Abstract
Objective
To assess the distribution of bacterial species and antimicrobial resistance in an ICU during long-term use of selective digestive decontamination (SDD) in the context of national reference data.
Design and setting
Five-year prospective observational study in a 24-bed interdisciplinary surgical ICU of a university hospital (study ICU) participating in the project “Surveillance of Antimicrobial Use and Antimicrobial Resistance in German Intensive Care Units” (SARI; reference ICUs).
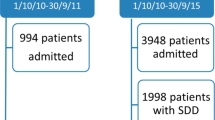
Patients
Resistance data were obtained from all patients; patients intubated for at least 2 days received SDD (colistin, tobramycin, amphotericin B).
Interventions and measurements
SDD was performed in 1,913 of 7,270 patients. Antimicrobial resistance was examined in 4,597 (study ICU) and 46,346 (reference ICUs) isolates.
Results
Methicillin-resistant Staphylococcus aureus (MRSA) remained stable (2.76 and 2.58 isolates/1000 patient days) in the study ICU; this was below the German average (4.26 isolates/1000 patient days). Aminoglycoside- and betalactam-resistant Gram-negative rods did not increase during SDD use. Aminoglycoside resistance of Pseudomonas aeruginosa was 50% below the mean value of SARI (0.24 vs. 0.52 isolates/1,000 patient days). The relative frequency of enterococci and coagulase-negative staphylococci (CNS) was higher than in the SARI ICUs (23.2% vs. 17.3%, and 25.0% vs. 20.6%, respectively).
Conclusion
Routine 5-year-use of SDD was not associated with increased antimicrobial resistance in our ICU with low baseline resistance rates. Vigorous surveillance and control measures to search and destroy MRSA were considered a mandatory component of the SDD program. The relative increase in enterococci and CNS is of concern requiring further investigation.
Similar content being viewed by others
Introduction
Intensive care unit (ICU) patients are at high risk to develop severe infections, respiratory infections being the most frequent [1]. Ventilator-associated pneumonia has been associated with an attributable mortality of approx. 30% [2]; it contributes to increased morbidity, prolonged ICU stay and additional costs [3]. Obviously prophylaxis of such infections is highly desirable.
Selective digestive decontamination (SDD) is an intervention aimed at preventing infections by selectively eradicating aerobic Gram-negative bacteria, Staphylococcus aureus, and yeasts from the oropharynx and the digestive tract [4, 5, 6]. SDD consists of topical application of nonabsorbable antimicrobials (generally polymyxin, an aminoglycoside, and amphotericin B); in many trials an intravenous antibiotic is added for the first days. Although reduced pneumonia rates [7] and even survival benefit for certain ICU patients have been shown in meta-analyses [8, 9] and in prospective, randomized trials [10, 11, 12] of SDD, the routine use of SDD remains controversial. Proponents claim level 1 evidence for broad-range use of SDD [13, 14] while other reviewers warn against it [15, 16], arguing that SDD promotes the emergence of antibiotic resistance [7, 15]. The increase in micro-organisms that are intrinsically resistant to the applied antibiotics, i.e., methicillin-resistant S. aureus (MRSA) or vancomycin-resistant enterococci (VRE), is suspected as well as the emergence of aminoglycoside-resistant Gram-negative bacteria [7, 15, 17]. The available studies come to conflicting conclusions ranging from “ecological disaster” [18] to a reduction in antimicrobial resistance with consequent savings of antibiotics [11]. However, in many studies the SDD-treated subgroup of the examined patient population was too small or the time period too short to elucidate this problem [7].
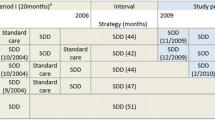
Therefore we present a 5-year prospective observation of antibiotic resistance in our surgical ICU, where SDD is routinely applied in patients intubated for at least 2 days. To determine the effect of long-term SDD application on antimicrobial resistance we compared the incidence of resistant isolates in the study ICU at the beginning of SDD use with the findings during the following 4 years. In addition to this internal comparison, the resistance data of our ICU were compared to data from 33 ICUs not using SDD, as provided by the project “Surveillance of Antimicrobial Use and Antimicrobial Resistance in German Intensive Care Units” (SARI) [19, 20].
