Abstract
Purpose
During volume-controlled ventilation, part of the volume delivered is compressed into the circuit. To correct for this phenomenon, modern ventilators use compensation algorithms. Humidity and temperature also influence the delivered volume.
Methods
In a bench study at a research laboratory in a university hospital, we compared nine ICU ventilators equipped with compensation algorithms, one with a proximal pneumotachograph and one without compensation. Each ventilator was evaluated under normal, obstructive, and restrictive conditions of respiratory mechanics. For each condition, three tidal volumes (V T) were set (300, 500, and 800 ml), with and without an inspiratory pause. The insufflated volume and the volume delivered at the Y-piece were measured independently, without a humidification device, under ambient temperature and pressure and dry gas conditions. We computed the actually delivered V T to the lung under body temperature and pressure and saturated water vapour conditions (BTPS).
Results
For target V T values of 300, 500, and 800 ml, actually delivered V T under BTPS conditions ranged from 261 to 396 ml (−13 to +32%), from 437 to 622 ml (−13 to +24%), and from 681 to 953 ml (−15 to +19%), respectively (p < 0.01). Respiratory system mechanics and application of an inspiratory pause significantly affected actually delivered V T. Assuming a set V T of 6 ml/kg of predicted body weight, a difference of 1–2 ml/kg with actually delivered V T would be commonly observed.
Conclusion
The difference between preset V T and actually delivered V T is clinically meaningful and differs across modern ICU ventilators.
Similar content being viewed by others
Introduction
The use of low tidal volumes (V T) in patients ventilated for acute respiratory distress syndrome (ARDS) has markedly improved survival rates [1]. A protective strategy using a V T of 6 ml/kg of predicted body weight helps to limit the alveolar damage induced by mechanical ventilation. Therefore, accurate control of the volume delivered by the ventilator has become of the utmost importance. During volume-controlled ventilation, the V T actually delivered to the patient may differ from the preset V T for several reasons. During the insufflation time, airway pressure rises within the ventilator circuit, causing gas compression (Boyle’s law) and, midly, tubing distension. As a result, part of the volume exiting the ventilator is compressed into the circuit and does not reach the patient [2]. At expiration, airway pressure decreases, leading to decompression of the gas. Both the volume exhaled by the patient and the volume compressed in the circuit are released through the exhalation valve and measured by spirometry [3]. The volume wasted by compression in the circuit may become meaningful when small volumes or high pressures are used, as may occur in patients with severe lung disease. Ventilator manufacturers have therefore equipped their intensive care unit (ICU) ventilators with algorithms that compensate for the effect of gas compression.
Moreover, V T is delivered by the ventilator under ambient temperature and pressure and dry gas conditions (ATPD). However, the V T in the patient’s lungs is at body temperature and pressure, and saturated with water vapour (BTPS). For a given amount of gas, the volume increases when temperature and humidity increase because of the physical properties. Therefore, the passage from ATPD to BTPS partially counteracts the volume decrease caused by gas compression. Studies of actually delivered V T compared to preset V T should therefore take into account not only gas compression, but also the passage from ATPD to BTPS.
The purpose of our study was to evaluate the ability of ICU ventilators to deliver accurate V T with various simulated respiratory mechanical loads. The preliminary results of this study were presented at the 2008 meeting of the European Society of Intensive Care Medicine [4].
Methods
A detailed method section is available in the electronic supplementary material.
Design of the experiment
We tested ICU ventilators on a Michigan test lung (Training Test Lung, Michigan Instruments, Grand Rapids, MI, USA). Each ventilator tested was connected to the single-lung test lung via an endotracheal tube and a ventilator circuit (Intersurgical, Berkshire, UK).
Ventilators were tested in volume-controlled mode with a square inspiratory flow of 60 l/min and three preset V T values of 300, 500, and 800 ml, respectively. To evaluate the impact of a pause on the compensation algorithm, we tested the three conditions with and without a 1-s end-inspiratory pause.
