveyed the members of the EHS and the EKA regarding the COVID-19 pandemic and its influence on their work.
The aim of the present study was to evaluate the impact of the COVID-19 pandemic on joint arthroplasty service in Europe by means of an online survey of arthroplasty surgeons in the EHS and the EKA.
Materials and methods
A prospective online survey of the members of two European orthopaedic societies was performed: EHS and EKA. The EHS, consisting of 510 members (328 of them are European full members), was founded in 1992, and its aim is “to provide a forum for the discussion of research, advances in clinical practice and the results of predominantly surgical procedures of all types relating to the hip joint” (Art. 2a EHS Constitution) and a special focus is on hip replacement. The European Knee Associates (EKA) is a section of the European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA). Within ESSKA, the EKA is an association particularly dealing with the management of degenerative diseases of the knee joint. Consequently, its members focus on knee arthroplasty and osteotomy around the knee. The EKA currently has 208 members.
No approval was obtained from an institutional review board, because the survey was anonymous and no patient data were included. Data were collected using SurveyMonkey (https://www.surveymonkey.com): an online data collection program.
The survey consisted of 20 questions (single/multiple choice and ranked questions) and was conducted from March 30, 2020, to April 10, 2020 (see Online Appendix 1 for survey details). Four main topics were addressed: (1) origin and surgical experience of the participant (four questions); (2) potential disruption of arthroplasty surgeries (12 questions); (3) influence of the pandemic on the particular arthroplasty surgeon (four questions); (4) a matrix provided 14 different arthroplasty surgeries and the participant was asked to state whether the dedicated surgery was stopped, delayed or cancelled at her or his department.
A link to the above-mentioned survey was sent to the members of both societies via email and society’s newsletter. All data gathered from the online database were calculated as frequencies and percentages.
Results
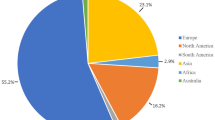
A total of 272 surgeons (217 EHS, 55 EKA) participated in the present survey. The participating surgeons were on average 20 years (min: 1 year, max: 47 years) in practice. The majority worked at an academic centre (44.6%) and a private hospital (44.5%), while 37.1% worked in a public hospital. Arthroplasty surgeons from 40 different countries responded. The majority lived in Italy (13.9%), Germany (9.6%) and France (8.1%). 64.6% had received a specific COVID-19 training.
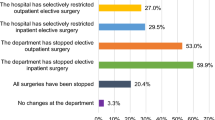
Of the respondents 25.7% stated that all surgeries were cancelled in their departments, while 68.4% responded that elective inpatient procedures were no longer being performed, and 68% reported that all outpatient procedures were cancelled. Elective inpatient and outpatient surgery was also restricted, namely to 20.6% and 15.4%, respectively. Only 0.7% of the respondents reported no changes at their department. On a four-level scale of escalation, 52.6% stated that they are at the last stage, treating only life-threatening diseases (Fig. 1).
Only 5.9% of the participants stated that they were still doing primary TJA (Table 1; Fig. 2). Regarding routine aseptic revisions, only 3.8% of the participants reported that they were still performing such procedures. In most hospitals, periprosthetic fractures (87.2%), total hip arthroplasty/hemiarthroplasty for femoral neck fractures and septic revisions for acute infections (75.8%) were still being performed. Second-stage revisions with re-implantation of the implants were being performed by 18.8% of the respondents. 50.9% of the participants reported that massively failed TJA (collapse, dislocation, component failure, imminent dislocation) were still going on and 25.8% that endoprosthetic reconstruction after malignant resection was being operated at their department.
The vast majority (82.6%) of arthroplasty surgeons stated that their personal surgical volume was drastically reduced, a delay in surgeries was reported by 50.7%, training or teaching of students, residents and fellows was stopped for 52.2% of the surgeons and more conservative clinical care was being performed by 20.4% of the respondents. Of the arthroplasty surgeons, 46.7% were performing more administrative work than usual, 39.3% were even allocated to non-orthopaedic duties and 53% stated that they were effectively not working due to institutional or self-imposed deferral of elective surgery.