Materials and methods
Setting and study design
The study was performed in a 24-bed surgical ICU in a German university hospital. Adult patients of all surgical departments were treated in this tertiary care ICU. Patients intubated for at least 2 days routinely received SDD until extubation. The topical SDD component consisted of colistin, tobramycin, and amphotericin B dissolved in aqua destillata. Every 6 h 5 ml each was given orally and into the stomach. A written protocol for a systemic component was not used, but an intravenous antibiotic, either as anti-infectious treatment or as perioperative prophylaxis (usually first or second generation cephalosporine), was administered in approx. 90% of the affected patients within the first 2 days of admission to the ICU.
Antibiotic resistance rates and the distribution of bacterial species were prospectively monitored in the SARI project between February 2000 and December 2004. ICU surveillance cultures for any bacterial or fungal species were performed in the study twice weekly from tracheal secretions and urine for all patients, independently of SDD use. Furthermore, since 2001 all patients have been screened for MRSA. For this aim a set of samples (nasal swab and tracheal secretions—or throat swabs from spontaneously breathing patients) was examined on admission, once weekly during ICU stay and before transfer. The MRSA screening was combined with rigorous isolation measures for MRSA carriers in one-bed rooms.
Specific microbiological examinations for suspected infections were carried out as ordered by intensivists. Susceptibility testing was performed using broth-microdilution or disc-diffusion methods according to guidelines published by the National Committee for Clinical Laboratory Standards [21]. Tobramycin was used to test for aminoglycoside resistance; amikacin resistance was not tested. From 2000 to 2002 the resistance data were listed by hand; beginning in 2003 the data were extracted from the microbiology laboratory database Hybase (Cymed, Bochum, Germany). As prescribed for the members of SARI, device-associated infections were assessed in the German Hospital Infection Surveillance System (Krankenhaus Infection Surveillance System, Kiss; www.nrz-hygiene.de) [20, 22]. Demographic and medical information for the study were extracted from the electronic ICU database. The longitudinal course of resistance data in the study ICU was compared with the findings at the beginning of SDD use. The reference data of SARI and KISS served for comparison to rank the findings in a nationwide context.
The SARI project
SARI is part of the research network “Spread of Nosocomial Infections and Resistant Pathogens.” This national surveillance system was initiated in February 2000 to provide an estimate of the prevalence of antimicrobial-resistant micro-organisms in German ICUs, as described previously [19, 20]. The SARI project leaves the collection and processing of microbiological samples to the routine of the participants. At present 40 ICUs contribute to the project. The microbiology laboratories serving the ICUs deliver the number of tested and resistant isolates for 13 sentinel bacterial species regardless of whether they are associated with infection or colonization. “Copy” or duplicate strains are excluded; a copy strain is defined as an isolate of the same species of bacteria showing the same antimicrobial susceptibility pattern in the same patient throughout a 1-month period, independently of the site of isolation [20]. This definition was applied for all ICUs participating in SARI, including the study ICU. In this study the results of all ICUs of the SARI project which do not use SDD served as national reference data to rank the findings in the study ICU.
Patients
During the 5-year study period 7,270 patients were admitted to the study ICU; SDD was carried out in 1,913 of these (60.12% male); their mean length of ICU stay was 14.75 ± 11.39 days. The most frequent reasons for intensive care treatment were neurosurgical interventions (25.9%), cardiovascular surgery (23.7%), severe trauma (17.1%), extended abdominal surgery or peritonitis (14.5%), and respiratory insufficiency after any type of surgical intervention (10.9%). In the study ICU 4,597 bacterial isolates were obtained from the total patient population. Approx. 70–80% of these originated from surveillance cultures. The 33 non-SDD ICUs reported 47,127 isolates. The number of isolates per 1,000 patient days was 139.2 in study ICU and 86.1 in the non-SDD SARI ICUs (pooled mean). This difference is a reflection of the different examination habits in the SARI project.
