Abstract
Animal studies implicate meningeal lymphatic dysfunction in the pathogenesis of neurodegenerative diseases such as Alzheimer’s disease and Parkinson’s disease (PD). However, there is no direct evidence in humans to support this role1,2,3,4,5. In this study, we used dynamic contrast-enhanced magnetic resonance imaging to assess meningeal lymphatic flow in cognitively normal controls and patients with idiopathic PD (iPD) or atypical Parkinsonian (AP) disorders. We found that patients with iPD exhibited significantly reduced flow through the meningeal lymphatic vessels (mLVs) along the superior sagittal sinus and sigmoid sinus, as well as a notable delay in deep cervical lymph node perfusion, compared to patients with AP. There was no significant difference in the size (cross-sectional area) of mLVs in patients with iPD or AP versus controls. In mice injected with α-synuclein (α-syn) preformed fibrils, we showed that the emergence of α-syn pathology was followed by delayed meningeal lymphatic drainage, loss of tight junctions among meningeal lymphatic endothelial cells and increased inflammation of the meninges. Finally, blocking flow through the mLVs in mice treated with α-syn preformed fibrils increased α-syn pathology and exacerbated motor and memory deficits. These results suggest that meningeal lymphatic drainage dysfunction aggravates α-syn pathology and contributes to the progression of PD.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Source data underlying all figures and tables are provided with this paper. To respect data protection and privacy of the participants, the remaining data, such as raw MRI images, are not publicly available. These data will be shared on request from qualified investigators for noncommercial research purposes within the limits of participants’ consent and are subject to institutional ethics committee approval and material transfer agreements. Requests will be handled by the corresponding author X.J.W. Source data are provided with this paper.
References
Da Mesquita, S. et al. Functional aspects of meningeal lymphatics in ageing and Alzheimer’s disease. Nature 560, 185–191 (2018).
Patel, T. K. et al. Dural lymphatics regulate clearance of extracellular tau from the CNS. Mol. Neurodegener. 14, 11 (2019).
Zou, W. et al. Blocking meningeal lymphatic drainage aggravates Parkinson’s disease-like pathology in mice overexpressing mutated α-synuclein. Transl. Neurodegener. https://doi.org/10.1186/s40035-019-0147-y (2019).
Wang, L. et al. Deep cervical lymph node ligation aggravates AD-like pathology of APP/PS1 mice. Brain Pathol. 29, 176–192 (2019).
Wen, Y.-R., Yang, J.-H., Wang, X. & Yao, Z.-B. Induced dural lymphangiogenesis facilities soluble amyloid-β clearance from brain in a transgenic mouse model of Alzheimer’s disease. Neural Regen. Res. 13, 709–716 (2018).
Galea, I., Bechmann, I. & Perry, V. H. What is immune privilege (not)? Trends Immunol. 28, 12–18 (2007).
Carson, M. J., Doose, J. M., Melchior, B., Schmid, C. D. & Ploix, C. C. CNS immune privilege: hiding in plain sight. Immunol. Rev. 213, 48–65 (2006).
Bower, N. I. & Hogan, B. M. Brain drains: new insights into brain clearance pathways from lymphatic biology. J. Mol. Med. 96, 383–390 (2018).
Louveau, A. et al. Structural and functional features of central nervous system lymphatic vessels. Nature 523, 337–341 (2015).
Antila, S. et al. Development and plasticity of meningeal lymphatic vessels. J. Exp. Med. 214, 3645–3667 (2017).
Ahn, J. H. et al. Meningeal lymphatic vessels at the skull base drain cerebrospinal fluid. Nature 572, 62–66 (2019).
Aspelund, A. et al. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. J. Exp. Med. 212, 991–999 (2015).
Louveau, A. et al. CNS lymphatic drainage and neuroinflammation are regulated by meningeal lymphatic vasculature. Nat. Neurosci. 21, 1380–1391 (2018).
Tarasoff-Conway, J. M. et al. Clearance systems in the brain-implications for Alzheimer disease. Nat. Rev. Neurol. 11, 457–470 (2015).
Da Mesquita, S., Fu, Z. & Kipnis, J. The meningeal lymphatic system: a new player in neurophysiology. Neuron 100, 375–388 (2018).
Coles, J. A., Myburgh, E., Brewer, J. M. & McMenamin, P. G. Where are we? The anatomy of the murine cortical meninges revisited for intravital imaging, immunology, and clearance of waste from the brain. Prog. Neurobiol. 156, 107–148 (2017).