Three combinations of compliance (C) and resistance (R) were used to simulate normal, obstructive, and restrictive conditions: normal with a resistance of 5 cmH2O/L/s and a compliance of 60 ml/cmH2O, chronic obstructive pulmonary disease (COPD) with a resistance of 20 cmH2O/L/s and a compliance of 60 ml/cmH2O, and acute respiratory distress syndrome (ARDS) with a resistance of 5 cmH2O/L/s and a compliance of 30 ml/cmH2O.
A low respiratory frequency (14 cycles/min) was used to minimise the risk of gas trapping. All measurements were performed using an FiO2 of 21% and a positive end-expiratory pressure (PEEP) of 5 cmH2O.
Before the measurements, each ventilator was tested according to the procedure described in the manufacturer’s user manual.
Compensation for tidal volume compressed in the circuit
To evaluate compensation algorithms, we measured the volume insufflated by the ventilator at the point of exit from the ventilator (beginning of the circuit) and the V T delivered to the test lung at the Y-piece (end of the circuit).
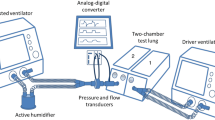
For this purpose, we used two calibrated Fleisch no. 2 pneumotachographs, one at the beginning of the inspiratory circuit (at the point of exit from the ventilator) to measure the volume insufflated by the ventilator and the other at the end of inspiratory circuit (Y-piece) to measure the V T delivered to the patient (Fig. 1).
Diagram of experimental setup used to evaluate the delivered tidal volume (V T) compared to the preset V T in a passive bench model. Flow traces were recorded using two pneumotachographs, one at the ventilator inspiratory valve to measure the insufflated volume in the circuit and the other at the Y-piece to measure delivered V T under ambient temperature and pressure and dry gas conditions (ATPD). This volume was converted to the value under body temperature and pressure saturated with water vapour conditions (BTPS) to estimate the V T actually delivered to the patient’s lungs
We compared the volume insufflated by the ventilator, the V T delivered to the test lung under ATPD conditions, the actually V T delivered to a patient under BTPS conditions, and the V T preset on the ventilator. Each measurement was recorded for 1 min after stabilisation and averaged over three cycles.
Ventilators
We evaluated new-generation ICU ventilators equipped with algorithms that compensated for the compressed volume in the circuit, namely, Avea (Viasys Healthcare, Conshohocken, PA), Elisée 350 (Resmed-Saime, North Ryde, Australia), Engström (General Electric, Fairfield, CO), Esprit (Respironics, Murrysville, PA), Extend (Taema, Antony, France), Evita XL (Dräger, Lübeck, Germany), Galileo (Hamilton, Rhäzuns, Switzerland), PB 840 (TYCO, Carlsbad, CA, USA), and Servo I (Maquet, Solna, Sweden). Two of these nine ventilators could be used with and without activation of the compensation algorithm (Avea and Servo I) and were tested in the two conditions. We compared these ventilators with two old-generation ICU ventilators, namely the Puritan-Bennett 7200 (TYCO, Carlsbad, CA), one of the first ventilators equipped with a compensation algorithm, and the Bird 8400 (Viasys Healthcare, Conshohocken, PA), which does not have a compensation algorithm. It must be noted that the Galileo ventilator measures V T via a proximal flow sensor at the Y-piece and was therefore included in the group of ventilators equipped with compensation algorithms.
ATPD/BTPS
The pneumotachograph at the Y-piece measured V T under ATPD conditions, since no humidification device was used. To estimate the V T actually delivered to the lungs under BTPS conditions, we used the psychrometric method to measure gas temperature and hygrometry at the Y-piece [5]. After measuring temperature and hygrometry, we estimated V T under BTPS conditions by converting the V T under ATPD conditions, using the following formula:
-
Gas volume at BTPS = gas volume at ATPD (barometric pressure − water vapour pressure/barometric pressure − 47) × 310/273 + temperature in °C)
where 47 is the vapour pressure of water at 37°C, 273 is Kelvin at 0°C, and 310 is Kelvin at 37°C (body temperature).