Statistics
The incidence density (ID) of resistant isolates was defined as: [(number of isolates of a bacterial species resistant to a tested antimicrobial in 1 year)/number of patient days in the same year)] × 1,000. Differences between the yearly IDs within the study ICU and compared with the non-SDD SARI ICUs were tested by the incidence density test. The proportion of each bacterial species (with the exception of S. aureus) in the examined spectrum was calculated as: [(number of isolates of a species)/number of isolates of all examined species, excluding S. aureus)] × 100. S. aureus was excluded to avoid a distortion of the calculation since this species was overrepresented in the study ICU due to the MRSA screening, which is uncommon in the reference ICUs. Significance was set at p = 0.05. Statistical analyses were performed using SAS version 9.1 and EpiInfo 6.04.
Results
The relative proportion of the bacterial species in the total spectrum is presented in Fig. 1, showing a low percentage of Enterobacteriaceae (with the exception of Serratia marcescens) and of nonfermenters in the study ICU. The proportion of enterococci, coagulase-negative staphylococci (CNS) and S. marcescens was above the 75th percentile of the reference ICUs. A comparison of S. aureus isolates was abandoned since the results would be distorted by the MRSA screening in the study ICU. This surveillance is widely uncommon in the non-SDD SARI-ICUs, but resulted in the detection of large numbers of Staphylococcus aureus isolates in the study ICU.
The spectrum of isolated bacterial species is presented for the study ICU (black bars) in comparison with the pooled mean of the reference ICUs (hatched bars). The results are given in percentages. The proportion of any particular bacterial species (with the exception of S. aureus) was calculated as: [(number of tested isolates of the species)/number of tested isolates of all species excluding S. aureus)] × 100. S. aureus was excluded from this calculation since a disproportionately high number of isolates of this species resulted from MRSA screening, which is uncommon in the reference ICUs. ++, – – Outlier in the study ICU above the 75th and below the 25th percentile of the non-SDD SARI ICUs
The incidence densities of micro-organisms resistant against the applied topical antibiotics are presented in Table 1. Methicillin resistance of S. aureus in the study ICU proved stable when the incidence density of the first year of MRSA screening (2001) was compared to that during the last year of the study period (2.76 vs. 2.58/1,000 patient days). On average the number of MRSA per 1,000 patient days was significantly lower in the study ICU than in the reference ICUs (3.24 vs. 4.40, p < 0.01; Table 1). In the study ICU, vancomycin resistance was neither observed in S. aureus nor in Enterococcus faecalis. Vancomycin-resistant Enterococcus faecium was introduced with a notoriously colonized patient in the year 2001 and 2003, respectively. At the end of 2004, however, five cases of vancomycin resistant E. faecium appeared (ID 0.68/1,000 patient days; Fig. 2, Table 1). The numbers of VRE isolates in the complete hospital and in the study ICU (Fig. 2) are presented month by month in Fig. 2. Genotyping results revealed that two strains predominated, indicating a hospital-wide outbreak, which stopped by the middle of 2005 (personal communication Dr. Stefan Borgmann, Department of Medical Microbiology and Hospital Infection Control, Tübingen University Hospital).
In the study ICU no aminoglycoside-resistant Gram-negative isolates were found until 2002, but in 2003 a peak appeared for Pseudomonas aeruginosa, Enterobacter cloacae, and Klebsiella pneumoniae (Table 1) and in 2004 for Escherichia coli. However, four of the five aminoglycoside-resistant E. coli, the aminoglycoside-resistant Klebsiella and Enterobacter isolates, and four of the seven resistant pseudomonads were obtained within the first 48 h of ICU admission of the patients in question.
Resistance to antimicrobial substances not part of the topical SDD regimen is presented in Fig. 3. The incidence density of resistant isolates is summarized for the three most important Gram-negative pathogens. The mean rate of ventilator-associated pneumonia was consistently low in the study ICU, with 4.2 infections per 1,000 ventilator days. This was below the 25th percentile (4.3) found in the surgical ICUs of the KISS project. The mean rate of 2.8 catheter-related bloodstream infections per 1,000 catheter days in the study ICU was equal to the 75th percentile of these reference ICUs.
