Abstract
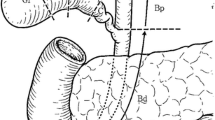
Whether bile spillage during operation presents a risk for peritoneal metastasis in the treatment of bile duct carcinoma was studied in 15 patients (12 with bile duct cancer, 3 with cancer of the papilla of Vater) who had all undergone a pancreatoduodenectomy. Preoperative bile was sampled through a percutaneous transhepatic biliary drainage catheter. Nine patients with bile duct cancer and one with cancer of the papilla of Vater showed positive bile cytology. The operative bile was obtained at the hepatic duct stump after a resection of the tumor-bearing bile duct. The operative bile in 10 patients with positive preoperative bile was found to be positive, while that in the five patients with negative preoperative bile was negative. Thus, the specificity of operative bile was identified as 100%. Moreover, in five patients with preoperative positive bile, saline irrigation of intrahepatic bile duct after a full recovery of hepatic bile revealed cancer cells to remain in the intrahepatic biliary trees. The viability of preoperative bile was 61%–97% with 104–2.4×105 tumor cells, whereas there was a 41%–97% viability with 7.6×104–10.4×105 tumor cells in the operative or irrigated bile. Accordingly, the patients with preoperative positive bile are thus suggested to be at high risk of inducing peritoneal metastasis due to the inadvertent spillage of hepatic bile at the time of resection of a bile duct tumor.
Similar content being viewed by others
References
Hoevels VJ, Lunderquist A, Ihse I (1978) Perkutane transhepatische Intubation der Gallengange zur kombinierten inneren und auseren Drainage bei extrahepatischer Cholestase. Fortschr Roentgenstr 129:533–550
Oleaga JA, Ring EJ, Freiman DB, McLean GK, Rosen RJ (1980) Extension of neoplasm along the tract of a transhepatic tube. AJR 135:841–842
Kim WS, Barth KH, Zinner M (1982) Seeding of pancreatic carcinoma along the transhepatic catheter tract. Radiology 143:427–428
Shorvon PJ, Leung JWC, Corcoran M, Mason RR, Cotton PB (1984) Cutaneous seeding of malignant tumors after insertion of percutaneous prosthesis for obstructive jaundice. Br J Surg 71:694–695
Ferrucci JT, Wittenberg J, Margolies MN, Carey RW (1979) Malignant seeding of the tract after thin-needle aspiration biopsy. Radiology 130:345–346
Drouard F, Delamarre J (1991) Cutaneous seeding of gallbladder cancer after laparoscopic cholecystectomy. N Engl J Med 325:1316
Miller GA, Heaston DK, Moore AV, Millis SR, Dunnick NR (1983) Peritoneal seeding of cholangiocarcinoma in patients with percutaneous biliary drainage. AJR 141:561–562
Anschuetz SL, Vogelzang RL (1986) Malignant pleural effusion: a complication of transhepatic biliary drainage. AJR, 146:1165–1166
Verbeek PCM, van der Hyde, Ramsoekh T, Bosma A (1990) Clinical significance of implantation metastases after surgical treatment of cholangiocarcinoma. Sem in Liver Dis 10:142–144
Nishimura A, Den N, Sato H, Takeda B (1973) Exfoliative cytology of the biliary tract with the use of saline irrigation under choledochoscopic control. Ann Surg 178:594–599
Harell GS, Anderson MFA, Berry PF (1981) Cytologic bile examination in the diagnosis of biliary duct neoplastic strictures. AJR 137:1123–1126
Muro A, Mueller PR, Ferrucci JT, Taft PD (1983) Bile cytology. Radiology 149:846–847
Kurzawinski TR, Deery A, Dooley JS, Dick R, Hobbs KEF, Davidson BR (1993) A prospective study of biliary cytology in 100 patients with bile duct strictures. Hepatology 18:1399–1403
Rabinovitz M, Zajko AB, Hassanein T, Shetty B, Bron KM, Schade RR, Gavaler JS, Block G, Van Thiel DH, Dekker A (1990) Diagnostic value of brush cytology in the diagnosis of bile duct carcinoma: a study in 65 patients with bile duct strictures. Hepatology 12:747–752
Umpleby HC, Fermor B, Symes MO, Williamson RCN (1984) Viability of exfoliated colorectal carcinoma cells. Br J Surg 71:659–663
Fermor B, Umpleby HC, Lever JV, Symes MO, Williamson RCN (1986) Proliferative and metastatic potential of exfoliated colorectal cancer cells. J Natl Cancer Inst 76:347–349
Chapman WC, Sharp KW, Weaver F, Sawyers JL (1989) Tumor seeding from percutaneous biliary catheters. Ann Surg 209:708–715
Hansen E, Wolff N, Knuechel R, Ruschoff J, Hofstaedter F, Taeger K (1995) Tumor cells in blood shed from the surgical field. Arch Surg 130:387–393
Tanaka N, Nobori M, Kohzuma T, Suzuki Y, Saiki S (1994) Anastomotic recurrence at hepaticojejunostomy in a long-term survivor of bile duct carcinoma: report of a case. Surg Today 24:280–284
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tanaka, N., Nobori, M. & Suzuki, Y. Does bile spillage during an operation present a risk for peritoneal metastasis in bile duct carcinoma?. Surg Today 27, 1010–1014 (1997). https://doi.org/10.1007/BF02385780
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02385780