Abstract
Purpose
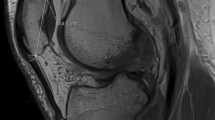
An increased lateral quadriceps vector has been associated with lateral patellar dislocation. Surgical correction of this increased vector through tibial tubercle medialization is often recommended when the quadriceps vector is “excessive”. This can be evaluated by physical examination measurements of Q-angle and/or tubercle sulcus angle (TSA), as well as the magnetic resonance imaging (MRI) measurement of tibial tubercle–trochlear groove (TT–TG) distance. This study examined the relationship between three objective measurements of lateral quadriceps vector (TT–TG, Q-angle, TSA). A secondary goal was to relate lateral patellar tilt to these measurements.
Methods
Consecutive patients undergoing patellofemoral stabilization surgery from 9/2010 to 6/2011 were included. The Q-angle and TSA were measured on intra-operative physical examination. The TT–TG and patellar tilt were measured on MRI. TSA, Q-angle, and patellar tilt were compared to TT–TG using Pearson correlation coefficient.
Results
The study cohort included 49 patients, ages 12–37 (mean 23.2); 62% female. The Pearson correlation coefficients showed (+) significance (p < 0.01) between the TT–TG and both TSA and Q-angle. Tilt and TT–TG were (+) non-significantly correlated. Despite positive correlations of each measurement with TT–TG, there is not uniform intra-patient correlation. In other words, if TT–TG is elevated for a patient, it does not guarantee that all other measurements, including tilt, are elevated in that individual patient.
Conclusion
The TT–TG distance has significant positive correlation with the measurements of TSA and Q-angle in patients undergoing surgery for patellofemoral instability. The clinical relevance is that the variability within individual patients demonstrates the need for considering both TSA and TT–TG before and during surgical intervention to avoid overcorrection with a medial tibial tubercle osteotomy.
Level of evidence
Diagnostic study, Level III.








Similar content being viewed by others
References
Apostolovic M, Vukomanovic B, Slavkovic N, Vuckovic V, Vukcevic M, Djuricic G, Kocev N (2011) Acute patellar dislocation in adolescents: operative versus nonoperative treatment. Int Orthop 35(10):1483–1487
Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C (2000) Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med 28(4):472–479
Biyani R, Elias JJ, Saranathan A, Feng H, Guseila LM, Morscher MA, Jones KC (2014) Anatomical factors influencing patellar tracking in the unstable patellofemoral joint. Knee Surg Sports Traumatol Arthrosc 22(10):2334–2341
Brattström H (1964) Shape of the intercondylar groove normally and in recurrent dislocation of patella. A clinical and X-ray-anatomical investigation. Acta Orthop Scand Suppl 68:1–148
Brown DE, Alexander AH, Lichtman DM (1984) The Elmslie-Trillat procedure: evaluation in patellar dislocation and subluxation. Am J Sports Med 12(2):104–109
Calmbach WL, Hutchens M (2003) Evaluation of patients presenting with knee pain: part II. Differential diagnosis. Am Fam Physician 68(5):917–922
Caylor D, Fites R, Worrell TW (1993) The relationship between quadriceps angle and anterior knee pain syndrome. J Orthop Sports Phys Ther 17(1):11–16
Cooney AD, Kazi Z, Caplan N, Newby M, St Clair Gibson A, Kader DF (2012) The relationship between quadriceps angle and tibial tuberosity-trochlear groove distance in patients with patellar instability. Knee Surg Sports Traumatol Arthrosc 20(12):2399–2404
Cox JS (1976) An evaluation of the Elmslie-Trillat procedure for management of patellar dislocations and subluxations: a preliminary report. Am J Sports Med 4(2):72–77
Daynes J, Hinckel BB, Farr J (2016) Tibial tuberosity-posterior cruciate ligament distance. J Knee Surg 29(6):471–477
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2(1):19–26
Dickschas J, Harrer J, Bayer T, Schwitulla J, Strecker W (2016) Correlation of the tibial tuberosity-trochlear groove distance with the Q-angle. Knee Surg Sports Traumatol Arthrosc 24(3):915–920
Freedman BR, Brindle TJ, Sheehan FT (2014) Re-evaluating the functional implications of the Q-angle and its relationship to in vivo patellofemoral kinematics. Clin Biomech (Bristol, Avon) 29(10):1139–1145
Goldthwait JE (1899) Permanent dislocation of the patella. The report of a case of twenty years’ duration, successfully treated by transplantation of the patella tendons with the tubercle of the tibia. Ann Surg 29(1):62–68
Guilbert S, Chassaing V, Radier C, Hulet C, Remy F, Chouteau J, Chotel F, Boisrenoult P, Sebilo A, Ferrua P, Ehkirch FP, Bertin D, Dejour D, French Arthroscopy Society (2013) Axial MRI index of patellar engagement: a new method to assess patellar instability. Orthop Traumatol Surg Res 99(8 Suppl):S399–S405