Ma, Q., Ineichen, B. V., Detmar, M. & Proulx, S. T. Outflow of cerebrospinal fluid is predominantly through lymphatic vessels and is reduced in aged mice. Nat. Commun. 8, 1434 (2017).
Bolte, A. C. et al. Meningeal lymphatic dysfunction exacerbates traumatic brain injury pathogenesis. Nat. Commun. 11, 4524 (2020).
Weller, R. O., Djuanda, E., Yow, H. Y. & Carare, R. O. Lymphatic drainage of the brain and the pathophysiology of neurological disease. Acta Neuropathol. 117, 1–14 (2009).
Hu, X. et al. Meningeal lymphatic vessels regulate brain tumor drainage and immunity. Cell Res. 30, 229–243 (2020).
Rasmussen, M. K., Mestre, H. & Nedergaard, M. The glymphatic pathway in neurological disorders. Lancet Neurol. 17, 1016–1024 (2018).
Louveau, A. et al. Understanding the functions and relationships of the glymphatic system and meningeal lymphatics. J. Clin. Invest. 127, 3210–3219 (2017).
Nistal, D. & Mocco, J. Central nervous system lymphatics and impact on neurologic disease. World Neurosurg. 109, 449–450 (2018).
Reeves, B. C. et al. Glymphatic system impairment in Alzheimer’s disease and idiopathic normal pressure hydrocephalus. Trends Mol. Med. 26, 285–295 (2020).
Valenza, M., Facchinetti, R., Steardo, L. & Scuderi, C. Altered waste disposal system in aging and Alzheimer’s disease: focus on astrocytic aquaporin-4. Front. Pharmacol. 10, 1656 (2019).
Kress, B. T. et al. Impairment of paravascular clearance pathways in the aging brain. Ann. Neurol. 76, 845–861 (2014).
Maloveska, M. et al. Dynamics of Evans blue clearance from cerebrospinal fluid into meningeal lymphatic vessels and deep cervical lymph nodes. Neurological Res. 40, 372–380 (2018).
Eide, P. K., Vatnehol, S. A. S., Emblem, K. E. & Ringstad, G. Magnetic resonance imaging provides evidence of glymphatic drainage from human brain to cervical lymph nodes. Sci. Rep. 8, 7194 (2018).
Sun, B. L. et al. Lymphatic drainage system of the brain: a novel target for intervention of neurological diseases. Prog. Neurobiol. 163-164, 118–143 (2018).
Tan, P., Goh, T., Nonomura, H. & Tan, B. Hilar vessels of the submandibular and upper jugular neck lymph nodes: anatomical study for vascularized lymph node transfer to extremity lymphedema. Ann. Plast. Surg. 76, 117–123 (2016).
Bou-Assaly, W. The forgotten lymph nodes: review of the superficial head and neck lymphatic system. J. Radiol. Imaging 1, 9–13 (2016).
Hsu, M. et al. Neuroinflammation-induced lymphangiogenesis near the cribriform plate contributes to drainage of CNS-derived antigens and immune cells. Nat. Commun. 10, 229 (2019).
Van der Perren, A. et al. The structural differences between patient-derived α-synuclein strains dictate characteristics of Parkinson’s disease, multiple system atrophy and dementia with Lewy bodies. Acta neuropathologica https://doi.org/10.1007/s00401-020-02157-3 (2020).
Peelaerts, W., Bousset, L., Baekelandt, V. & Melki, R. ɑ-Synuclein strains and seeding in Parkinson’s disease, incidental Lewy body disease, dementia with Lewy bodies and multiple system atrophy: similarities and differences. Cell Tissue Res. 373, 195–212 (2018).
Shahnawaz, M. et al. Discriminating α-synuclein strains in Parkinson’s disease and multiple system atrophy. Nature 578, 273–277 (2020).
Cromer, W. et al. The effects of inflammatory cytokines on lymphatic endothelial barrier function. Angiogenesis 17, 395–406 (2014).
Dohgu, S. et al. Monomeric α-synuclein induces blood–brain barrier dysfunction through activated brain pericytes releasing inflammatory mediators in vitro. Microvascular Res. 124, 61–66 (2019).
Kuan, W. et al. α-Synuclein pre-formed fibrils impair tight junction protein expression without affecting cerebral endothelial cell function. Exp. Neurol. 285, 72–81 (2016).
