Abstract
Aims/Hypothesis
Gamma-glutamyltransferase (GGT) is located on the external surface of most cells and mediates the uptake of gluthathione, an important component of intracellular antioxidant defenses. An increase in GGT concentration has been regarded as a marker of alcohol consumption or liver disease. However, more subtle gradations in GGT could be informative because its expression is enhanced by oxidative stress and it could be released by several conditions inducing cellular stress. Recently, serum GGT concentrations have been associated with many cardiovascular disease risk factors or components of the insulin resistance syndrome. We did a prospective study with the hypothesis that serum GGT is a predictor of incident diabetes.
Methods
A total of 4,088 healthy men working in a steel manufacturing company were examined in 1994 and 1998. Diabetes was defined as a serum fasting glucose concentration of more than 126 mg/dl or the use of diabetes medication.
Results
There was a strong dose-response relation between serum GGT concentrations at baseline and the incidence of diabetes. In contrast to the 31% of men with GGT concentrations under 9 U/l, adjusted relative risks for incidence of diabetes for GGT concentrations 10–19, 20–29, 30–39, 40–49, and over 50 U/l were 8.0, 13.3, 12.6, 19.6 and 25.8, respectively. The associations of age and BMI with incident diabetes became stronger the higher the value of baseline serum GGT concentration.
Conclusion/Interpretation
This study suggests that an increase in GGT concentration within its physiological range is a sensitive and early biomarker for the development of diabetes.
Similar content being viewed by others
Although gamma-glutamyltransferase (GGT) has been widely used as a marker of alcohol consumption or liver disease [1], several population studies [2, 3, 4] have shown a strong cross-sectional association between serum GGT concentrations and many cardiovascular disease risk factors or components of insulin resistance syndrome, including age, obesity, smoking, lack of exercise, blood pressure (BP), dyslipidaemia, and diabetes mellitus, irrespective of alcohol consumption. In addition, in prospective studies [5, 6, 7, 8, 9], baseline serum GGT concentration has been an independent risk factor for the development of cardiovascular or cerebrovascular diseases.
Gamma glutamyltransferase has a pivotal role in the maintenance of intracellular antioxidant defenses through its mediation of extracellular glutathione (GSH) transport into most types of cells [10, 11, 12]. Oxidative stress is associated with a number of pathological conditions, such as inflammation, carcinogenesis, aging, atherosclerosis, and reperfusion injury [13]. Oxidative stress can also play a role in the cause and pathophysiology of diabetes. Most studies [14, 15] focus on the role of oxidative stress in developing cardiovascular complications in diabetic patients, but some studies [16, 17] have suggested that oxidative stress could be involved in the development of Type 1 or Type 2 diabetes.
We did a prospective study to test the hypothesis that GGT, possibly as a marker of oxidative stress, is a predictor of incident diabetes. Given known relations among hypertension, insulin resistance, and diabetes, this hypothesis is partly motivated by our previous work showing that serum GGT concentration is associated with hypertension, especially among alcohol drinkers [18]. In addition, since oxidative stress increases with age and adiposity [19, 20], we analysed whether the relations between age, obesity and diabetes were modified by the baseline GGT concentration.
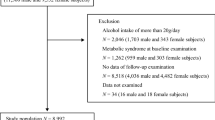
The data analysed were from periodic worksite health examinations at one large steel company in Korea. Throughout 1994, a health check-up was done between 9:00 a.m. and noon in a health care center located in the factory. Male workers between 25 and 55 years of age without diabetes mellitus (defined as fasting serum glucose ≥126 mg/dl and/or taking diabetes medication) were eligible for follow-up in this study. Of the 6,087 men who met these criteria, 4,280 men (70.3 percent follow-up rate) were re-examined in 1998. In addition, 36 reporting definite liver diseases (for example, chronic active hepatitis or liver cirrhosis) and 156 with incomplete or inconsistent information were excluded. After these exclusions, 4,088 men were included in the analysis. Because not all departments in the steel company offered screening for fasting serum glucose, this sample is about half of those included in our study on hypertension [18]. No specific informed consent for this study was obtained. Data are analyzed pursuant to the Korean health regulation pertaining to factories, which states that the factory physician has an obligation to analyse health examination data to educate workers.
FormalPara MeasurementsInformation on lifestyle factors including alcohol consumption, cigarette smoking, exercise, medical history, and family history of diabetes mellitus were obtained primarily by self-reported questionnaires. Venous blood samples were obtained from an antecubital vein after a 12-h overnight fast. Serum GGT, alanine aminotransferase (ALT), and aspartate aminotransferase (AST) concentrations were measured at 37° with an automatic analyser (normal range 0–50 U/l, Hitachi 7170. Japan) and serum glucose was measured by the glucose oxidase method. The serum samples were kept at 4° and analysed within 48 h.