Herrington L, Nester C (2004) Q-angle undervalued? The relationship between Q-angle and medio-lateral position of the patella. Clin Biomech (Bristol, Avon) 19(10):1070–1073
Huberti HH, Hayes WC (1984) Patellofemoral contact pressures. The influence of Q-angle and tendofemoral contact. J Bone Joint Surg Am 66(5):715–724
Izadpanah K, Weitzel E, Vicari M, Hennig J, Weigel M, Sudkamp NP, Niemeyer P (2014) Influence of knee flexion angle and weight bearing on the tibial tuberosity-trochlear groove (TTTG) distance for evaluation of patellofemoral alignment. Knee Surg Sports Traumatol Arthrosc 22(11):2655–2661
Kirsch MD, Fitzgerald SW, Friedman H, Rogers LF (1993) Transient lateral patellar dislocation: diagnosis with MR imaging. AJR Am J Roentgenol 161(1):109–113
Kolowich PA, Paulos LE, Rosenberg TD, Farnsworth S (1990) Lateral release of the patella: indications and contraindications. Am J Sports Med 18(4):359–365
Lee C-H, Wu C-C, Pan R-Y, Lu H-T, Shen H-C (2014) Medial retinacular flap advancement and arthroscopic lateral release for symptomatic chronic patellar lateral subluxation with tilting. Knee Surg Sports Traumatol Arthrosc 22(10):2499–2504
Livingston LA (1998) The quadriceps angle: a review of the literature. J Orthop Sports Phys Ther 28(2):105–109
Merchant AC (2011) A philosophy of the patellofemoral joint: a logical clinical approach. In: Sanchis-Alfonso V (ed) Anterior knee pain and patellar instability, 2nd edn. Springer-Verlag, London, pp 519–530
Merchant AC, Mercer RL (1974) Lateral release of the patella. A preliminary report. Clin Orthop Relat Res 103:40–45
Miyazaki Y, Nakamura T, Kogame K, Saito M, Yamamoto K, Suguro T (2011) Analysis of the kinematics of total knee prostheses with a medial pivot design. J Arthroplasty 26(7):1038–1044
Nietosvaara Y, Aalto K, Kallio PE (1994) Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 14(4):513–515
Roux C (1888) Luxation habituelle de la rotule. Traitement opératoire/[Recurrent dislocation of the patella. Operative treatment]. Rev Chir 8:682–689
Sanchez HM, Sanchez EGdM, Barauna MA, Canto RSdT (2014) Evaluation of Q angle in differents static postures. Acta Ortop Bras 22(6):325–329
Sanfridsson J, Arnbjornsson A, Friden T, Ryd L, Svahn G, Jonsson K (2001) Femorotibial rotation and the Q-angle related to the dislocating patella. Acta Radiol 42(2):218–224
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CWA, Fucentese SF, Romero J (2006) The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13(1):26–31
Smith TO, Hunt NJ, Donell ST (2008) The reliability and validity of the Q-angle: a systematic review. Knee Surg Sports Traumatol Arthrosc 16(12):1068–1079
Stefancin JJ, Parker RD (2007) First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res 455:93–101
Tanaka MJ, Elias JJ, Williams AA, Carrino JA, Cosgarea AJ (2015) Correlation between changes in tibial tuberosity-trochlear groove distance and patellar position during active knee extension on dynamic kinematic computed tomographic imaging. Arthroscopy 31(9):1748–1755
Tensho K, Akaoka Y, Shimodaira H, Takanashi S, Ikegami S, Kato H, Saito N (2015) What components comprise the measurement of the tibial tuberosity-trochlear groove distance in a patellar dislocation population? J Bone Joint Surg Am 97(17):1441–1448
Trillat A, Dejour H, Couette A (1964) Diagnosis and treatment of recurrent dislocations of the patella. Rev Chir Orthop Reparatrice Appar Mot 50:813–824
Wilson T, Kitsell F (2002) Is the Q-angle an absolute or a variable measure?: Measurement of the Q-angle over one minute in healthy subjects. Physiotherapy 88(5):296–302
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Sources of funding
This study has no sources of funding.
Ethical approval
Institutional Review Board (IRB) approval was obtained from the University of Minnesota IRB (Study Number 0307M50363) prior to initiation of this study.
Informed consent
All ethical standards and requirements for maintaining patient, data, and study integrity have been employed, including those in accordance with the 1964 Declaration of Helsinki and the U.S. Health Insurance Portability and Accountability Act (HIPAA).
Rights and permissions
About this article
Cite this article
Graf, K.H., Tompkins, M.A., Agel, J. et al. Q-vector measurements: physical examination versus magnetic resonance imaging measurements and their relationship with tibial tubercle–trochlear groove distance. Knee Surg Sports Traumatol Arthrosc 26, 697–704 (2018). https://doi.org/10.1007/s00167-017-4527-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4527-5