RB, P. et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 30, 1591–1601 (2015).
Gilman, S. et al. Second consensus statement on the diagnosis of multiple system atrophy. Neurology 71, 670–676 (2008).
Hoglinger, G. U. et al. Clinical diagnosis of progressive supranuclear palsy: the movement disorder society criteria. Mov. Disord. 32, 853–864 (2017).
Yamada, M. et al. Diagnostic criteria for dementia with Lewy bodies: updates and future directions. J. Mov. Disord. 13, 1–10 (2020).
Armstrong, M. J. et al. Criteria for the diagnosis of corticobasal degeneration. Neurology 80, 496–503 (2013).
Rektor, I., Rektorová, I. & Kubová, D. Vascular parkinsonism—an update. J. Neurol. Sci. 248, 185–191 (2006).
Movement Disorder Society Task Force on Rating Scales for Parkinson’s Disease. The Unified Parkinson’s Disease Rating Scale (UPDRS): status and recommendations. Mov. Disord. 18, 738–750 (2003).
Wenning, G. K. et al. Development and validation of the unified multiple system atrophy rating scale (UMSARS). Mov. Disord. 19, 1391–1402 (2004).
Golbe, L. I. & Ohman-Strickland, P. A. A clinical rating scale for progressive supranuclear palsy. Brain 130, 1552–1565 (2007).
Yoo, J. et al. Timed up and go test and the risk of Parkinson’s disease: a nation-wide retrospective cohort study. Mov. Disord. 35, 1263–1267 (2020).
Lindholm, B., Nilsson, M., Hansson, O. & Hagell, P. External validation of a 3-step falls prediction model in mild Parkinson’s disease. J. Neurol. 263, 2462–2469 (2016).
Seitz, J. et al. Reduction of motion artifacts in magnetic resonance imaging of the neck and cervical spine by long-term averaging. Investigative Radiol. 35, 380–384 (2000).
Tang, H. et al. [Feasibility research of the new fixation device compatible with head and neck coil of MRI for radiotherapy]. Zhongguo yi liao qi xie za zhi [Chin. J. Med. Instrum.] 43, 326–329 (2019).
Greene, D. et al. Behavioral interventions for reducing head motion during MRI scans in children. NeuroImage 171, 234–245 (2018).
Bazin, P. L. et al. Volumetric neuroimage analysis extensions for the MIPAV software package. J. Neurosci. Methods 165, 111–121 (2007).
Ogul, H. Double ophthalmic arteries arising from the internal carotid artery and the accessory meningeal artery: a case report of a new anatomic variation. World Neurosurg. 135, 103–106 (2020).
Ondas, O., Unal, A., Ulusal, S., Guven, F. & Ogul, H. Anomalous origins of ophthalmic arteries on three-dimensional time-of-flight magnetic resonance angiography and their clinical importance. Ophthalmic Res. 63, 341–346 (2020).
Azuma, M. et al. Evaluation of intracranial dural arteriovenous fistulas: comparison of unenhanced 3T 3D time-of-flight MR angiography with digital subtraction angiography. Magn. Reson. Med. Sci. 14, 285–293 (2015).
Ding, X. et al. Propagation of pathological α-synuclein from the urogenital tract to the brain initiates MSA-like syndrome. iScience 23, 101166 (2020).
Wang, X. et al. Autonomic ganglionic injection of α-synuclein fibrils as a model of pure autonomic failure α-synucleinopathy. Nat. Commun. 11, 934 (2020).
Acknowledgements
X.-J.W. was supported by grants from the National Natural Science Foundation of China (no. 81873791, 81471307) and the Natural Science Foundation of Henan Province for Excellent Young Scholars (no. 202300410357). J.-F.T. was supported by grants from the National Natural Science Foundation of China (no. 81671267). B.-S.T. was supported by the National Key Plan for Scientific Research and Development of China (no. 2016YFC1306000). J.-Y.L. was supported by the Swedish Research Council (2019-01551). We thank all our collaborators at the First Affiliated Hospital of Zhengzhou University for their assistance with imaging examinations. Specially, we thank Y. Li for her excellent technical support and we also appreciate Z. Yang and L. Zhou’s assistance with image processing and Euni Wu’s efforts for language editing.
