Abstract
Contact isolation of infected or colonised hospitalised patients is instrumental to interrupting multidrug-resistant organism (MDRO) cross-transmission. Many studies suggest an increased rate of adverse events associated with isolation. We aimed to compare isolated to non-isolated patients in intensive care units (ICUs) for the occurrence of adverse events and medical errors.
Methods
We used the large database of the Iatroref III study that included consecutive patients from three ICUs to compare the occurrence of pre-defined medical errors and adverse events among isolated vs. non-isolated patients. A subdistribution hazard regression model with careful adjustment on confounding factors was used to assess the effect of patient isolation on the occurrence of medical errors and adverse events.
Results
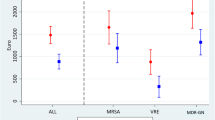
Two centres of the Iatroref III study were eligible, an 18-bed and a 10-bed ICU (nurse-to-bed ratio 2.8 and 2.5, respectively), with a total of 1,221 patients. After exclusion of the neutropenic and graft transplant patients, a total of 170 isolated patients were compared to 980 non-isolated patients. Errors in insulin administration and anticoagulant prescription were more frequent in isolated patients. Adverse events such as hypo- or hyperglycaemia, thromboembolic events, haemorrhage, and MDRO ventilator-associated pneumonia (VAP) were also more frequent with isolation. After careful adjustment of confounders, errors in anticoagulant prescription [subdistribution hazard ratio (sHR) = 1.7, p = 0.04], hypoglycaemia (sHR = 1.5, p = 0.01), hyperglycaemia (sHR = 1.5, p = 0.004), and MDRO VAP (sHR = 2.1, p = 0.001) remain more frequent in isolated patients.
Conclusion
Contact isolation of ICU patients is associated with an increased rate of some medical errors and adverse events, including non-infectious ones.
Similar content being viewed by others
Introduction
Antimicrobial resistance has reached such endemic levels that infection control programmes are now mandatory procedures in many centres. Means to prevent the spread of multidrug-resistant organisms (MDROs) have included the development of antimicrobial stewardship programmes, the promotion of hand hygiene and its improvement, the screening of patients at admission, and the use of strict barrier and isolation precautions. A number of infection control societies recommend mandatorily setting up and respecting standard and contact precautions for preventing the transmission of MDROs such as methicillin-resistant Staphylococcus aureus (MRSA), vancomycin–resistant Enterococcus (VRE), and some gram-negative bacilli (GNB) [1–3]. However, although recommended and widely used in healthcare institutions to prevent transmission of MDROs, contact isolation measures and their global impact remain debated [4–7].
Recently, in a cluster-randomised trial conducted in the intensive care unit (ICU), some authors suggested that surveillance for MRSA and VRE colonisation as well as the expanded use of barrier precautions was not effective in reducing the transmission of these two MDROs [8]. Moreover, contact isolation in hospital wards has been associated with decreased patient-healthcare worker contact [9], an increased rate of depression and anxiety symptoms, decreased patient satisfaction with care [10], and a higher number of adverse events in patients on contact isolation [11].
So far, the global evaluation of the risk-benefit balance of the isolation of ICU patients remains controversial. During the Iatroref III study, we carefully monitored selected medication errors, adverse events and nosocomial infections. This study included two ICUs from the Iatroref III study where MDRO-related contact isolation of non-neutropenic, not graft-recipient patients was routinely performed on an individual patient basis and prospectively monitored.
Therefore, the purpose of this post hoc analysis is to assess the impact of isolation on the rate of medication errors and adverse events using the Iatroref III study data set.
Methods
This study was approved by the institutional review board of the Rhône-Alpes-Auvergne Clinical Investigation Centres, which waived the requirement for written informed consent. Patients eligible for the study are all patients from two centres extracted from the Iatroref III study [12, 13]. The Iatroref III study is a multicentre cluster-randomised study in consecutive patients older than 18 years, aiming to test the effects of three multifaceted safety programmes (MFSP). These programmes were designed to decrease insulin administration errors, anticoagulant prescription and administration errors, and errors leading to accidental removal of endotracheal tubes and central venous catheters, respectively. The Iatroref III study included all consecutive patients admitted during four predefined periods from January 2007 to January 2008 in three ICUs belonging to the Outcome Rea Study Group. The two centres that were eligible for the isolation study were those where patients were isolated for MDRO. Isolation was initiated when patients were suspected of or identified as carrying an MDRO or as being infected with one. One centre is within a university teaching hospital; the other is within a general hospital. Within this subset, patients were excluded if they had protective isolation for neutropenia or recent solid organ transplantation.