The incidence density of isolates (number of isolates per 1,000 patient days) of the three most frequent Gram-negative bacterial species, which were resistant to β-lactams and quinolones are given as the pooled mean of the years 2000–2004. The study ICU and the 33 non-SDD ICUs are presented by grey and dotted bars, respectively. The tested third-generation cephalosporine was ceftazidime in Pseudomonas aeruginosa isolates; otherwise cefotaxime was tested. Meropenem or imipenem was tested to represent the carabapenems
Discussion
The prevalence of antimicrobial resistance in an ICU is determined by various factors. Mutation of initially susceptible micro-organisms probably plays a minor role because it occurs only sporadically. The selection of preexisting resistant strains during antibiotic exposure is more relevant in terms of quantity. Cross-transmission of resistant strains, which is promoted by inadequate infection control measures, is the second important factor. Finally, the introduction of resistant micro-organisms by the admission of colonized or infected patients contributes to increasing antimicrobial resistance [23]. These factors interact in a given ICU setting since the risk of cross-transmission grows with rising numbers of patients harboring resistant strains [23, 24]. From an ecological point of view any administration of antibiotics is expected to promote the growth of micro-organisms that are intrinsically resistant or have acquired resistance to the applied substances [25]. This has also been suspected for SDD prophylaxis [7, 15, 16].
The selection of MRSA is thought to be one of the greatest risks associated with SDD [7, 26]. In an Austrian ICU the proportion of MRSA rose from 17% to 81% under SDD prophylaxis [27], and a Spanish multicenter trial found significantly more patients colonized by MRSA, even though this was not followed by increased MRSA infection rates [28]. The findings in our study ICU paint a different picture since the MRSA rate remained stable and constantly below the reference ICUs. This agrees with the results of several other studies showing no adverse effects of SDD on methicillin resistance of S. aureus [10, 11, 26]. Two of these trials [10, 11] were performed in an environment with very low MRSA rates, which means that there was also low selection pressure for MRSA. However, in a French ICU with an MRSA frequency of approx. 20% SDD had as well no adverse effects [26]. Early identification and isolation of MRSA-colonized patients were thought to be important mechanisms for keeping the MRSA rate lower than the commonly observed figures in France [26]. This is corroborated by the data of our study ICU, where the MRSA rate remained constantly low with active surveillance and strict isolation measures. Several studies have demonstrated as well the efficacy of surveillance programs in preventing the spread of MRSA [29, 30], which should, in our opinion, be mandatory if SDD is applied to a large proportion of patients such as in our ICU.
The sharp increase in the number of VRE strains observed in the second half of 2004 raises the question of whether it was related to the SDD prophylaxis. However, this hospital-wide outbreak of VRE began in other parts of our hospital 2 months before the first VRE isolate appeared in the study ICU and was comparable to outbreaks reported from two other large hospitals not using SDD in the same region a few months earlier [31]. We cannot exclude that occult VRE colonization was already present in our ICU since systematic surveillance and infection control measures regarding VRE were started thereafter. Therefore SDD could theoretically have exerted antibiotic selection pressure promoting growth of enterococci and thus also of VRE [23, 24]. Indeed, the percentage of Gram-positive and especially of enterococcal isolates in the study ICU was higher than in the reference ICUs not using SDD. In our study only the relative proportions of the bacterial species can be evaluated. The absolute number of isolates cannot be compared between the study ICU and the reference ICUs of SARI due to the study design of SARI, which leaves microbiological sampling to the local examination practices of the participating ICUs [19, 20]. Thus the importance of Gram-positive overgrowth for infection rates in the study ICU remains to be elucidated by another study.
