Abstract
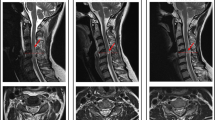
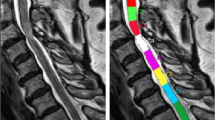
Pathophysiological changes in the spinal cord white and grey matter resulting from injury can be observed with MRI techniques. These techniques provide sensitive markers of macrostructural and microstructural tissue integrity, which correlate with histological findings. Spinal cord MRI findings in traumatic spinal cord injury (tSCI) and nontraumatic spinal cord injury — the most common form of which is degenerative cervical myelopathy (DCM) — have provided important insights into the pathophysiological processes taking place not just at the focal injury site but also rostral and caudal to the spinal injury. Although tSCI and DCM have different aetiologies, they show similar degrees of spinal cord pathology remote from the injury site, suggesting the involvement of similar secondary degenerative mechanisms. Advanced quantitative MRI protocols that are sensitive to spinal cord pathology have the potential to improve diagnosis and, more importantly, predict outcomes in patients with tSCI or nontraumatic spinal cord injury. This Review describes the insights into tSCI and DCM that have been revealed by neuroimaging and outlines current activities and future directions for the field.
Key points
-
Traumatic spinal cord injury (tSCI) and (nontraumatic) degenerative cervical myelopathy (DCM) have different aetiologies but lead to similar secondary degenerative changes in the spinal cord.
-
Advanced MRI techniques have been used to improve the sensitivity and specificity with which spinal degenerative changes can be detected.
-
Diffusion tensor imaging (DTI) is an advanced MRI technique that characterizes tissue microstructure by measuring the water diffusion profile of the tissue.
-
In tSCI and DCM, DTI has been used to identify changes in microstructure above and below the lesion or stenosis that are not visible with conventional MRI.
-
Spinal cord DTI metrics correlate with neurological and electrophysiological outcomes after tSCI and DCM.
-
Further advances in data acquisition, processing and modelling are needed to improve the reliability and specificity of quantitative MRI metrics as predictors of patient outcome.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Ahuja, C. S. et al. Traumatic spinal cord injury. Nat. Rev. Dis. Primers 3, 17018 (2017).
Kato, S. & Fehlings, M. Degenerative cervical myelopathy. Curr. Rev. Musculoskelet. Med. 9, 263–271 (2016).
Akter, F. & Kotter, M. Pathobiology of degenerative cervical myelopathy. Neurosurg. Clin. N. Am. 29, 13–19 (2018).
Buss, A. et al. Gradual loss of myelin and formation of an astrocytic scar during Wallerian degeneration in the human spinal cord. Brain 127, 34–44 (2004).
Fehlings, M. G. et al. A clinical practice guideline for the management of patients with degenerative cervical myelopathy: recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression. Glob. Spine J. 7, 70S–83S (2017).
Fehlings, M. G. et al. A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on the role of baseline magnetic resonance imaging in clinical decision making and outcome prediction. Glob. Spine J. 7, 221S–230S (2017).
Prados, F. et al. Spinal cord grey matter segmentation challenge. Neuroimage 152, 312–329 (2017).
Martin, A. R. et al. Translating state-of-the-art spinal cord MRI techniques to clinical use: a systematic review of clinical studies utilizing DTI, MT, MWF, MRS, and fMRI. NeuroImage. Clin. 10, 192–238 (2016).
Basser, P. J., Mattiello, J. & LeBihan, D. Estimation of the effective self-diffusion tensor from the NMR spin echo. J. Magn. Reson. 103, 247–254 (1994).
Pierpaoli, C., Jezzard, P., Basser, P. J., Barnett, A. & Di Chiro, G. Diffusion tensor MR imaging of the human brain. Radiology 201, 637–648 (1996).
Beaulieu, C. & Allen, P. S. Determinants of anisotropic water diffusion in nerves. Magn. Reson. Med. 31, 394–400 (1994).
Wheeler-Kingshott, C. A. et al. The current state-of-the-art of spinal cord imaging: applications. Neuroimage 84, 1082–1093 (2014).
Grabher, P., Mohammadi, S., David, G. & Freund, P. Neurodegeneration in the spinal ventral horn prior to motor impairment in cervical spondylotic myelopathy. J. Neurotrauma 34, 2329–2334 (2017).
Allen, A. R. Remarks on the histopathological changes in the spinal cord due to impact: an experimental study. J. Nerv. Ment. Dis. 41, 141–147 (1914).
Dusart, I. & Schwab, M. E. Secondary cell death and the inflammatory reaction after dorsal hemisection of the rat spinal cord. Eur. J. Neurosci. 6, 712–724 (1994).