Regarding post-operative follow-up, 45.7% stated that they were following only high-risk patients after TJA. Of the surgeons, 31.6% and 25.7% reported that they were still doing normal clinical and radiologic follow-ups, respectively (Fig. 3). Rehabilitation and physical therapy after TJA were available for selected cases (40.8%), for inpatient patients (16.5%), for outpatient patients (28.7%), and no physical therapy or rehabilitation after TJA was reported in 30.1% of cases.
Of the surgeons, 21.3% stated that they tried to keep a distance to their families, 22.6% reported that they avoided physical contact with their families and 21.7% performed surface disinfection at home. Likewise, 5.5% lived in separate rooms at home, 2.9% stated that they do not even go home anymore, and 15.8% were on vacancy during the pandemic.
The majority of respondents knew either patients and/or hospital staff with a positive COVID-19 test.
Findings of the survey in more detail are provided in Tables 2, 3, 4, 5 and Fig. 4.
Discussion
The most important finding of the present study was the massive cutback in primary as well as revision TJA service in Europe during the COVID-19 pandemic. Primary TJA was reported by only 5.9% of survey participants as still being carried out. 3.8% of the participants stated that they were still performing aseptic TJA revisions and 18.8% communicated that they were doing TJA reimplantation after previous removal of septic implants (2nd stage). In addition, postoperative follow-up visits and rehabilitation were also reported to be drastically impaired (Fig. 2).
These type of approach both by the health and hospital authorities and the orthopaedic surgeons has several undoubtable reasons: save resources for COVID-19 patients (medical and nurse staff, hospital beds, intensive care units, economical resources), to reduce the risks of contamination (of the staff, of the patients of the whole community) in an “open environment” such as the hospitals which are difficult to be controlled, to avoid contamination of fragile patients that are the majority of TJA patients especially in the post-operative time, to guarantee a safe and effective rehabilitation time.
When comparing our findings with those of other studies, it appears that the literature on that subject is scarce. Liebensteiner et al. questioned surgeons from Germany, Switzerland and Austria on a broad range of orthopaedic procedures [9]. Only 10% and 30% of their participants stated that they were still able to offer arthroscopic procedures, depending on the joint and procedure. Liebensteiner et al. found that 25% of the participating surgeons were still able to offer anterior cruciate ligament reconstructions, and 50% of the participants reported that rotator cuff repair was no longer being performed. Hardly any participants (< 1%) reported that even femoral fractures or sarcoma patients were postponed. In addition, similar to our findings, those authors reported drastic disruptions in postoperative follow-ups and rehabilitation facilities. In summary, the findings of that study are in good agreement with those of the current study.
Some publications reported similar scenarios in other surgical disciplines. Angelico et al. showed that major organ transplantation was reduced by 25% in recent weeks due to the lack of intensive care beds [2]. Our results also show that intensive care units as well as intermediate care units are the bottleneck during the COVID-19 pandemic (Table 5). Hence, one can assume that this consequently leads to a reduction in revision arthroplasty procedures, even when a patient has a massively failed TJA. Reduction of surgical volume was also reported for urology and colorectal surgeries [4, 10]. Our results show a massive reduction in outpatient activities. A similar scenario was shown for urology patients [4].
