Abstract
Purpose
To examine the role of the posterior fan-like extension of the ACL’s femoral footprint on the ACL failure load.
Methods
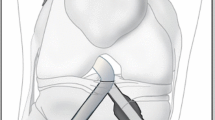
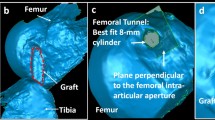
Sixteen (n = 16) fresh frozen, mature porcine knees were used in this study and randomized into two groups (n = 8): intact femoral ACL insertion (ACL intact group) and cut posterior fan-like extension of the ACL (ACL cut group). In the ACL cut group, flexing the knees to 90°, created a folded border between the posterior fan-like extension and the midsubstance insertion of the femoral ACL footprint and the posterior fan-like extension was dissected and both areas were measured. Specimens were placed in a testing machine at 30° of flexion and subjected to anterior tibial loading (60 mm/min) until ACL failure.
Results
The intact ACL group had a femoral insertion area of 182.1 ± 17.1 mm2. In the ACL cut group, the midsubstance insertion area was 113.3 ± 16.6 mm2, and the cut posterior fan-like extension portion area was 67.1 ± 8.3 mm2. The failure load of the ACL intact group was 3599 ± 457 N and was significantly higher (p < 0.001) than the failure load of the ACL cut group 392 ± 83 N.
Conclusion
Transection of the posterior fan-like extension of the ACL femoral footprint has a significant effect on the failure load of the ligament during anterior loading at full extension. Regarding clinical relevance, this study suggests the importance of the posterior fan-like extension of the ACL footprint which potentially may be retained with remnant preservation during ACL reconstruction. Femoral insertion remnant preservation may allow incorporation of the fan-like structure into the graft increasing graft strength.





Similar content being viewed by others
References
Araki D, Thorhauer E, Tashman S (2018) Three-dimensional isotropic magnetic resonance imaging can provide a reliable estimate of the native anterior cruciate ligament insertion site anatomy. Knee Surg Sports Traumatol Arthrosc 26:1311–1318
Araujo PH, Asai S, Pinto M, Protta T, Middleton K, Linde-Rosen M, Irrgang J, Smolinski P, Fu FH (2015) ACL graft position affects in situ graft force following ACL reconstruction. J Bone Jt Surg Am 97:1767–1773
Fujimaki Y, Thorhauer E, Sasaki Y, Smolinski P, Tashman S, Fu FH (2016) Quantitative in situ analysis of the anterior cruciate ligament: length, midsubstance cross-sectional area, and insertion site areas. Am J Sports Med 44:118–125
Gan Y, Xu D, Ding J, Xu Y (2012) Tension band wire fixation for anterior cruciate ligament avulsion fracture: biomechanical comparison of four fixation techniques. Knee Surg Sports Traumatol Arthrosc 20:909–915
Hara K, Mochizuki T, Sekiya I, Yamaguchi K, Akita K, Muneta T (2009) Anatomy of normal human anterior cruciate ligament attachments evaluated by divided small bundles. Am J Sports Med 37:2386–2391
Harner CD, Livesay GA, Kashiwaguchi S, Fujie H, Choi NY, Woo SL (1995) Comparative study of the size and shape of human anterior and posterior cruciate ligaments. J Orthop Res 13:429–434
Kawaguchi Y, Kondo E, Takeda R, Akita K, Yasuda K, Amis AA (2015) The role of fibers in the femoral attachment of the anterior cruciate ligament in resisting tibial displacement. Arthroscopy 31:435–444
Li F, Qin L, Gong X, Huang Z, Wang T, Liu Z, Sandiford S, Yang J, Zhu S, Liang X, Huang W, Hu N (2019) The Chinese ACL injury population has a higher proportion of small ACL tibial insertion sizes than Western patients. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05541-z
Markolf KL, Hame S, Hunter DM, Oakes DA, Zoric B, Gause P, Finerman GA (2002) Effects of femoral tunnel placement on knee laxity and forces in an anterior cruciate ligament graft. J Orthop Res 20:1016–1024
Mochizuki T, Fujishiro H, Nimura A, Mahakkanukrauh P, Yasuda K, Muneta T, Akita K (2014) Anatomic and histologic analysis of the mid-substance and fan-like extension fibres of the anterior cruciate ligament during knee motion, with special reference to the femoral attachment. Knee Surg Sports Traumatol Arthrosc 22:336–344
Moon DK, Woo SL, Takakura Y, Gabriel MT, Abramowitch SD (2006) The effects of refreezing on the viscoelastic and tensile properties of ligaments. J Biomech 39:1153–1157
Nawabi DH, Tucker S, Schafer KA, Zuiderbaan HA, Nguyen JT, Wickiewicz TL, Imhauser CW, Pearle AD (2016) ACL fibers near the lateral intercondylar ridge are the most load bearing during stability examinations and isometric through passive flexion. Am J Sports Med 44:2563–2571
Rahnemai-Azar AA, Sabzevari S, Irarrázaval S, Chao T, Fu F (2016) Anatomical individualized ACL reconstruction. ABJS 4:291–297
Sasaki N, Ishibashi Y, Tsuda E, Yamamoto Y, Maeda S, Mizukami H, Toh S, Yagihashi S, Tonosaki Y (2012) The femoral insertion of the anterior cruciate ligament: discrepancy between macroscopic and histological observations. Arthroscopy 28:1135–1146
Smigielski R, Zdanowicz U, Drwiega M, Ciszek B, Ciszkowska-Lyson B, Siebold R (2015) Ribbon like appearance of the midsubstance fibres of the anterior cruciate ligament close to its femoral insertion site: a cadaveric study including 111 knees. Knee Surg Sports Traumatol Arthrosc 23:3143–3150
van Eck CF, Lesniak BP, Schreiber VM, Fu FH (2010) Anatomic single- and double-bundle anterior cruciate ligament reconstruction flowchart. Arthroscopy 26:258–268
Woo SL, Hollis JM, Adams DJ, Lyon RM, Takai S (1991) Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am J Sports Med 19:217–225
Woo SL, Orlando CA, Camp JF, Akeson WH (1986) Effects of postmortem storage by freezing on ligament tensile behavior. J Biomech 19:399–404
Xerogeanes JW, Fox RJ, Takeda Y, Kim HS, Ishibashi Y, Carlin GJ, Woo SL (1998) A functional comparison of animal anterior cruciate ligament models to the human anterior cruciate ligament. Ann Biomed Eng 26:345–352
Funding
This study was funded by the Department of Orthopaedic Surgery at the University of Pittsburgh.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflicts to disclose.
Ethical approval
No ethical approval was required from IACUC.
Informed consent
Not applicable to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sabzevari, S., Shaikh, H., Marshall, B. et al. The femoral posterior fan-like extension of the ACL insertion increases the failure load. Knee Surg Sports Traumatol Arthrosc 28, 1113–1118 (2020). https://doi.org/10.1007/s00167-019-05753-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05753-3