FormalPara Statistical analysisIn this study, the diagnosis of incident diabetes was based on the updated American Diabetes Association criteria (serum fasting glucose concentration ≥126 mg/dl or taking diabetes medication). Although no specific information was obtained about whether the diabetes was Type 1 or Type 2, based on the age distribution, it is likely that the great majority of incident cases are Type 2. The relation between the risk of incident diabetes during 4 years and six categories of baseline GGT level (0–9; 10–19; 20–29; 30–39; 40–49; ≥50 U/l) was analysed using multiple logistic regression analysis. Covariates were the baseline values of age (years), BMI(kg/m2), cigarette smoking (pack years), alcohol consumption (gram/week), exercise (frequency/week), family history of diabetes (dichotomy), and fasting serum glucose (mg/dl). Subgroup analyses included the association of GGT with incident diabetes within nondrinkers, normal weight subjects (BMI <25 kg/m2), and subjects with normal ALT (<35 U/l). The relation among age (25–34; 35–44; 45–55 years), BMI (16–22.9; 23–26.9; 27–32 kg/m2) and incident diabetes were examined within three categories of GGT (0–19; 20–39; ≥40 U/l) by linear and logistic regression analyses. The SAS statistical program, version 8.0, was used in all analyses, the p values quoted are two-sided, and a p value of less than 0.05 were regarded as statistically significant.
Results
Baseline characteristics by GGT
At baseline, there were clear positive or negative dose-response relations with serum GGT concentration among all listed variables except family history of diabetes (Table 1).
GGT and incidence of diabetes
During the 4-year period, 2.0% (83 of the 4,088 workers) received a diagnosis of diabetes. In comparison with the group whose GGT concentration was less than 9 U/l, the adjusted relative risks for incident diabetes among those with GGT concentrations of 10–19, 20–29, 30–39, 40–49, and over 50 U/l were 8.0, 13.3, 12.6, 19.6, and 25.8, respectively (Table 2). The dose-response association was apparent in non-drinkers, drinkers, non-overweight participants (those with BMI <25 kg/m2, and even in lean persons with BMI <23 kg/m2), and subjects with normal values of ALT. On the other hand, the relation between the amount of alcohol consumption and incident diabetes was U-shaped [incidence rate (incident cases of diabetes/number at risk): 2.7% for nondrinkers (23/839), 1.8% for drinkers of 1–90 g per week (33/1826), 1.5% for drinkers of 91–180 g per week (11/744), 2.2% for drinkers of 181–360 g per week (11/508), and 3.6% for drinkers of >360 g per week (5/138), p for quadratic fit =0.06], and therefore not consistent with alcohol overuse as the only explanation of the association of GGT with incident diabetes. ALT itself also showed a dose-response relation with incident diabetes, however, it was weaker than the gradient for GGT, and most strongly observed in the abnormal range of ALT (Table 2). The trend of incident diabetes with AST was similar with that of ALT.
Interaction between age, BMI and GGT
The association of age with incidence of diabetes varied by baseline GGT concentration, being strongest at the highest GGT concentration (p<0.001 for additive interaction) (Fig. 1). Similarly, the association of BMI with incidence of diabetes was strongest at the highest concentration of GGT (Fig. 2, p<0.001 for additive interaction). These interactions persisted after adjustment for the baseline values of smoking, drinking, exercise, family history, fasting blood glucose, and BMI or age.
Discussion
This study showed a strong, positive, dose-response relation for serum GGT concentrations at baseline, mostly within the normal range, with incidence of diabetes with 4 years of followup. This study also showed that, as hypothesized, the effects of age and BMI for the risk of diabetes were different depending on the baseline GGT concentration. Among those with low normal GGT (68% of participants), the associations of age and BMI with the development of diabetes were small, but, among those with high normal or abnormal GGT (11% of participants), the associations of age and BMI with the development of diabetes were very strong. Another prospective study [7] has also reported a graded association between the concentration of GGT in serum and the risk of Type 2 diabetes.
An increase in concentrations of GGT is conventionally interpreted as a marker of alcohol abuse and/or liver damage [1]; however, neither of these interpretations explains the association of GGT within its normal range with incident diabetes. GGT does not solely reflect alcohol in this cohort, because the association between alcohol consumption and risk of diabetes was U-shaped and differs dramatically from the relation of GGT with diabetes. Furthermore, in this study GGT predicted incident diabetes independently of the amount of alcohol consumed, as well as within nondrinkers. Others [7] have interpreted GGT as a marker for hepatic steatosis and hepatic insulin resistance in the pathogenesis of diabetes. These liver problems do not explain our finding; in our subjects, the dose-response relation between GGT concentration and incidence of diabetes was observed among subjects within the normal range of ALT, which usually increases in cases of hepatic steatosis. The same authors [7] also speculated that visceral fat could play a role in the association of GGT with Type 2 diabetes; however, in our study GGT was predictive of Type 2 diabetes even among lean subjects with a BMI of less than 23, who are likely to have little visceral fat.