Author information
Authors and Affiliations
Contributions
X.-J.W. conceived and designed the experiments; X.-J.W. coordinated the whole project; X.-B.D., M.-M.M., J.-F.T., Y.F. and X.-X.W. were responsible for the initial assessment and diagnosing of patients; X.-B.D., X.-X.W., Y.F. and H.-Y.T. were responsible for assessing and documenting their patients’ health information. X.-X.W., Y.F., Y.-K.C. and Q.-C.C. performed image analysis. D.-H.X., C.Q., J.-Q.W., Z.X. and H.L. conducted modeling surgery and behavioral tests; D.-H.X., H.L., J.-Q.W. and Z.-X.Z. performed immunostaining; E.W., J.-Y.L., B.-S.T., W.W. and X.-B.D. provided statistical analysis and technical support; X.-J.W., X.-B.D., M.-M.M., X.-X.W. and D.-H.X. participated in final data analysis and interpretation; X.-J.W., D.-H.X., X.-X.W., H.L. and X.-B.D. carried out most of the writing with input from other authors. All authors discussed the results and commented on the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 CONSORT diagram.
Consolidated Standards of Reporting Trials flow diagram showing study participants screening, eligibility and inclusion.
Extended Data Fig. 2 Patients’ demographics and clinical characteristics.
Demographics and characteristics of DLB, CBD and VP groups who performed DCE-MRI of dcLNs. Mean (standard deviation) and N (%) were reported. Demographic factors and clinical characteristics were compared using chi-square test and two-sided Mann-Whitney tests.
Extended Data Fig. 3 Demographics and clinical characteristics of iPD patients.
The demographics and clinical characteristics of I-iPD and II-iPD groups who completed the MRI scans. Mean (standard deviation) and N (%) were reported.
Extended Data Fig. 4 Visualization and measurement of mLVs-SSS and mLVs-SS by high-solution MRI sequences.
a, Visualization of mLVs-SSS in NC (i, v), iPD (ii, vi), MSA (iii, vii) and PSP-RS (iv, viii) groups on 2D T1 black-blood (i-iv) and 3D T2 FLAIR (v-viii) sequences. Visualization of mLVs-SS in NC (ix, xiii), iPD (x, xiv), MSA (xi, xv) and PSP-RS (xii, xvi) groups on 2D T1 black-blood (ix-xii) and 3D T2 FLAIR (xiii-xvi) sequences. The red rectangles represent three mLVs-SSS (L-, R- and Lo-mLVs-SSS) (i-viii) or three mLVs-SS (L-, R- and Lo-mLVs-SS) (ix-xvi), L-, R- and Lo-mLVs-SSS represent the left, right and lower mLVs-SSS, respectively; L-, R- and Lo-mLVs-SS represent the left, right and lower mLVs-SS, respectively. Scale bar, 1 cm. b, Measurement and comparison of the average cross-sectional areas of mLVs-SSS (i) in NC (n = 73), iPD (n = 61), MSA (n = 18) and PSP-RS (n = 19) groups, or mLVs-SS (ii) in NC (n = 47), iPD (n = 46), MSA (n = 18) and PSP-RS (n = 17) groups on 2D T1 black-blood, 3D T1 black-blood and 3D T2 FLAIR sequences (one-way ANOVA with Tukey’s multiple comparison correction, Supplementary Table 3). Measurement and comparison of the average cross-sectional areas of mLVs-SSS (iii) in NC (n = 73), I-iPD (n = 31) and II-iPD (n = 30) groups, or mLVs-SS (iv) in NC (n = 47), I-iPD (n = 23) and II-iPD (n = 23) groups on 2D T1 black-blood, 3D T1 black-blood and 3D T2 FLAIR sequences (one-way ANOVA with Tukey’s multiple comparison correction, Supplementary Table 4). I-iPD group, H&Y stage ≤ 2.5; II-iPD group, H&Y stage > 2.5. c, Correlations between the modified H&Y staging scale scores and the average cross-sectional areas of mLVs-SSS (i-iii) (n = 61) or mLVs-SS (iv-vi) (n = 46) in iPD patients on 2D T1 black-blood (i, iv), 3D T1 black-blood (ii, v) and 3D T2 FLAIR (iii, vi) sequences (two-sided Spearman correlation analysis, Supplementary Table 6). All box-and-whisker plots depict the median, quartiles and range.
Extended Data Fig. 5 The DCE-MRI parameters of dcLNs in NC, DLB, CBD and VP groups.
Comparison of the average TTP values (a), average wash-in rate values (b) and average AUC values (c) of bilateral dcLNs in NC (n = 95), DLB (n = 8), CBD (n = 4) and VP (n = 19) groups (Kruskal–Wallis test with Dunn’s multiple comparison test). All box-and-whisker plots depict the median, quartiles and range.