Overgrowth of resistant Gram-negative micro-organisms has also been reported [32], but a causative role of SDD was not identified. In most trials SDD significantly reduced the colonization with aerobic Gram-negative strains [6, 7, 11, 26, 33]. Occasionally, intestinal decontamination was even successful in terminating an outbreak of multiresistant Gram-negative bacilli [34]. This is in keeping with the findings in the study ICU, where the proportion of P. aeruginosa, E. coli, and K. pneumoniae isolates was below the 25th percentile of the reference ICUs. The relatively high percentage of S. marcescens isolates in the study ICU may reflect the intrinsic resistance of this species to colistin. However, this organism is most commonly found in respiratory infections, and the VAP rates in our ICU were below the 25th percentile compared to national reference data.
Aminoglycoside resistance of Enterobacteriaceae in SDD-treated patients has been reported several times [18, 33]. Verwaest and coworkers observed tobramycin-resistant Enterobacteriaceae in 48% of patients receiving SDD vs. 14% in controls [18]. At first glance our findings also suggest an increase in aminoglycoside resistance during SDD use. However, Verwaest et al. [18] and others [26] excluded isolates obtained within the first 48 h after ICU admission from data analysis, stating that SDD should not affect resistance within this period. In contrast, in the present study all isolates were included according to the SARI rules. When our data analysis was limited to isolates from day 3 or later, only one tobramycin-resistant E. coli isolate remained. Thus in agreement with the findings of a comprehensive meta-analysis and also more recent trials [8, 10, 26], SDD had no adverse effect on aminoglycoside resistance of Enterobacteriaceae in our study. One potentially important reason for the different findings is the high rate of baseline aminoglycoside resistance in the Belgian ICU described by Verwaest and coworkers [18, 23, 24].
Emergence of resistance to β-lactams or quinolones is of concern if these substances are used as the systemic component of SDD. Approx. 90% of the patients received one of these agents in the first days after admission. As illustrated in Fig. 3, the resistance to these substances in our ICU tended to be lower than in national reference data, suggesting that the SDD regimen neither directly nor indirectly contributed to the emergence of antibiotic resistance to β-lactams or quinolones. This is in agreement with the findings of others [26, 33, 35] who observed no effect of SDD on β-lactam resistance. Furthermore, we did not use SDD in patients who were expected to stay less than 48 h in the ICU, resulting in an overall proportion of 26% of patients receiving SDD. The restriction to patients expected to derive most benefit from SDD [10, 36] certainly kept the risk of unnecessary selection pressure low in our ICU population.
Finally the limitations of the present study design should be borne in mind. Since our aim was to assess the effects of routine SDD use in a complete ICU patient population, it was not possible to establish a classical control group in the study ICU. On the other hand, the data from the national surveillance project SARI provide a yardstick against which to judge the findings during SDD use [19, 20, 22]. However, the SARI design does not prescribe standardized microbiological sampling, and therefore the comparison is limited to relative proportions of bacterial species. Furthermore, since strict surveillance and infection control measures were a mandatory part of our SDD program we cannot know, if the control of resistance is due to SDD, our search and destroy policy regarding MRSA, or a combination of these.
In conclusion, the findings of this 5-year observation confirm that SDD prophylaxis for mechanically ventilated patients can be safely used with regard to antimicrobial resistance. This should be seen in light of the special circumstances in our ICU. Firstly, the baseline level of resistance against the applied antibiotics was low. Secondly, for prompt recognition of changes in this baseline level antimicrobial resistance was continuously monitored within the SARI project. Finally, strict surveillance and isolation measures were implemented for MRSA. The importance of the increased proportion of enterococci and CNS remains to be evaluated in future studies.