Karadimas, S. K. et al. A novel experimental model of cervical spondylotic myelopathy (CSM) to facilitate translational research. Neurobiol. Dis. 54, 43–58 (2013).
Dhillon, R. S. et al. Axonal plasticity underpins the functional recovery following surgical decompression in a rat model of cervical spondylotic myelopathy. Acta Neuropathol. Commun. 4, 89 (2016).
Karadimas, S. K. et al. Riluzole blocks perioperative ischemia-reperfusion injury and enhances postdecompression outcomes in cervical spondylotic myelopathy. Sci. Transl Med. 7, 316ra194 (2015).
Ohshio, I., Hatayama, A., Kaneda, K., Takahara, M. & Nagashima, K. Correlation between histopathologic features and magnetic resonance images of spinal cord lesions. Spine 18, 1140–1149 (1993).
Fukuoka, M., Matsui, N., Otsuka, T., Murakami, M. & Seo, Y. Magnetic resonance imaging of experimental subacute spinal cord compression. Spine 23, 1540–1549 (1998).
Hackney, D. B., Finkelstein, S. D., Hand, C. M., Markowitz, R. S. & Black, P. Postmortem magnetic resonance imaging of experimental spinal cord injury. Neurosurgery 35, 1104–1111 (1994).
Takahashi, T., Suto, Y., Kato, S. & Ohama, E. Experimental acute dorsal compression of cat spinal cord: correlation of magnetic resonance signal intensity with spinal cord evoked potentials and morphology. Spine 21, 166–173 (1996).
FALCI, S. et al. Obliteration of a posttraumatic spinal cord cyst with solid human embryonic spinal cord grafts: first clinical attempt. J. Neurotrauma 14, 875–884 (1997).
Ito, D. et al. Prognostic value of magnetic resonance imaging in dogs with paraplegia caused by thoracolumbar intervertebral disk extrusion: 77 cases (2000–2003). J. Am. Vet. Med. Assoc. 227, 1454–1460 (2005).
Budde, M. D. et al. Toward accurate diagnosis of white matter pathology using diffusion tensor imaging. Magn. Reson. Med. 57, 688–695 (2007).
Kim, J. H. et al. Noninvasive diffusion tensor imaging of evolving white matter pathology in a mouse model of acute spinal cord injury. Magn. Reson. Med. 58, 253–260 (2007).
Kozlowski, P. et al. Characterizing white matter damage in rat spinal cord with quantitative MRI and histology. J. Neurotrauma 25, 653–676 (2008).
Xie, M., Wang, Q., Wu, T.-H., Song, S.-K. & Sun, S.-W. Delayed axonal degeneration in slow Wallerian degeneration mutant mice detected using diffusion tensor imaging. Neuroscience 197, 339–347 (2011).
Brennan, F. H., Cowin, G. J., Kurniawan, N. D. & Ruitenberg, M. J. Longitudinal assessment of white matter pathology in the injured mouse spinal cord through ultra-high field (16.4T) in vivo diffusion tensor imaging. Neuroimage 82, 574–585 (2013).
Zhang, J. et al. Diffusion tensor magnetic resonance imaging of Wallerian degeneration in rat spinal cord after dorsal root axotomy. J. Neurosci. 29, 3160–3171 (2009).
Song, S.-K. et al. Diffusion tensor imaging detects and differentiates axon and myelin degeneration in mouse optic nerve after retinal ischemia. Neuroimage 20, 1714–1722 (2003).
Sun, S.-W., Liang, H.-F., Cross, A. H. & Song, S.-K. Evolving Wallerian degeneration after transient retinal ischemia in mice characterized by diffusion tensor imaging. Neuroimage 40, 1–10 (2008).
Huber, E., Lachappelle, P., Sutter, R., Curt, A. & Freund, P. Are midsagittal tissue bridges predictive of outcome after cervical spinal cord injury? Ann. Neurol. 81, 740–748 (2017).
Vallotton, K. et al. Width and neurophysiologic properties of tissue bridges predict recovery after cervical injury. Neurology 92, e2793–e2802 (2019).
Farhadi, H. F. et al. Impact of admission imaging findings on neurological outcomes in acute cervical traumatic spinal cord injury. J. Neurotrauma 35, 1398–1406 (2018).
Talbott, J. F. et al. The brain and spinal injury center score: a novel, simple, and reproducible method for assessing the severity of acute cervical spinal cord injury with axial T2-weighted MRI findings. J. Neurosurg. Spine 23, 495–504 (2015).