The ATPD to BTPS correction increased the mean delivered V T by 11.6% for compressed gas ventilators and by 10.4% for turbine ventilators.
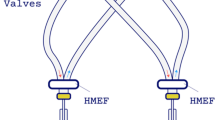
Humidification
All tests were performed without any humidification device. When we measured baseline circuit compliance we found an approximate increase of 10% with an HH compared to an HME. Once taken into account into the compensation algorithm of the ventilator, the difference became negligible. The resistive effect of these devices was also considered negligible. For details, see the electronic supplementary material.
Also, three ventilators allowed different humidification settings (Avea, Evita XL, and Engström), and we measured delivered V T with the two settings available on the ventilator, namely, heat and moisture exchanger or heated humidifier.
Statistical analysis
We used multiple analyses of variance to evaluate the impact of respiratory mechanics, physical conditions, and ventilator settings (preset V T and application of a pause) on V T accuracy. When the global F was significant, post hoc comparisons were done using Bonferroni test for multiple comparisons. Ventilators with and without compensation algorithms were compared for each variable using unpaired Student’s t-tests. p values smaller than 0.05 were considered statistically significant.
Results
Comparison of actually delivered tidal volumes
Delivered V T differed significantly across ventilators (p < 0.01). For target V T values of 300, 500, and 800 ml, actually delivered V T under BTPS conditions ranged from 261 to 396 ml (−13 to +32%), 437–622 ml (−13 to +24%), and 681–953 ml (−15 to +19%), respectively (p < 0.01) (Fig. 2). The absolute difference (positive or negative) between the preset V T and the actually delivered V T under BTPS conditions was greater than 25% with one ventilator (Extend), 15–25% with three ventilators (Servo I with compensation, Engström, and Elisée 350), 5–15% with seven ventilators (Bird 8400, AVEA with and without compensation, Servo I without compensation, Galileo, Esprit, PB 7200, and PB 840), and lower than 5% with one ventilator (Evita XL). With V T preset at 6 ml/kg of predicted body weight, 17% of volume error represents an error of 1 ml/kg. Thus, errors may frequently range from 1 to 2 ml/kg.
Figure showing the volume error [as the percentage of preset tidal volume (V T)] for all ventilators tested using three preset V T values (800, 500, and 300 ml from top to bottom) and three respiratory mechanics conditions (normal in white, restrictive condition simulating ARDS in grey, and obstructive condition simulating COPD in black) under BTPS conditions (actually delivered V T). The volume errors frequently reached 15% of the preset V T or about 1 ml/kg of predicted body weight, *p < 0.05 versus normal condition. ARDS acute respiratory distress syndrome, COPD chronic obstructive pulmonary disease
VT indicated by the ventilator was significantly different from the actually delivered VT under BTPS conditions (p < 0.01) (Fig. 3). The actually delivered VT was greater than the VT indicated by the ventilator with all ventilators except PB 840 and AVEA without compensation. When VT was preset at 300 ml, the absolute difference between the actually delivered VT and the VT indicated by the ventilator was greater than 20% with one ventilator (Extend), 10–20% with five ventilators (Esprit, PB 7200, Servo I with compensation, Engström, and Elisée 350), and less than 5% with three ventilators (Galileo, PB 840, and Evita XL).
Actually delivered tidal volume (V T) under BTPS conditions in black and V T indicated by the ventilator in red for all ventilators tested using three V T values (800, 500, and 300 ml from top to bottom). V T values are the means of six conditions: three respiratory system mechanics conditions with and without an inspiratory pause. The V T indicated by the ventilator was lower than the actually delivered V T, and the difference was often greater than 10% of the preset V T
Impact of the compensation algorithm on delivered tidal volume
In all conditions, V T was significantly larger with ventilators using compensation algorithms compared to ventilators without compensation algorithms (p < 0.01). Under ATPD conditions, the volume error was significantly smaller with ventilators using compensation algorithms (p < 0.01). As expected, the actually delivered V T under BTPS conditions was larger than the V T delivered at the Y-piece in ATPD conditions (p < 0.01) (Fig. 4). Consequently, ventilators using compensation algorithms delivered actual V T values under BTPS conditions that were larger than the preset V T.