References
Vincent J-L, Jacobs F (2003) Infection in critically ill patients: clinical impact and management. Curr Opin Infect Dis 16:309–313
Fagon JY, Chastre J, Hance AJ, Montravers P, Novara A, Gibert C (1993) Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. Am J Med 94:281–288
Heyland DK, Cook DJ, Griffith L, Keenan SP, Bun-Buisson C, Canadian Critical Trials Group (1999) The attributable morbidity and mortality of ventilator-associated pneumonia in the critically ill patient. Am J Respir Crit Care Med 159:1249–1256
Gastinne H, Wolff M, Delatour F, Faurisson F, Chevret S (1992) A controlled trial in intensive care units of selective decontamination of the digestive tract with nonabsorbable antibiotics. N Engl J Med 326:594–599
Stoutenbeek CP, van Saene HKF, Miranda DR, Miranda DR, Zandstra DF (1984) The effect of selective decontamination and infection rate in multiple trauma patients. Intensive Care Med 10:185–192
Unertl K, Ruckdeschel G, Selbmann HK, Forst H, Lenhart FP, Peter K (1987) Prevention of colonization and respiratory infections in long-term prophylaxis. Intensive Care Med 13:106–113
Bonten MJM, Kullberg BJ, van Dalen R, Girbes ARJ, Hoepelman IM, Hustinx W, van der Meer JWM, Speelman P, Stobberingh EE, Verbrugh HA, Verhoef J, Zwaveling JH and consultants of the Dutch Working group on Antibiotic Policy (2000) Selective digestive decontamination in patients in intensive care. J Antimicrob Chemother 46:351–362
Nathens AB, Marshall JC (1999) Selective decontamination of the digestive tract in surgical patients. A systemic review of the evidence. Arch Surg 134:170–176
D'Amico R, Pifferi S, Leonetti C, Torri V, Tinazzi A, Liberati A (1998) Effectiveness of antibiotic prophylaxis in critically ill adult patients: systemic review of randomised controlled trials. BMJ 316:1275–1285
Krueger WA, Lenhart FP, Neeser G, Ruckdeschel G, Schreckhase H, Eissner HJ, Forst H, Eckart J, Peter K, Unertl KE (2002) Influence of combined intravenous and topical antibiotic prophylaxis on the incidence of infections, organ dysfunctions, and mortality in critically ill surgical patients: a prospective, stratified, randomized, double-blind, placebo-controlled clinical trial. Am J Respir Crit Care Med 166:1029–1037
De Jonge E, Schultz MJ, Spanjaard L, Bossuyt PMM, Vroom MB, Dankert J, Kesecioglu J (2003) Effects of selective decontamination of digestive tract on mortality and acquisition of resistant bacteria in intensive care: a randomised controlled trial. Lancet 362:1011–1016
De La Cal MA, Cerda E, Gardi-Hierro P, van Saene HK, Gomez Santos D, Negro E, Lorente JA (2005) Survival benefit in critically ill burned patients receiving selective decontamination of the digestive tract: a randomized, placebo-controlled, double-blind trial. Ann Surg 241:424–430
De Jonge (2005) Effects of selective decontamination of digestive tract on mortality and antibiotic resistance in the intensive-care unit. Curr Opinion Crit Care 11:144–149
Van Saene HKF, Petros AJ, Ramsay Gl, Baxby D (2003) All great truths are iconoclastic: selective decontamination of the digestive tract moves from heresy to level 1 truth. Intensive Care Med 29:677–690
Kollef MH (2003) Selective digestive decontamination should not be routinely employed. Chest 123:464S–468S
Kollef MH, Micek ST (2005) Strategies to prevent antimicrobial resistance in the intensive care unit. Crit Care Med 33:1845–1853
Nasia S, Adnan S, Luey MR (2004) The role of selective digestive decontamination for reducing infection in patients undergoing liver transplantation: a systematic review and meta-analysis. Liver Transpl 10:817–827
Verwaest C, Verhaegen J, Ferdinande P, Schetz M, Van den Berghe G, Verbist L, Lauwers P (1997) Randomized, controlled trial of selective digestive decontamination in 600 mechanically ventilated patients in a multidisciplinary intensive care unit. Crit Care Med 25:63–71