Extended Data Fig. 6 Diagnostic accuracy of the DCE-MRI parameters for distinguishing iPD from AP.
The sensitivity, specificity, threshold, AUROC and 95% CI of the AUROC, sensitivity and specificity were calculated by ROC curve.
Extended Data Fig. 7 Diagnostic accuracy of the DCE-MRI parameters for distinguishing I-iPD from AP.
The sensitivity, specificity, threshold, AUROC and 95% CI of the AUROC, sensitivity and specificity were calculated by ROC curve.
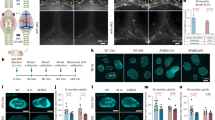
Extended Data Fig. 8 PD-like pathology induced by intrastriatal inoculation of α-syn PFFs in mice.
a, Representative transmission electron micrographs of mouse α-syn PFFs before (i) and after (ii) sonication (repeated three times). Scale bar, 100 nm. iii, Distribution of sonicated mouse α-syn PFFs lengths after 500 measurements. b, Representative immunohistochemical results of different segments from α-syn PFFs- (i-iii, v-vii, ix-xi, xiii-xv) and PBS- (iv, viii, xii, xvi) injected mice. Representative images displayed the distribution of pα-syn in the cortex (i-iv), striatum (v-viii), amygdala (ix-xii) and substantia nigra (xiii-xvi) at 1 mpi (i, v, ix, xiii), 3 mpi (ii, vi, x, xiv) and 6 mpi (iii, vii, xi, xv), but not in PBS-injected mice at 6 mpi (iv, viii, xii, xvi). Scale bar, 20 μm. xvii-xx, Quantification of pα-syn immunoreactivity of cortex (xvii), striatum (xviii), amygdala (xix), and substantia nigra (xx) from α-syn PFFs-injected mice at 1, 3 and 6 mpi and PBS-injected mice at 6 mpi; two-sided Student’s t-test. n = 6 mice/age/group. c, Representative immunoblot images of total α-syn (i, ii) or pS129 α-syn (iii, iv) in the soluble (i, iii) and insoluble (ii, iv) fractions of cortex of PBS- and α-syn PFFs-injected mice and quantification (v, vi); two-sided Mann–Whitney test. n = 6 mice/group. The loading controls (GAPDH) were run on different gels in the same experiment. All box-and-whisker plots depict the median, quartiles and range.
Extended Data Fig. 9 Ligation of the bilateral afferent lymphatics exacerbated PD-like pathology and motor deficits in ligated α-syn PFFs-injected mice.
a, b, Representative images of LYVE-1-positive (green) vessels in the meninges of sham-operated (a1) and ligated (a2) mice and the quantification of diameters (b); two-sided Student’s t-test. n = 6 mice/group. Scale bar, 2 mm. c, d, Representative images of EB (red) draining into the dcLNs (c1-c3, sham-operated; d1-d3, ligated) one hour after injection, stained with LYVE-1 (green) and Hoechst 33258 (blue). Scale bar, 200 µm. e, Quantification of EB percentage area by area in dcLNs of sham-operated and ligated mice; two-sided Mann-Whitney test. n = 6 mice/group. f-i, Representative immunohistochemical results of different segments from ligated α-syn PFFs-injected mice (f1-f3, g1-g3, h1-h3, i1-i3) and ligated PBS-injected mice (f4, g4, h4, i4). The images displayed the distribution of pα-syn in cortex (f1-f3), striatum (g1-g3), amygdala (h1-h3) and substantia nigra (i1-i3) at 1 mpi (f1, g1, h1, i1), 3 mpi (f2, g2, h2, i2) and 6 mpi (f3, g3, h3, i3), but not in ligated PBS-injected mice at 6 mpi (f4, g4, h4, i4). Scale bar, 20 µm. j-m, Quantification of pα-syn immunoreactivity of the cortex (j), striatum (k), amygdala (l) and substantia nigra (m) in non-ligated α-syn PFFs-injected and ligated α-syn PFFs-injected mice (n = 6 mice/age/group); two-sided Student’s t-test. n-p, Representative immunoblot images (n) of total (up) and pS129 (down) α-syn in soluble (left) and insoluble (right) fractions of cortex of non-ligated α-syn PFFs-injected and ligated α-syn PFFs-injected mice and quantification (o, p); two-sided Mann-Whitney test. n = 6 mice/group. The loading controls (GAPDH) were run on different gels in the same experiment. All box-and-whisker plots depict the median, quartiles and range.