In general, serum GGT concentration is closely related with other enzymes more specific to the liver, serum ALT or AST concentration, so we did parallel analyses with ALT and AST to further explore the possible role of liver damage in the association of GGT with diabetes. Within their normal ranges, ALT and AST showed little gradient of risk for diabetes, although there was an increased risk of diabetes when ALT or AST was abnormal. Clinical studies [21, 22] have consistently reported an association between several pathologic liver conditions, such as chronic viral hepatitis, liver cirrhosis, or liver cancer, and Type 2 diabetes. Recently fatty liver with a broad spectrum of pathologic conditions has also been linked to insulin resistance syndrome and/or Type 2 diabetes [23, 24]. Therefore, the relations between an abnormal concentration of ALT or AST and diabetes might reflect a relation between fatty liver and insulin resistance syndrome; but liver damage does not seem to explain the association of GGT with diabetes.
Experimental studies have reported that GGT plays an important role in antioxidant systems [10, 11, 12]. It is an ectoenzyme normally present at the outer side of the cell membrane that has the primary function of maintaining intracellular concentrations of glutathione (GSH), a critical antioxidant defense for the cell. Although GGT has been regarded as a marker of liver diseases, GGT actually shows the highest activity in kidney. The activity of GGT in liver is approximately one-fifth that in kidney, and many organs including pancreas, brain, spinal cord, and male reproductive system, also show GGT activity [25]. Increases in GGT activity can be a response to oxidative stress, facilitating increased transport of GSH precursors into cells. In addition, GGT is leaked into the serum possibly as a result of normal cell turnover and cellular stresses. Several mechanisms for GGT leakage are possible and include increases in oxidative stress, proteolysis, glycosylation, GGT synthesis and endothelial cell damage [26, 27]. Thus, increased serum concentrations of GGT could identify people with a low but persistent increase of oxidative and other cellular stresses.
We speculate on one possibility that might explain the association of GGT with incidence of diabetes. Recent studies [28, 29] clearly indicated that under physiological conditions, especially in the presence of Fe3+ or Cu2+, GGT itself is involved directly in reactive oxygen species (ROS) generation. These increased ROS concentrations could exceed the capacity of the antioxidant system and induce oxidative stress in cells, which might predispose to diabetes. For example, some of the products of the GGT reaction, notably, increased concentrations of cysteinylglycine, could lead to an increase in ROS production. Under these circumstances, GGT could turn into a pro-oxidant.
In conclusion, the results suggest that serum GGT could be a sensitive and early biomarker for development of diabetes and that the well-known associations of age and BMI with diabetes could be modified by serum GGT concentration.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
aspartate aminotransferase
- GGT:
-
gamma-glutamyltransferase
- GSH:
-
glutathione
- ROS:
-
reactive oxygen species
References
Teschke R, Brand A, Strohmeyer G (1977) Induction of hepatic microsomal gamma-glutamyltransferase activity following chronic alcohol consumption. Biochem Biophys Res Commun 75:718–724
Nystrom E, Bengtsson C, Lindstedt G, et al. (1988) Serum gamma-glutamyltransferase in a Swedish female population. Age-related reference intervals; morbidity and prognosis in cases with raised catalytic concentration. Acta Med Scand 224:79–84
Nilssen O, Forde OH, Brenn T, The Tromso Study (1990) Distribution and population determinants of gamma-glutamyltransferase. Am J Epidemiol 132:318–326
Nilssen O, Forde OH (1994) Seven-year longitudinal population study of change in gamma-glutamyltransferase: the Tromso Study. Am J Epidemiol 139:787–792
Wannamethee G, Ebrahim S, Shaper AG (1995) Gamma-glutamyltransferase: determinants and association with mortality from ischemic heart disease and all causes. Am J Epidemiol 142:699–708
Brenner H, Rothenbacher D, Arndt V, Schuberth S, Fraisse E, Fliedner TM (1997) Distribution, determinants, and prognostic value of gamma-glutamyltransferase for all-cause mortality in a cohort of construction workers from southern Germany. Prev Med 26:305–107
