Abstract
Objective:To examine the knowledge of, counseling about, and use of prior directives among patients with HIV-related disease.
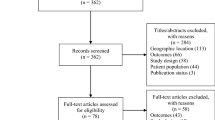
Design:Cross-sectional survey with personal interviews that was part of the evaluation of a multi-site AIDS Health Services Program.
Setting:Outpatient clinics and AIDS community-based organizations.
Patients/participants:To be eligible for the survey, subjects had to be at least 18 years of age and enrolled in the AIDS Health Services Program for at least one month. 1,031 clients were interviewed in nine communities.
Measurements and main results:Of those surveyed, 61% had thought a moderate or great amount about naming a proxy for health care decisions. The majority (68%) of the patients knew about prior directives, yet only 35% had been counseled and only 28% had a prior directive. Of those counseled, physicians had counseled only 11% (38/359). Gay/bisexual men were more likely to have been counseled and to have executed a prior directive than were others. Counseling was associated with having obtained a prior directive. Counseled subjects were 3.5 times more likely to have obtained a prior directive than were those not counseled.
Conclusions:A gap exists between subjects’ knowledge and implementation of prior directives. To help bridge this gap, the authors recommend that physicians not only attend to the technical aspects of patient care, but also determine patient values concerning life-sustaining therapy and counsel patients on prior directives.
Similar content being viewed by others
References
President’s Commision for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Deciding to forego life-sustaining treatment. Washington, DC: U.S. Government Printing Office, 1983.
Guidelines on the termination of life-sustaining treatment and the care of the dying. Bloomington, IN: Indiana University Press, 1987.
Jonsen AR, Siegler M, Winslade WS. Clinical ethics: a practical approach to ethical decisions in clinical medicine. New York: Macmillan Publishing Co, 1982.
Lo B, Steinbrook RL. Deciding whether to resuscitate. Arch Intern Med. 1983;143:1561–3.
Bedell SE, Pelle D, Maher PL, et al. Do-not-resuscitate orders for critically ill patients in the hospital: how are they used and what is their impact? JAMA. 1986;256:232–7.
Schneiderman LJ, Arras JD. Counseling patients to counsel physician on future care in the event of patient incompetence. Ann Intern Med. 1985;102:693–8.
Steinbrook R, Lo B. Decision making for incompetent patients by designated proxy: California’s new law. N Engl J Med. 1984;319:1598–1601.
Lo B, McLeod GA, Saika G. Patient attitudes to discussing life-sustaining treatment. Arch Intern Med. 1986;146:1613–5.
Schmerling RH, Bedell SE, Lilienfeld A, et al. Discussing cardiopulmonary resuscitation: a study of elderly outpatients. J Gen Intern Med. 1988;3:317–21.
Steinbrook R, Lo B, Moulton J, et al. Preferences of homosexual men with AIDS for life-sustaining treatment. N Engl J Med. 1986;314:457–60.
Finucane TE, Shumway JM, Powers RI, et al. Planning with elderly outpatients for contingencies of severe illness: a survey and clinical trial. J Gen Intern Med. 1988;3:322–5.
Steiber SR. Social issues: right to die: public balks at deciding for others. Hospitals. 1987;61:72.
Mor V, Piette J, Fleishman J. Challenges to community case management of persons with AIDS. Health Aff. 1989; Winter: 139–53.
Fleishman JA, Piete JD, Mor V. Organizational response to AIDS. Evaluation and Program Plann. 1990;13:31–8.
Fleishman J, Cwi JS, Mor V. Sampling and accessing people with AIDS: a study of program clients in nine locales. Proceedings of the Fifth Conference of Health Survey Research Methods. Keystone, CO: May, 1989.
Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Q. 1976;54(4):439–67.
Kleinbaum DG, Kupper LL, Morganstein H. Epidemiologic research: principles and quantitative Methods. Belmont, CA: Lifetime Learning Publications, 1982.
SPSS-X User’s Guide. 3-rd ed. Chicago: SPSS Inc., 1988.
Davidson KW, Hackler C, Caradine DR, McCord RS. Physicians’ attitudes on advance directives. JAMA. 1989;262:2415–9.
Klutch M. Survey results after one year’s experience with the Natural Death Act. West J Med. 1978;128:329–30.
Emanuel LL, Emanuel EJ. The medical directive: a new comprehensive advance care document. JAMA. 1989;261:3288–93.
Eisendrath SJ, Jonsen AR. The living will: help or hindrance. JAMA. 1983;249:2054–8.
Buchanan AE, Brock DW. Deciding for others: the ethics of surrogate decision making. Cambridge, MA: Cambridge University Press, 1989.
Wanzer SH, Federmann DD, Adelstein SJ, et al. The physician’s responsibility toward hopelessly ill patients: a second look. N Engl J Med. 1989;320:844–9.
Author information
Authors and Affiliations
Additional information
Supported by National Institute of Aging Post Doctoral Health Care Research Training Grant AG00160 (JT) and supported in part by a grant from the Robert Wood Johnson Foundation.
Rights and permissions
About this article
Cite this article
Teno, J., Fleishman, J., Brock, D.W. et al. The use of formal prior directives among patients with HIV-related diseases. J Gen Intern Med 5, 490–494 (1990). https://doi.org/10.1007/BF02600877
Issue Date:
DOI: https://doi.org/10.1007/BF02600877