Patient characteristics were collected on Rhea ™ software (http://outcomerea.org/rhea/install), and medical error characteristics were entered in an add-on specifically designed for the study. The following data were collected: age, sex, the underlying diseases using the Knaus classification [14] admission category (medical, scheduled surgery, or unscheduled surgery), and the reason for ICU admission (with nine categories prospectively defined before the study, namely, respiratory, cardiac, or renal failure; coma, multiple organ failure, acute exacerbation of chronic pulmonary disease, monitoring, trauma, and scheduled surgery). The location of the patient prior to ICU admission was recorded, with transfer from wards defined as being within the same hospital or from another hospital. The Simplified Acute Physiology Score (SAPS II) [15] at admission and the Sequential Organ Failure Assessment (SOFA) score [16] were computed using the worst physical and laboratory data during the first 24 h in the ICU. The date and reason for contact isolation initiation were recorded. Patients who were MDRO carriers were isolated until the day of ICU discharge. Invasive procedures and medications (anticoagulants, vasopressor support, blood products, insulin, sedatives) used during the entire stay were listed. Lengths of stay in the ICU and acute-care hospital were recorded, as well as vital status at ICU and hospital discharge.
Specific incidences of adverse events were calculated as the ratio of the number of events on the number of days of ICU care where the patient was exposed to the risk of the specific event.
Medical errors targeted by the study
Medical errors were defined according to the Iatroref III study [13]; the three target safety indicators and their possible harm have been defined elsewhere [12]. The following events were prospectively recorded: accidental removal of a central venous catheter (Fig. 1) or accidental extubation [17, 18], hypernatremia >150 mmol/l [19], ventilator-associated pneumonia (VAP) [20] occurrence, error in insulin administration, error in anticoagulant administration, error in anticoagulant prescription, adverse events related to medication errors such as phlebitis, pulmonary embolism, haemorrhage requiring red blood cell transfusion, and hypo- and hyperglycaemia (Table 1).
Statistical analysis
Patients’ characteristics were described using the frequency and percentage of qualitative variables, and the mean and standard deviation (or median and quartiles) for quantitative ones.
Differences in specific incidence rates of adverse events/medical errors between the pre-isolation period and isolation period were tested using the Poisson regression model with the Pearson scale and robust sandwich variance to include intra-patient correlation.
We used subdistribution hazard models to account for discharge alive from the ICU as a competing event to experiencing medical errors or adverse event in the ICU [21]. This modelling took into account the indirect effect on mortality of a (potentially) extended stay due to the exposure. Isolation was treated as time-dependent exposition, changing from non-isolated to isolated status at the time of isolation. For each medical error or adverse event, models were adjusted for other clinically relevant confounders.
Models were applied to the entire cohort except for a few endpoints: for accidental removal of the endotracheal tube or catheter, analysis was restricted to intubated patient or patients with a central venous catheter at least once during the ICU stay. Errors on administering anticoagulant were restricted to patients with anticoagulants, ventilator-associated nosocomial pneumonia cases were restricted to ventilated patients, and errors in insulin administration were restricted to patients receiving insulin.
Every model was stratified by ICU centre. No correction for multiple testing was applied. The full statistical analysis was performed using SAS version 9.3, and models were fitted using PROC PHREG.
Results
A total of 1,221 patients were included in the two centres eligible for MDRO isolation study. The two centres were respectively an 18-bed medical ICU and a 10-bed medical/surgical ICU. The targeted nurse-to-bed ratios were 2.8 and 2.5 for both ICUs, but we did not collect daily nurse-to-bed ratio variability because of absenteeism of closed beds. Patients who were neutropenic or had had a graft transplant were excluded (171 patients, 5.8 %). Therefore, 1,150 (54 %) patients were eligible for the MDRO isolation study (Table 2). Among these patients, 170 (14.8 %) were isolated for MDRO carriage or infection during their ICU stay, whereas 980 (85.2 %) were not. The mean age of the study population was 62 years (±17 years), and the average SAPS was 43 (±21). Isolated patients were more often diagnosed for acute respiratory failure shock or multiorgan failure at admission than non-isolated patients. In the first 24 h following admission, they were more frequently treated with catecholamine and insulin and more frequently had central venous and arterial catheters.
Of the 170 isolated patients, 75 (44.1 %) had adverse events before isolation and 140 (82.4 %) during the isolation period.
Rates of medication errors or adverse events per patient are depicted in Table 3.
Specific incidences of adverse events associated with transfusion or VAP due to MDRO (Table 3) were higher during days under isolation compared to non-isolation days.