Extended Data Fig. 10 Quantitative assessments of MMA, SSS and ECA flow by DCE-MRI.
a, Representative DCE-MRI scans of MMA (i, ii, vii, viii), SSS (iii, iv, ix, x) and ECA (v, vi, xi, xii) before (i-vi) and after (vii-xii) administration of gadobutrol in NC (i, iii, v, vii, ix, xi) and iPD (ii, iv, vi, viii, x, xii) groups. The red ellipses represent MMA (i, ii, vii, viii), SSS (iii, iv, ix, x) and ECA (v, vi, xi, xii), respectively. Scale bar, 2 cm. b, Representative TICs of MMA (i, iv), SSS (ii, v) and ECA (iii, vi) of NC (i-iii) and iPD groups (iv-vi) obtained by DCE-MRI. L-MMA and R-MMA represent the left and right MMA, respectively. L-ECA and R-ECA represent the left and right ECA, respectively. c, Comparison of the average TTP values (i), average wash-in rate values (iv) and average AUC values (vii) of bilateral MMA in NC (n = 39), iPD (n = 24), MSA (n = 17) and PSP-RS (n = 17) groups (Kruskal–Wallis test with Dunn’s multiple comparison test). Comparison of the TTP values (ii), wash-in rate values (v) and AUC values (viii) of SSS in NC (n = 38), iPD (n = 24), MSA (n = 17) and PSP-RS (n = 18) groups (Kruskal–Wallis test with Dunn’s multiple comparison test). Comparison of the average TTP values (iii), average wash-in rate values (vi) and average AUC values (ix) of bilateral ECA in NC (n = 40), iPD (n = 24), MSA (n = 17) and PSP-RS (n = 18) groups (Kruskal–Wallis test with Dunn’s multiple comparison test). All box-and-whisker plots depict the median, quartiles and range.
Supplementary information
Supplementary Information
Supplementary Figs. 1 and 2 and Supplementary Tables 1–8.
Supplementary Video 1
3D reconstruction of mLVs (red) in a healthy participant from subtracted T1 black-blood images (horizontal view, 360°). The mLVs run alongside the venous sinus, especially the SSS and SS.
Supplementary Video 2
3D reconstruction of mLVs (red) in an iPD patient from subtracted T1 black-blood images (horizontal view, 360°). The mLVs run alongside the venous sinus, especially the SSS and SS.
Source data
Source Data Fig. 1
Statistical Source Data.
Source Data Fig. 2
Statistical Source Data.
Source Data Fig. 3
Statistical Source Data and unprocessed western blots.
Source Data Extended Data Fig. 2
Statistical Source Data.
Source Data Extended Data Fig. 3
Statistical Source Data.
Source Data Extended Data Fig. 4
Statistical Source Data.
Source Data Extended Data Fig. 5
Statistical Source Data.
Source Data Extended Data Fig. 6
Statistical Source Data.
Source Data Extended Data Fig. 7
Statistical Source Data.
Source Data Extended Data Fig. 8
Statistical Source Data and unprocessed western blots.
Source Data Extended Data Fig. 9
Statistical Source Data and unprocessed western blots.
Source Data Extended Data Fig. 10
Statistical Source Data.
Rights and permissions
About this article
Cite this article
Ding, XB., Wang, XX., Xia, DH. et al. Impaired meningeal lymphatic drainage in patients with idiopathic Parkinson’s disease. Nat Med 27, 411–418 (2021). https://doi.org/10.1038/s41591-020-01198-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-01198-1
This article is cited by
-
Enhanced meningeal lymphatic drainage ameliorates lipopolysaccharide-induced brain injury in aged mice
Journal of Neuroinflammation (2024)
-
Dynamic changes in glymphatic function in reversible cerebral vasoconstriction syndrome
The Journal of Headache and Pain (2024)
-
A deeper dive into amyloid clearance by meningeal lymphatic vessels
Nature Cardiovascular Research (2024)
-
Altered perivascular spaces in subcortical white matter in Parkinson’s disease patients with levodopa-induced dyskinesia
npj Parkinson's Disease (2024)
-
Advancing insights into in vivo meningeal lymphatic vessels with stereoscopic wide-field photoacoustic microscopy
Light: Science & Applications (2024)