Box plots showing the median value (25th–75th percentiles) of the volume error under ATPD and BTPS conditions using ventilators with (grey squares) and without (white squares) compensation algorithms. Results are given for a preset tidal volume of 300 ml in three respiratory system conditions: restrictive simulating ARDS at the top, normal in the middle, and obstructive simulating COPD at the bottom. Actually delivered tidal volumes were larger with ventilators using compensation algorithms than with ventilators not using compensation algorithms and were larger than the preset tidal volume, *p < 0.05 versus ATPD without compensation, # p < 0.05 versus BTPS without compensation. ATPD ambient temperature and pressure and dry gas condition, BTPS body temperature and pressure and saturated water vapour conditions, ARDS acute respiratory distress syndrome, COPD chronic obstructive pulmonary disease
Effect of respiratory system conditions
For a similar preset V T, the delivered V T differed significantly across the three mechanical respiratory conditions (normal, restrictive, and obstructive patterns, p < 0.01) (Fig. 2). The delivered V T was smaller under restrictive conditions than normal conditions with all ventilators except Evita XL. Compared to normal conditions, this difference sometimes exceeded 10% with the three ventilators using no compensation algorithms (Bird 8400, Avea, and Servo I without compensation).
Impact of inspiratory pause
For a given preset V T value, application of an inspiratory pause significantly modified the actually delivered V T in the obstructive condition (p < 0.05) (Fig. 5). With V T preset at 300 ml, the application of an inspiratory pause decreased the delivered V T by more than 10% with three ventilators (Galileo, PB 840, and Servo I with compensation) (Figs. 5 and 6).
Volume error [as the percentage of the preset tidal volume (VT)] for all ventilators tested under BTPS conditions (actually delivered V T). Volume error was obtained for a preset V T of 300 ml in the obstructive condition with a large difference between peak and plateau pressures due to high resistance. With this respiratory system condition, adding a pause markedly changed the V T actually delivered by ventilators using a compensation algorithm based on end-inspiratory pressure
Humidification strategy
Three ventilators could be set to either a heat and moisture exchanger or a heated humidifier. Activation of the heated humidifier decreased the delivered V T by 10 and 15% with the Avea and Engström ventilators, respectively, and had no effect with the Evita XL ventilator.
Discussion
We used a lung model to accurately measure the delivered V T during volume-controlled ventilation with a large number of ICU ventilators. We found wide variations in delivered V T. The ventilators using compensation algorithms delivered larger volumes than the ventilators without compensation. Actually delivered V T values under BTPS conditions were lower than preset V T with ventilators that did not use compensation and larger than preset V T with ventilators that used compensation. The volume error varied significantly across ventilators and often reached 15–17%, representing about 1 ml/kg for a preset V T volume at 6 ml/kg of predicted body weight. The V T indicated by the ventilator was lower than the actually delivered V T, and this difference was often greater than 10%. For a similar preset V T, respiratory system conditions and the application of an inspiratory pause significantly influenced the delivered V T.
Clinical implications
Several studies have compared ICU ventilators in terms of trigger function and pressurization capability during pressure-support ventilation [6–8], but to the best of our knowledge there are no previous comparative data on actually delivered V T during volume-controlled ventilation. We compared most of the new-generation ICU ventilators that are currently available. Ventilation with a low V T is crucial to minimise alveolar damage and mortality in ARDS patients [1]. However, several studies found no differences between 7 and 10 ml/kg of preset V T, suggesting a role for confounding factors [9–11]. We found that the actually delivered V T varied substantially across ventilators. The largest difference between two ventilators represented respectively 32, 25, and 21% of the preset V T at 300, 500, and 800 ml. These differences in actually delivered V T for a given preset V T may have confounded the results of studies investigating the effects of V T values on ARDS outcomes. Moreover, we found significant differences between the V T values indicated by the ventilators and the actually delivered V T values.