When we considered VAP, the specific incidence in non-isolated patients was 35.6 per thousand mechanical ventilation days, whereas, for isolated patients, the incidence was 72.1 per thousand before isolation and 65.9 per thousand under isolation. Interestingly, the increase in the incidence of VAP due to MDRO was the sole contributor to the increase in VAP incidence observed under isolation (Table 3).
The time-adjusted hazard ratio of errors in anticoagulant therapy prescription, in insulin administration, and of adverse events (hypo-, hyperglycaemia, haemorrhage, thromboembolic events) increased during isolation days. After adjustment of other risk factors, isolation remained associated with errors in anticoagulant prescription, hypo- and hyperglycaemia, and VAP due to MDRO (Table 4). Very similar results were obtained when comparing patients isolated on admission and patients not isolated. There was no significant difference in the effect of isolation on the occurrence of adverse events between the two centres.
Discussion
In this study, our purpose was to assess the frequency of adverse events according to the isolation status in an ICU cohort population. Medication errors and adverse events were prospectively collected by trained dedicated personnel on a large cohort of patients. After careful adjustment for confounding variables and use of appropriate time-adjusted models, hypoglycaemia, hyperglycaemia, error in anticoagulant prescription, and VAP due to MDRO were the five medication errors or adverse events observed significantly more often in isolated patients.
The presence of errors that could be avoided without having to examine the patient (e.g., insulin ordering depends on review of medical records and not on direct evaluation of the patient) could be considered surprising. Indeed, in the two ICUs, medical records were only available as paper charts located into the patient’s room. Switching to electronic medical records available outside the room could be a potential benefit for reducing the occurrence of adverse events and needs to be further evaluated.
The risk-benefit ratio of isolation in the ICU is debated. Whereas a number of studies have suggested that isolation reduces the spread of multiresistant bacteria [7, 22], other studies have underlined the weakness of and potential bias associated with before-after studies [4, 23] that combine isolation with other interventions [24]. Several studies have reported significantly better control using surveillance cultures and contact precautions in the ICU [1, 7, 25].
Several studies [10, 11, 26, 27] performed in hospital wards outside of ICUs suggested that the use of isolation may cause patients to receive less medical attention and less healthcare worker-to-patient contact; may result in more frequent medical errors and adverse events, in delay of medical progress, and delay of discharge; and is associated with psychological stress and anxiety, and with decreased patient satisfaction with care [28].
Adverse events in patients under contact precaution (CP) have been evaluated in an historical-matched cohort reviewing charts for 150 patients under CP and 300 controls not under CP at two hospitals in North America. Two matched cohorts were retrospectively created with patients issued from general medicine or patients with congestive heart failure and adjusted on the CP exposure duration. This study showed that CP was associated with a decrease in vital sign recording and a decrease in medical and nurse daily recording of narrative notes. Isolation was also associated with a more than six-fold increase in the occurrence of preventable adverse events and with an eight-fold increase in supportive care failure (falls, pressure ulcers, fluid or electrolyte disorders) [11].
All these different studies have a number of limitations such as the limited number of patients included [27, 29], no or limited adjustment for the number of confounding factors, and an unclear total number of isolated patients. More importantly, it has never been tested in an ICU setting where a nurse-to-patient ratio of 1:2 is considered sufficient [11, 26]. Our results suggest that the association between isolation and non-infectious medical errors or adverse events exists also in the ICU setting.
In a recent study [30], the authors underline a decrease in the incidence of VAP in their ICU after implementing eight target recommendations, with most of them requiring close monitoring of the patient. In our study, after careful adjustment of the risk factors of VAP, isolation remained a risk factor solely for those VAPs due to MDRO. The increase in the cumulative incidence of VAP due to MDRO could either be due to a failure to maintain an appropriate strategy for prevention or be related to the MDRO carriage. Indeed, the increase in resistance of endogenous flora associated with MDRO carriage adds to the total burden of VAP [31] and likely explains the overall increase in the VAP rate.
Study limitations
The association shown between isolation measures and the increase in the risk of some medication errors and of some adverse events might have been related to the absence of control of other confounders that may influence the risk of events. We made a particular effort to adjust for potential confounders at ICU admission, but we cannot be sure that all confounders present at ICU admission or occurring between ICU admission and isolation have been taken into account.
The crude incidence of adverse events was paradoxically higher before that during isolation in isolated patients. This finding is explained by the fact that the daily number of adverse events in all patients (isolated and non-isolated) in the original IATROREF III study decreased with time during the ICU stay [12].