Pfyffer, D., Huber, E., Sutter, R., Curt, A. & Freund, P. Tissue bridges predict recovery after traumatic and ischemic thoracic spinal cord injury. Neurology 93, e1550 (2019).
Freund, P. et al. MRI investigation of the sensorimotor cortex and the corticospinal tract after acute spinal cord injury: a prospective longitudinal study. Lancet Neurol. 12, 873–881 (2013).
Grabher, P. et al. Tracking sensory system atrophy and outcome prediction in spinal cord injury. Ann. Neurol. 78, 751–761 (2015).
Ziegler, G. et al. Progressive neurodegeneration following spinal cord injury. Neurology 90, e1257–e1266 (2018).
Freund, P. et al. Disability, atrophy and cortical reorganization following spinal cord injury. Brain 134, 1610–1622 (2011).
Huber, E. et al. Dorsal and ventral horn atrophy is associated with clinical outcome after spinal cord injury. Neurology 90, e1510–e1522 (2018).
Lundell, H. et al. Independent spinal cord atrophy measures correlate to motor and sensory deficits in individuals with spinal cord injury. Spinal Cord 49, 70–75 (2011).
David, G. et al. In vivo evidence of remote neural degeneration in the lumbar enlargement after cervical injury. Neurology 92, e1367–e1377 (2019).
Huber, E., Curt, A. & Freund, P. Tracking trauma-induced structural and functional changes above the level of spinal cord injury. Curr. Opin. Neurol. 28, 365–372 (2015).
Freund, P. et al. MRI in traumatic spinal cord injury: from clinical assessment to neuroimaging biomarkers. Lancet Neurol. https://doi.org/10.1016/S1474-4422(19)30138-3 (2019).
Kucher, K. et al. First-in-man intrathecal application of neurite growth-promoting anti-nogo-A antibodies in acute spinal cord injury. Neurorehabil. Neural Repair 32, 578–589 (2018).
Freund, P. et al. Nogo-A-specific antibody treatment enhances sprouting and functional recovery after cervical lesion in adult primates. Nat. Med. 12, 790–792 (2006).
Jungmann, P. M., Agten, C. A., Pfirrmann, C. W. & Sutter, R. Advances in MRI around metal. J. Magn. Reson. Imaging 46, 972–991 (2017).
Jungmann, P. M. et al. View-angle tilting and slice-encoding metal artifact correction for artifact reduction in MRI: experimental sequence optimization for orthopaedic tumor endoprostheses and clinical application. PLOS ONE 10, e0124922 (2015).
Lu, W., Pauly, K. B., Gold, G. E., Pauly, J. M. & Hargreaves, B. A. SEMAC: slice encoding for metal artifact correction in MRI. Magn. Reson. Med. 62, 66–76 (2009).
Song, K. D., Yoon, Y. C. & Park, J. Reducing metallic artefacts in post-operative spinal imaging: slice encoding for metal artefact correction with dual-source parallel radiofrequency excitation MRI at 3.0T. Br. J. Radiol. 86, 20120524 (2013).
Worters, P. W., Sung, K., Stevens, K. J., Koch, K. M. & Hargreaves, B. A. Compressed-sensing multispectral imaging of the postoperative spine. J. Magn. Reson. Imaging 37, 243–248 (2013).
Shanmuganathan, K., Gullapalli, R. P., Zhuo, J. & Mirvis, S. E. Diffusion tensor MR imaging in cervical spine trauma. AJNR Am. J. Neuroradiol. 29, 655–659 (2008).
Cheran, S. et al. Correlation of MR diffusion tensor imaging parameters with ASIA motor scores in hemorrhagic and nonhemorrhagic acute spinal cord injury. J. Neurotrauma 28, 1881–1892 (2011).
Chang, Y., Jung, T.-D., Yoo, D. S. & Hyun, J. K. Diffusion tensor imaging and fiber tractography of patients with cervical spinal cord injury. J. Neurotrauma 27, 2033–2040 (2010).
Schwartz, E. D. et al. Apparent diffusion coefficients in spinal cord transplants and surrounding white matter correlate with degree of axonal dieback after injury in rats. AJNR. Am. J. Neuroradiol. 26, 7–18 (2005).
Deo, A. A., Grill, R. J., Hasan, K. M. & Narayana, P. A. In vivo serial diffusion tensor imaging of experimental spinal cord injury. J. Neurosci. Res. 83, 801–810 (2006).
Ellingson, B. M., Ulmer, J. L., Kurpad, S. N. & Schmit, B. D. Diffusion tensor MR imaging in chronic spinal cord injury. AJNR Am. J. Neuroradiol. 29, 1976–1982 (2008).