Meyer E, Schwab F, Jonas D, Rueden H, Gastmeier P, Daschner FD (2004) Surveillance of antimicrobial use and antimicrobial resistance in intensive care units (SARI). I. Antimicrobial use in German intensive care units. Intensive Care Med 30:1089–1096
Meyer E, Jonas D, Schwab F, Rueden H, Gastmeier P, Daschner FD (2003) Design of a surveillance system of antibiotic use and bacterial resistance in German intensive care units (SARI). Infection 31:208–215
National Committee for Clinical Laboratory Standards (2000) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard, 5th edn. NCCLS document M7-A5, Wayne, Pa., USA
Geffers C, Koch J, Sohr D, Nassauer A, Daschner F, Rueden H, Gastmeier P (2000) Aufbau einer Referenzdatenbank für die Surveillance nosokomialer Infektionen auf Intensivstationen. Erste Ergebnisse des nationalen Krankenhaus-Infektions-Surveillance-Systems (KISS). Anaesthesist 49:732–737
Bonten MJM, Slaughter S, Ambergen AW, Haydn MK, van Voorhis J, Nathan C, Weinstein RA (1998) The role of colonisation pressure in the spread of vancomycin-resistant enterococci. An important infection control variable. Arch Intern Med 158:1127–1132
Bonten MJM, Austin DJ, Lipsitch M (2001) Understanding the spread of antibiotic-resistant pathogens in hospitals: mathematical models as tools for infection control. Clin Infect Dis 33:1739–1746
Kollef MK, Fraser VJ (2001) Antibiotic resistance in the intensive care unit. Ann Intern Med 134:298–314
Leone M, Albanese J, Antonini F, Nguyen-Michel A, Martin C (2003) Long-term (6-year) effect of selective digestive decontamination on antimicrobial resistance in intensive care, multiple-trauma patients. Crit Care Med 31:2090–2095
Lingnau W, Berger J, Javorsky F, Fille M, Allerberger F, Benzer H (1998) changing bacterial ecology during a five year period of selective intestinal decontamination. J Hosp Infect 39:195–206
Sánchez García M, Cambronero Galache JA, Lopez Diaz J, Cerda Cerda E, Rubio Balsco J, Gomez Aguinaga MA, Nunez Reiz A, Rogero Marin S, Onoro Canaveral JJ, Sacristan del Castillo JA (1998) Effectiveness and cost of selective decontamination of the digestive tract in critically ill intubated patients. Am J Respir Crit Care Med 158:908–916
Muto CA, Jernigan JA, Ostrowsky BE, Richet HM, Jarvis HM, Boyce JM, Farr BM (2003) SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus. Infect Control Hosp Epidemiol 24:362–386
Farr BM (2004) Prevention and control of methicillin-resistant Staphylococcus aureus infections. Curr Opin Infect Dis 17:317–322
Anonymous (2005) Zum gehäuften Auftreten von glycopeptidresistenten Enterococcus faecium in südwestdeutschen Krankenhäusern. Epidemiol Bull 17:150–155
Hammond PJ, Potgieter PD (1995) Longterm effects of selective decontamination on antimicrobial resistance. Crit Care Med 23:637–645
Saunders GL, Hammond JM, Potgieter PD, Plumb HA, Forder AA (1994) Microbiological surveillance during selective decontamination of the digestive tract (SDD). J Antimicrob Chemother 34:529–544
Brun-Buisson C, Legrand P, Rauss A, Richard C, Montravers F, Beses M, Meakins JL, Soussy CJ, Lemaire F (1989) Intestinal decontamination for control of nosocomial multiresistant Gram-negative bacilli. Study of an outbreak in an intensive care unit. Ann Intern Med 110:873–881
Krueger WA, Unertl KE (2002) Selective decontamination of the digestive tract. Curr Opin Crit Care 8:139–144
Bonten MJ, Krueger WA (2006) Selective decontamination of the digestive tract: cumulating evidence, at last? Semin Respir Crit Care Med 27:18–22
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heininger, A., Meyer, E., Schwab, F. et al. Effects of long-term routine use of selective digestive decontamination on antimicrobial resistance. Intensive Care Med 32, 1569–1576 (2006). https://doi.org/10.1007/s00134-006-0304-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0304-5