Another limitation is that our study was not designed to capture data related to the number of visits of healthcare staff to monitor and check the patient, the level of medical and nurse recording, or the patient’s feelings about the isolation. We selected events previously demonstrated to be easy to measure and well defined. It still needs to be established that the selected adverse events are an appropriate surrogate of an increase in the overall rate of adverse events. Finally, although in our study we underlined an association between isolation and adverse events, it is unclear whether the observed results are markers of the severity of patient illness or are a direct consequence of isolation. However, we tried to adjust and take into account the numerous confounding variables as optimally as possible in order to draw the most realistic conclusions.
Conclusions
In this large study conducted in ICUs, isolation in the ICU was significantly associated with more medication errors and more adverse events. With regards to efficacy and therefore ethics, contact isolation measures for limiting the spread of MDRO should be limited and designed according to the individual risk and collective benefit to ensure the benefits outweigh the risks.
References
Muto CA, Jernigan JA, Ostrowsky BE, Richet HM, Jarvis WR, Boyce JM, Farr BM (2003) SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus. Infect Control Hosp Epidemiol 24:362–386
Siegel JD, Rhinehart E, Jackson M, Chiarello L (2007) 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control 35:S65–S164
Siegel JD, Rhinehart E, Jackson M, Chiarello L (2007) Management of multidrug-resistant organisms in health care settings, 2006. Am J Infect Control 35:S165–S193
Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, Duckworth G, Lai R, Ebrahim S (2004) Isolation measures in the hospital management of methicillin resistant Staphylococcus aureus (MRSA): systematic review of the literature. BMJ 329:533
Cepeda JA, Whitehouse T, Cooper B, Hails J, Jones K, Kwaku F, Taylor L, Hayman S, Cookson B, Shaw S, Kibbler C, Singer M, Bellingan G, Wilson AP (2005) Isolation of patients in single rooms or cohorts to reduce spread of MRSA in intensive-care units: prospective two-centre study. Lancet 365:295–304
Raineri E, Crema L, De Silvestri A, Acquarolo A, Albertario F, Carnevale G, Latronico N, Petrosillo N, Tinelli C, Zoncada A, Pan A (2007) Meticillin-resistant Staphylococcus aureus control in an intensive care unit: a 10 year analysis. J Hosp Infect 67:308–315
Lucet JC, Paoletti X, Lolom I, Paugam-Burtz C, Trouillet JL, Timsit JF, Deblangy C, Andremont A, Regnier B (2005) Successful long-term program for controlling methicillin-resistant Staphylococcus aureus in intensive care units. Intensive Care Med 31:1051–1057
Huskins WC, Huckabee CM, O’Grady NP, Murray P, Kopetskie H, Zimmer L, Walker ME, Sinkowitz-Cochran RL, Jernigan JA, Samore M, Wallace D, Goldmann DA (2011) Intervention to reduce transmission of resistant bacteria in intensive care. N Engl J Med 364:1407–1418
Evans HL, Shaffer MM, Hughes MG, Smith RL, Chong TW, Raymond DP, Pelletier SJ, Pruett TL, Sawyer RG (2003) Contact isolation in surgical patients: a barrier to care? Surgery 134:180–188
Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN (2009) Adverse outcomes associated with contact precautions: a review of the literature. Am J Infect Control 37:85–93
Stelfox HT, Bates DW, Redelmeier DA (2003) Safety of patients isolated for infection control. JAMA 290:1899–1905
Garrouste-Orgeas M, Timsit JF, Vesin A, Schwebel C, Arnodo P, Lefrant JY, Souweine B, Tabah A, Charpentier J, Gontier O, Fieux F, Mourvillier B, Troche G, Reignier J, Dumay MF, Azoulay E, Reignier B, Carlet J, Soufir L (2010) Selected medical errors in the intensive care unit: results of the IATROREF study: parts I and II. Am J Respir Crit Care Med 181:134–142
Garrouste-Orgeas M, Soufir L, Tabah A, Schwebel C, Vesin A, Adrie C, Thuong M, Timsit JF (2012) A multifaceted program for improving quality of care in intensive care units: iatroref study. Crit Care Med 40:468–476
Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE (1981) APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med 9:591–597