During the study period, the Coronavirus disease (COVID-19) pandemic was evolving rapidly in Europe, widely disrupting the personal, social, economic and professional life of healthcare workers. The overall goal of most governments in Europe was to “flatten the curve” of new COVID cases and to avoid a collapse of the national healthcare systems [1]. At the close of the survey, there were 840,246 confirmed COVID-19 cases in Europe with 70,583 fatalities [18]. Affected by the catastrophic consequences of the pandemic, orthopaedic healthcare was substantially cut back on the whole continent. This drastic disruption has had a massive impact on TJA, which is currently the international standard of care for surgical treatment of degenerative and rheumatologic joint diseases, as well as for certain fractures adjacent to the joint, like femoral neck fractures [7]. Postponing TJA in patients with high-stage osteoarthritis leads to more opioid use and poorer overall outcome regarding revision rate and readmission rate after TJA [12]. However, at least life-threatening pathologies such as periprosthetic fractures and first-stage revisions of acute infected TJA can still be treated appropriately even in the present difficult scenario.
More than 3.1 million total hip arthroplasties and 2.5 million total knee arthroplasties are performed every year in Europe [7, 11] to increase quality of life and improve the mobility of patients to enhance their life expectancy. Hence, the described cutback in arthroplasty services also has severe economic consequences for implant companies and their employees, as well as the families of the employees. TJA outcome is outstanding, and total hip arthroplasty has been named by several reports as “the operation of the century” [8]. In Europe, more than 24 national joint registries with over 40 years of experience are monitoring the life expectancy of implants and are responsible for quality assessment and management in TJA [11]. The beneficial impact of TJA regarding mobility, social life, work capability, prevention of cardiovascular diseases, general health, patient satisfaction, decreasing pain and increasing joint function, especially in elderly persons, but nowadays in young active people as well, is undisputed. Hence, if access to TJA is restricted, the direct and indirect costs to a nation’s society are enormous, because of early retirement, inability to work, direct costs to the healthcare systems caused by the immobility of people and indirect costs to the healthcare system, like employment status, earnings, time missed from work (or absenteeism), and disability payments [14]. There is no doubt that the COVID-19 outbreak in Europe influences our daily behaviour and prevention strategies [15]. As mentioned in our results, also most arthroplasty surgeons have contact with infected patients or infected hospital staff. Consequently, they change their attitude towards their families to prevent them from becoming infected with the disease. These lifestyle modifications range from affordable changes like washing and disinfecting the hands more often (87.1%) to significant changes like avoiding close physical contact with their families (22.1%), staying away from home (2.9%) or staying in a separate room at home (5.5%).
The study has some limitations. First, the expert opinion of the members of two societies was evaluated jointly in one study. However, both societies consist of predominantly arthroplasty experts and opinion leaders. Second, the respondents came from various countries that maintain different strategies toward the pandemic and that were at different levels of severity of the pandemic at the moment of the survey.
Conclusions
The 2020 COVID-19 pandemic has currently triggered a near-total shutdown of arthroplasty surgeries in Europe. A massive cutback was observed for primary TJA and revision TJA, even in massively failed TJA with collapse, dislocation, component failure or imminent dislocation. Out of trauma cases and malignancy, only life-threatening pathologies like periprosthetic fractures and acute septic TJA are currently being treated surgically.