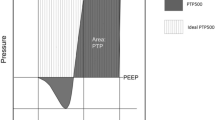
Compensation algorithm
Recent algorithms for compensation are based on peak airway pressure and others on end-inspiratory pressure corresponding to either a peak or a plateau pressure when applying an inspiratory pause. In these ventilators, applying an inspiratory pause without changing the preset V T led to a substantial decrease in actually delivered V T. Surprisingly, these ventilators changed the actually delivered V T without modifying the preset V T (Fig. 6). The difference was more pronounced in the obstructive condition simulating COPD, a disease characterised by high resistance (high peak airway pressure) and high compliance (low plateau pressure) of the respiratory system and, therefore, by a large difference between peak and plateau pressures. When simulating ARDS (restrictive condition), most ventilators without compensation algorithms were unable to compensate for the wasted volume due to high airway pressure, and the actually delivered V T therefore dropped by more than 10% compared to the normal condition.
Compared with ventilators without compensation algorithms, ventilators with compensation algorithms had larger actually delivered V T values. However, this actually delivered V T was larger than the preset V T, suggesting overcompensation by the algorithms.
ATPD/BTPS
The V T delivered at the Y-piece is under ATPD conditions, i.e., dry gas at ambient temperature and pressure. The hygrometry of the gas differs depending on whether compressed gas from a wall outlet or a turbine is used. Compressed gas wall outlets deliver dry gas (air and O2 mixture), and turbines produce a mixture of dry compressed oxygen and ambient air. Consequently, humidity is higher when a turbine is used. When the gas enters the lungs, it is warmed to 37°C and completely saturated with water vapour (BTPS). Therefore, to deliver the preset V T, the ventilator must use an algorithm that takes into account both the volume decrease related to gas compression in the circuit and the volume increase induced by warming and water vapour saturation.
Several previous studies have compared the V T indicated by the ventilator and the V T actually delivered to the patient. Three clinical paediatric studies found significant differences between the V T measured at the expiratory valve and the exhaled V T measured using a pneumotachograph at the Y-piece [12–14]. However, these two V T values should differ, as the temperature and humidity conditions differ between the two measurement sites. Thus, the V T measured by the ventilator at the expiratory valve should be smaller than the V T measured at the Y-piece, because the gas cools and loses humidity along of the expiratory tubing. These three studies did not take hygrometry into account.
Humidification device
Larger V T values would be expected at the Y-piece with a heated humidifier than with a heat and moisture exchanger. However, the actually delivered V T into the patient’s lungs (BTPS) must be the same due to higher temperature and humidity [15]. Surprisingly, we found, however, that two ventilators reduced the insufflated volume when the heated humidifier condition was turned on. The V T measured at the expiratory valve should differ according to whether heated circuits are used.
Limitations
Advantages of the lung model used in our study include standardization of the mechanical characteristics, repeatability of the ventilator tests, and the ability to study a broad range of situations. The lung model closely replicates the V T actually delivered to the patient, after correction for BTPS conditions. The ideal study should accurately measure the V T exhaled by the patient irrespective of the ventilatory settings and humidification device. We measured V T with no humidification device. Therefore, our results may not reflect the V T values obtained with heated humidifiers. However, in most cases the V T at the ventilator exit point is probably similar with and without a heated humidifier.
In summary, despite the use of compensation algorithms, ventilators differ in their ability to deliver the preset V T, and substantial differences may exist between the preset V T and the V T under BTPS conditions in the patient’s lungs. When V T was set at 6 ml/kg of predicted body weight, differences ranging from 1 to 2 ml/kg were common. Such differences may have clinical consequences in terms of both alveolar ventilation and the risk of ventilator-induced lung injury.