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Timsit JF, Fosse JP, Troche G, De Lassence A, Alberti C, Garrouste-Orgeas M, Bornstain C, Adrie C, Cheval C, Chevret S (2002) Calibration and discrimination by daily logistic organ dysfunction scoring comparatively with daily sequential organ failure assessment scoring for predicting hospital mortality in critically ill patients. Crit Care Med 30:2003–2013
Calvino Gunther S, Schwebel C, Vesin A, Remy J, Dessertaine G, Timsit JF (2009) Interventions to decrease tube, line, and drain removals in intensive care units: the FRATER study. Intensive Care Med 35:1772–1776
de Lassence A, Alberti C, Azoulay E, Le Miere E, Cheval C, Vincent F, Cohen Y, Garrouste-Orgeas M, Adrie C, Troche G, Timsit JF (2002) Impact of unplanned extubation and reintubation after weaning on nosocomial pneumonia risk in the intensive care unit: a prospective multicenter study. Anesthesiology 97:148–156
Darmon M, Timsit JF, Francais A, Nguile-Makao M, Adrie C, Cohen Y, Garrouste-Orgeas M, Goldgran-Toledano D, Dumenil AS, Jamali S, Cheval C, Allaouchiche B, Souweine B, Azoulay E (2010) Association between hypernatraemia acquired in the ICU and mortality: a cohort study. Nephrol Dial Transpl 25:2510–2515
Zahar JR, Nguile-Makao M, Francais A, Schwebel C, Garrouste-Orgeas M, Goldgran-Toledano D, Azoulay E, Thuong M, Jamali S, Cohen Y, de Lassence A, Timsit JF (2009) Predicting the risk of documented ventilator-associated pneumonia for benchmarking: construction and validation of a score. Crit Care Med 37:2545–2551
Beyersmann J, Schumacher M (2008) Time-dependent covariates in the proportional subdistribution hazards model for competing risks. Biostatistics 9:765–776
Loveday HP, Pellowe CM, Jones SR, Pratt RJ (2006) A systematic review of the evidence for interventions for the prevention and control of meticillin-resistant Staphylococcus aureus (1996–2004): report to the Joint MRSA Working Party (Subgroup A). J Hosp Infect 63(Suppl 1):S45–S70
Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, Duckworth GJ, Lai R, Ebrahim S (2003) Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling. Health Technol Assess 7:1–194
Jarlier V, Trystram D, Brun-Buisson C, Fournier S, Carbonne A, Marty L, Andremont A, Arlet G, Buu-Hoi A, Carlet J, Decre D, Gottot S, Gutmann L, Joly-Guillou ML, Legrand P, Nicolas-Chanoine MH, Soussy CJ, Wolf M, Lucet JC, Aggoune M, Brucker G, Regnier B (2010) Curbing methicillin-resistant Staphylococcus aureus in 38 French hospitals through a 15-year institutional control program. Arch Intern Med 170:552–559
Harbarth S, Masuet-Aumatell C, Schrenzel J, Francois P, Akakpo C, Renzi G, Pugin J, Ricou B, Pittet D (2006) Evaluation of rapid screening and pre-emptive contact isolation for detecting and controlling methicillin-resistant Staphylococcus aureus in critical care: an interventional cohort study. Crit Care 10:R25
Saint S, Higgins LA, Nallamothu BK, Chenoweth C (2003) Do physicians examine patients in contact isolation less frequently? A brief report. Am J Infect Control 31:354–356
Kirkland KB, Weinstein JM (1999) Adverse effects of contact isolation. Lancet 354:1177–1178
Lesko LM, Kern J, Hawkins DR (1984) Psychological aspects of patients in germ-free isolation: a review of child, adult, and patient management literature. Med Pediatr Oncol 12:43–49
Klein BS, Perloff WH, Maki DG (1989) Reduction of nosocomial infection during pediatric intensive care by protective isolation. N Engl J Med 320:1714–1721
Bouadma L, Mourvillier B, Deiler V, Le Corre B, Lolom I, Regnier B, Wolff M, Lucet JC (2010) A multifaceted program to prevent ventilator-associated pneumonia: impact on compliance with preventive measures. Crit Care Med 38:789–796
Ammerlaan HS, Troelstra A, Kruitwagen CL, Kluytmans JA, Bonten MJ (2009) Quantifying changes in incidences of nosocomial bacteraemia caused by antibiotic-susceptible and antibiotic-resistant pathogens. J Antimicrob Chemother 63:1064–1070
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was written on behalf the OUTCOMEREA study Group.
Rights and permissions
About this article
Cite this article
Zahar, J.R., Garrouste-Orgeas, M., Vesin, A. et al. Impact of contact isolation for multidrug-resistant organisms on the occurrence of medical errors and adverse events. Intensive Care Med 39, 2153–2160 (2013). https://doi.org/10.1007/s00134-013-3071-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-3071-0