Change history
30 October 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00167-023-07636-0
References
Akiyama MJ, Spaulding AC, Rich JD (2020) Flattening the curve for incarcerated populations—Covid-19 in jails and prisons. N Engl J Med. https://doi.org/10.1056/NEJMp2005687
Angelico R, Trapani S, Manzia TM, Lombardini L, Tisone G, Cardillo M (2020) The COVID-19 outbreak in Italy: initial implications for organ transplantation programs. Am J Transplant. https://doi.org/10.1111/ajt.15904
Chang Liang Z, Wang W, Murphy D, Po Hui JH (2020) Novel coronavirus and orthopaedic surgery: early experiences from Singapore. J Bone Jt Surg Am. https://doi.org/10.2106/JBJS.20.00236
Connor MJ, Winkler M, Miah S (2020) COVID-19 Pandemic—is virtual urology clinic the answer to keeping the cancer pathway moving? BJU Int . https://doi.org/10.1111/bju.15061
D’Apolito R, Faraldi M, Ottaiano I, Zagra L (2020) Disruption of Arthroplasty practice in an orthopaedic center in northern Italy during COVID-19 pandemic. J Arthoplasty. https://doi.org/10.1016/j.arth.2020.04.057
Gurría A (2020) Secretary General Angel Gurría’s statement for the G20 videoconference summit on COVID-19. https://read.oecd-ilibrary.org/view/?ref=126_126445-5ofyod1xpv&title=SecretaryGeneralAngelGurriaStatementforthe20_VideoconferenceSummitonCOVID19. Accessed 20 Apr 2
Kurtz SM, Ong KL, Lau E, Widmer M, Maravic M, Gómez-Barrena E, de Pina M, Manno V, Torre M, Walter WL, de Steiger R, Geesink RGT, Peltola M, Röder C (2011) International survey of primary and revision total knee replacement. Int Orthop 35:1783–1789
Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: total hip replacement. Lancet (London) 370:1508–1519
Liebensteiner MC, Khosravi I, Hirschmann MT, Heuberer PR, Thaler M (2020) Massive cutback in orthopaedic healthcare services due to the COVID-19 pandemic: an online survey of almost 1400 orthopaedic surgeons in Austria, Germany and Switzerland. Knee Surg Sport Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06032-2
Lisi G, Campanelli M, Spoletini D, Carlini M (2020) The possible impact of COVID-19 on colorectal surgery in Italy. Color Dis 12:13. https://doi.org/10.1111/codi.15054
Lübbeke A, Silman AJ, Barea C, Prieto-Alhambra D, Carr AJ (2018) Mapping existing hip and knee replacement registries in Europe. Health Policy 122:548–557
Malik AT, Alexander JH, Li DD, Li M, Khan SN, Scharschmidt TJ (2020) What are the costs of hip osteoarthritis in the year prior to a total hip arthroplasty? J Arthroplasty 35:313–317.e1
Mao R, Liang J, Shen J, Ghosh S, Zhu L-R, Yang H, Wu K-C, Chen M-H (2020) Implications of COVID-19 for patients with pre-existing digestive diseases. Lancet Gastroenterol Hepatol 5:426–428
Ruiz DJ, Koenig L, Dall TM, Gallo P, Narzikul A, Parvizi J, Tongue J (2013) The direct and indirect costs to society of treatment for end-stage knee osteoarthritis. J Bone Jt Surg Am 95:1473–1480
Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A (2020) The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. https://doi.org/10.1177/0020764020915212
Tsai J, Wilson M (2020) COVID-19: a potential public health problem for homeless populations. Lancet Public Health 5:e186–e187
Vannabouathong C, Devji T, Ekhtiari S, Chang Y, Phillips SA, Zhu M, Chagla Z, Main C, Bhandari M (2020) Novel Coronavirus COVID-19: current evidence and evolving strategies. J Bone Jt Surg Am. https://doi.org/10.2106/JBJS.20.00396
WHO (2020) WHO Coronavirus 2019 Situation Report-82. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Accessed 11 Apr 2020
Xue Y, Kristiansen IS, de Blasio BF (2012) Dynamic modelling of costs and health consequences of school closure during an influenza pandemic. BMC Public Health 12:962. https://doi.org/10.1186/1471-2458-12-962
Funding
None.
Author information
Authors and Affiliations
Contributions
MT was responsible for data collection and manuscript writing. IK wrote the survey, helped during writing of the manuscript by providing results, figures and table. MTH performed a revision of the manuscript. MCL, NPK, JAE and LZ were responsible for the data collection and also reviewing the manuscript. MT provided the concept of the study and developed the survey. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
None (no patient data involved).
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thaler, M., Khosravi, I., Hirschmann, M.T. et al. Disruption of joint arthroplasty services in Europe during the COVID-19 pandemic: an online survey within the European Hip Society (EHS) and the European Knee Associates (EKA). Knee Surg Sports Traumatol Arthrosc 28, 1712–1719 (2020). https://doi.org/10.1007/s00167-020-06033-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06033-1