Koskinen, E. et al. Assessing the state of chronic spinal cord injury using diffusion tensor imaging. J. Neurotrauma 30, 1587–1595 (2013).
Vedantam, A., Eckardt, G., Wang, M. C., Schmit, B. D. & Kurpad, S. N. Clinical correlates of high cervical fractional anisotropy in acute cervical spinal cord injury. World Neurosurg. 83, 824–828 (2015).
Petersen, J. A. et al. Chronic cervical spinal cord injury: DTI correlates with clinical and electrophysiological measures. J. Neurotrauma 29, 1556–1566 (2012).
Loy, D. N. et al. Diffusion tensor imaging predicts hyperacute spinal cord injury severity. J. Neurotrauma 24, 979–990 (2007).
Li, X.-H. et al. Timing of diffusion tensor imaging in the acute spinal cord injury of rats. Sci. Rep. 5, 12639 (2015).
Freund, P. et al. Degeneration of the injured cervical cord is associated with remote changes in corticospinal tract integrity and upper limb impairment. PLOS ONE 7, e51729 (2012).
Cohen-Adad, J. et al. Demyelination and degeneration in the injured human spinal cord detected with diffusion and magnetization transfer MRI. Neuroimage 55, 1024–1033 (2011).
Pearse, D. D. et al. Histopathological and behavioral characterization of a novel cervical spinal cord displacement contusion injury in the rat. J. Neurotrauma 22, 680–702 (2005).
Anderson, K. D., Borisoff, J. F., Johnson, R. D., Stiens, S. A. & Elliott, S. L. The impact of spinal cord injury on sexual function: concerns of the general population. Spinal Cord 45, 328–337 (2007).
Yiannakas, M. C. et al. Reduced field-of-view diffusion-weighted imaging of the lumbosacral enlargement: a pilot in vivo study of the healthy spinal cord at 3T. PLOS ONE 11, e0164890 (2016).
Schwab, M. E. & Bartholdi, D. Degeneration and regeneration of axons in the lesioned spinal cord. Physiol. Rev. 76, 319–370 (1996).
O’Dell, D. R. et al. Midsagittal tissue bridges are associated with walking ability in incomplete spinal cord injury: a magnetic resonance imaging case series. J. Spinal Cord Med. 22, 1–4 (2018).
Koskinen, E. A. et al. Clinical correlates of cerebral diffusion tensor imaging findings in chronic traumatic spinal cord injury. Spinal Cord 52, 202–208 (2014).
Shanmuganathan, K. et al. Diffusion tensor imaging parameter obtained during acute blunt cervical spinal cord injury in predicting long-term outcome. J. Neurotrauma 34, 2964–2971 (2017).
Kim, J. H. et al. Diffusion tensor imaging at 3 hours after traumatic spinal cord injury predicts long-term locomotor recovery. J. Neurotrauma 27, 587–598 (2010).
Martin, A. R. et al. Monitoring for myelopathic progression with multiparametric quantitative MRI. PLOS ONE 13, e0195733 (2018).
Nouri, A. et al. MRI analysis of the combined prospectively collected AOSpine North America and international data: the prevalence and spectrum of pathologies in a global cohort of patients with degenerative cervical myelopathy. Spine 42, 1058–1067 (2017).
Harrop, J. S. et al. Cervical myelopathy. Spine 35, 620–624 (2010).
Martin, A. R. et al. A novel MRI biomarker of spinal cord white matter injury: t2*-weighted white matter to gray matter signal intensity ratio. AJNR Am. J. Neuroradiol. 38, 1266–1273 (2017).
Grabher, P. et al. Voxel-based analysis of grey and white matter degeneration in cervical spondylotic myelopathy. Sci. Rep. 6, 24636 (2016).
Martin, A. R. et al. Can microstructural MRI detect subclinical tissue injury in subjects with asymptomatic cervical spinal cord compression? A prospective cohort study. BMJ Open 8, e019809 (2018).
Martin, A. R. et al. Imaging evaluation of degenerative cervical myelopathy. Neurosurg. Clin. N. Am. 29, 33–45 (2018).
Facon, D. et al. MR diffusion tensor imaging and fiber tracking in spinal cord compression. AJNR Am. J .Neuroradiol. 26, 1587–1594 (2005).
Ford, J. C., Hackney, D. B., Lavi, E., Phillips, M. & Patel, U. Dependence of apparent diffusion coefficients on axonal spacing, membrane permeability, and diffusion time in spinal cord white matter. J. Magn. Reson. Imaging 8, 775–782 (1998).
Budzik, J.-F. et al. Diffusion tensor imaging and fibre tracking in cervical spondylotic myelopathy. Eur. Radiol. 21, 426–433 (2011).