Perry IJ, Wannamethee SG, Shaper AG (1998) Prospective study of serum gamma-glutamyltransferase and risk of NIDDM. Diabetes Care 21:732–737
Miura K, Nakagawa H, Nakamura H et al. (1994) Serum gamma-glutamyl transferase level in predicting hypertension among male drinkers. J Hum Hypertens 8:445–449
Jousilahti P, Rastenyte D, Tuomilehto J (2000) Serum gamma-glutamyl transferase, self-reported alcohol drinking, and the risk of stroke. Stroke 31:1851–1855
Kugelman A, Choy HA, Liu R, Shi MM, Gozal E, Forman HJ (1994) Gamma-glutamyl transpeptidase is increased by oxidative stress in rat alveolar L2 epithelial cells. Am J Respir Cell Mol Biol 11:5865–5892
Takahashi Y, Oakes SM, Williams MC, Takahashi S, Miura T, Joyce-Brady M (1997) Nitrogen dioxide exposure activates gamma-glutamyl transferase gene expression in rat lung. Toxicol Appl Pharmacol 143:388–396
Karp DR, Shimooku K, Lipsky PE (2001) Expression of gamma-glutamyl transpeptidase protects ramos B cells from oxidation-induced cell death. J Biol Chem 276:3798–3804
Droge W (2002) Free radicals in the physiological control of cell function. Physiol Rev 82:47–95
Rosen P, Nawroth PP, King G, Moller W, Tritschler HJ, Packer L (2001) The role of oxidative stress in the onset and progression of diabetes and its complications: a summary of a Congress Series sponsored by UNESCO-MCBN, the American Diabetes Association and the German Diabetes Society. Diabetes Metab Res Rev 17: 189–212
Vlassara H, Palace MR (2002) Diabetes and advanced glycation endproducts. J Intern Med 251: 87–101
West IC (2000) Radicals and oxidative stress in diabetes. Diabet Med 17: 171–180
Haluzik M, Nedvidkova J (2000) The role of nitric oxide in the development of streptozotocin-induced diabetes mellitus: experimental and clinical implications. Physiol Res 49 [Suppl 1]: S37–S42
Lee DH, Ha MH, Kim JR, Gross M, Jacobs DR(2002) Gamma-glutamyltransferase, alcohol, and blood pressure: a four year follow-up study. Ann Epidemiol 12: 90–96
Hensley K, Floyd RA (2002) Reactive oxygen species and protein oxidation in aging: a look back, a look ahead. Arch Biochem Biophys 397:377–383
Bakker SJ, IJzerman RG, Teerlink T, Westerhoff HV, Gans RO, Heine RJ (2000) Cytosolic triglycerides and oxidative stress in central obesity: the missing link between excessive atherosclerosis, endothelial dysfunction, and beta-cell failure? Atherosclerosis 148: 17–21
Mehta SH, Brancati FL, Sulkowski MS, Strathdee AS, Szklo M, Thomas DL (2000) Prevalence of type 2 diabetes mellitus among persons with hepatitis C virus infections in the United States. Ann Intern Med 17:595–599
Custro N, Carroccio A, Ganci A et al. (2001) Glycemic homeostasis in chronic viral hepatitis and liver cirrhosis. Diabetes Metab 27: 476–481
Marchesini G, Brizi M, Bianchi G et al. (2001) Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes 50: 1844–1850
Chitturi S, Abeygunasekera S, Farrell GC, et al. (2002) NASH and insulin resistance: Insulin hypersecretion and specific association with the insulin resistance syndrome. Hepatology 35: 373–379
Hanigan MH, Frierson HF (1996) Immnuohistochemical detection of gamma-glutamyl transpeptidase in normal human tissue. J Histochem Cytochem 44:1101–1108
Ikeda Y, Fujii J, Taniguchi N, Meister A (1995) Expression of an active glycosylated human gamma-glutamyl transpeptidase mutant that lacks a membrane anchor domain. Proc Natl Acad Sci USA 92: 126–130
Joyce-Brady M, Jean JC, Hughey RP (2001) Gamma-glutamyltransferase and its isoform mediate an endoplasmic reticulum stress response. J Biol Chem 276: 9468–9477
Stark AA, Russell JJ, Langenbach R, Pagano DA, Zeiger E, Huberman E (1994) Localization of oxidative damage by a glutathione-gamma-glutamyl transpeptidase system in preneoplastic lesions in sections of livers from carcinogen-treated rats. Carcinogenesis 15:343–348
Drozdz R, Parmentier C, Hachad H, Leroy P, Siest G, Wellman M (1998) gamma-Glutamyltransferase dependent generation of reactive oxygen species from a glutathione/transferrin system. Free Radic Biol Med 25:786–792
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, DH., Ha, MH., Kim, JH. et al. Gamma-glutamyltransferase and diabetes—a 4 year follow-up study. Diabetologia 46, 359–364 (2003). https://doi.org/10.1007/s00125-003-1036-5
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-003-1036-5