References
(2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 342:1301-1308
Cote CJ, Petkau AJ, Ryan JF, Welch JP (1983) Wasted ventilation measured in vitro with eight anesthetic circuits with and without inline humidification. Anesthesiology 59:442–446
Forbat AF, Her C (1980) Correction for gas compression in mechanical ventilators. Anesth Analg 59:488–493
Lyazidi A, Richard JC-M, Thille AW, Besson O, Brochard L (2008) Are tidal volume delivered by the ventilator and received by the patient similar? Intensive Care Med 34:A0756
Lellouche F, Taille S, Maggiore SM, Qader S, L’Her E, Deye N, Brochard L (2004) Influence of ambient and ventilator output temperatures on performance of heated-wire humidifiers. Am J Respir Crit Care Med 170:1073–1079
Ferreira JC, Chipman DW, Kacmarek RM (2008) Trigger performance of mid-level ICU mechanical ventilators during assisted ventilation: a bench study. Intensive Care Med 34:1669–1675
Thille AW, Lyazidi A, Richard JC, Galia F, Brochard L (2009) A bench study of intensive care unit ventilators: new versus old and turbine-based versus compressed gas-based ventilators. Intensive Care Med 35:1368–1376
Richard JC, Carlucci A, Breton L, Langlais N, Jaber S, Maggiore S, Fougere S, Harf A, Brochard L (2002) Bench testing of pressure support ventilation with three different generations of ventilators. Intensive Care Med 28:1049–1057
Brochard L, Roudot-Thoraval F, Roupie E, Delclaux C, Chastre J, Fernandez-Mondejar E, Clementi E, Mancebo J, Factor P, Matamis D, Ranieri M, Blanch L, Rodi G, Mentec H, Dreyfuss D, Ferrer M, Brun-Buisson C, Tobin M, Lemaire F (1998) Tidal volume reduction for prevention of ventilator-induced lung injury in acute respiratory distress syndrome. The multicenter trail group on tidal volume reduction in ARDS. Am J Respir Crit Care Med 158:1831–1838
Stewart TE, Meade MO, Cook DJ, Granton JT, Hodder RV, Lapinsky SE, Mazer CD, McLean RF, Rogovein TS, Schouten BD, Todd TR, Slutsky AS (1998) Evaluation of a ventilation strategy to prevent barotrauma in patients at high risk for acute respiratory distress syndrome. Pressure- and volume-limited Ventilation Strategy Group. N Engl J Med 338:355–361
Brower RG, Shanholtz CB, Fessler HE, Shade DM, White P Jr, Wiener CM, Teeter JG, Dodd-o JM, Almog Y, Piantadosi S (1999) Prospective, randomized, controlled clinical trial comparing traditional versus reduced tidal volume ventilation in acute respiratory distress syndrome patients. Crit Care Med 27:1492–1498
Cannon ML, Cornell J, Tripp-Hamel DS, Gentile MA, Hubble CL, Meliones JN, Cheifetz IM (2000) Tidal volumes for ventilated infants should be determined with a pneumotachometer placed at the endotracheal tube. Am J Respir Crit Care Med 162:2109–2112
Castle RA, Dunne CJ, Mok Q, Wade AM, Stocks J (2002) Accuracy of displayed values of tidal volume in the pediatric intensive care unit. Crit Care Med 30:2566–2574
Neve V, Leclerc F, Noizet O, Vernoux S, Leteurtre S, Forget P, Sadik A, Riou Y (2003) Influence of respiratory system impedance on volume and pressure delivered at the Y piece in ventilated infants. Pediatr Crit Care Med 4:418–425
Fujita Y, Imanaka H, Fujino Y, Takeuchi M, Tomita T, Mashimo T, Nishimura M (2006) Effect of humidifying devices on the measurement of tidal volume by mechanical ventilators. J Anesth 20:166–172
Author information
Authors and Affiliations
Corresponding author
Additional information
In collaboration with the “Groupe de Travail sur les Respirateurs AP-HP”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lyazidi, A., Thille, A.W., Carteaux, G. et al. Bench test evaluation of volume delivered by modern ICU ventilators during volume-controlled ventilation. Intensive Care Med 36, 2074–2080 (2010). https://doi.org/10.1007/s00134-010-2044-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-2044-9