Uda, T. et al. Assessment of cervical spondylotic myelopathy using diffusion tensor magnetic resonance imaging parameter at 3.0 tesla. Spine 38, 407–414 (2013).
Rajasekaran, S. et al. The assessment of neuronal status in normal and cervical spondylotic myelopathy using diffusion tensor imaging. Spine 39, 1183–1189 (2014).
Chen, X. et al. Magnetic resonance diffusion tensor imaging of cervical spinal cord and lumbosacral enlargement in patients with cervical spondylotic myelopathy. J. Magn. Reson. Imaging 43, 1484–1491 (2016).
Vedantam, A. et al. Diffusion tensor imaging correlates with short-term myelopathy outcome in patients with cervical spondylotic myelopathy. World Neurosurg. 97, 489–494 (2017).
Wen, C. Y. et al. Is diffusion anisotropy a biomarker for disease severity and surgical prognosis of cervical spondylotic myelopathy? Radiology 270, 197–204 (2014).
Cui, J.-L. et al. Quantitative assessment of column-specific degeneration in cervical spondylotic myelopathy based on diffusion tensor tractography. Eur. Spine J. 24, 41–47 (2015).
Yu, W.-R. et al. Molecular mechanisms of spinal cord dysfunction and cell death in the spinal hyperostotic mouse: implications for the pathophysiology of human cervical spondylotic myelopathy. Neurobiol. Dis. 33, 149–163 (2009).
Martin, A. R. et al. Clinically feasible microstructural MRI to quantify cervical spinal cord tissue injury using DTI, MT, and t2*-weighted imaging: assessment of normative data and reliability. Am. J. Neuroradiol. 38, 1257–1265 (2017).
Jones, J. G. A., Cen, S. Y., Lebel, R. M., Hsieh, P. C. & Law, M. Diffusion tensor imaging correlates with the clinical assessment of disease severity in cervical spondylotic myelopathy and predicts outcome following surgery. Am. J. Neuroradiol. 34, 471–478 (2013).
Kerkovský, M. et al. Magnetic resonance diffusion tensor imaging in patients with cervical spondylotic spinal cord compression. Spine 37, 48–56 (2012).
Sato, T. et al. Evaluation of cervical myelopathy using apparent diffusion coefficient measured by diffusion-weighted imaging. Am. J. Neuroradiol. 33, 388–392 (2012).
Lemon, R. N. & Griffiths, J. Comparing the function of the corticospinal system in different species: organizational differences for motor specialization? Muscle Nerve 32, 261–279 (2005).
Starkey, M. L. & Schwab, M. E. Anti-nogo-A and training: can one plus one equal three? Exp. Neurol. 235, 53–61 (2012).
Karadimas, S. K., Gatzounis, G. & Fehlings, M. G. Pathobiology of cervical spondylotic myelopathy. Eur. Spine J. 2, 132–138 (2015).
Yu, W. R., Liu, T., Kiehl, T. R. & Fehlings, M. G. Human neuropathological and animal model evidence supporting a role for Fas-mediated apoptosis and inflammation in cervical spondylotic myelopathy. Brain 134, 1277–1292 (2011).
Seif, M. et al. Cervical cord neurodegeneration in traumatic and non-traumatic spinal cord injury. J. Neurotrauma https://doi.org/10.1089/neu.2019.6694 (2019).
Cohen-Adad, J. & Wheeler-Kingshott, C. A. M. Quantitative MRI of the Spinal Cord (Elsevier, 2014).
Setsompop, K. et al. High-resolution in vivo diffusion imaging of the human brain with generalized slice dithered enhanced resolution: simultaneous multislice (gSlider-SMS). Magn. Reson. Med. 79, 141–151 (2018).
Barry, R. L., Vannesjo, S. J., By, S., Gore, J. C. & Smith, S. A. Spinal cord MRI at 7T. Neuroimage 168, 437–451 (2018).
Wilm, B. J. et al. Diffusion-weighted imaging of the entire spinal cord. NMR Biomed. 22, 174–181 (2009).
Finsterbusch, J., Eippert, F. & Büchel, C. Single, slice-specific z-shim gradient pulses improve T2*-weighted imaging of the spinal cord. Neuroimage 59, 2307–2315 (2012).
Topfer, R., Foias, A., Stikov, N. & Cohen-Adad, J. Real-time correction of respiration-induced distortions in the human spinal cord using a 24-channel shim array. Magn. Reson. Med. 80, 935–946 (2018).
Vannesjo, S. J., Clare, S., Kasper, L., Tracey, I. & Miller, K. L. A method for correcting breathing-induced field fluctuations in T2*-weighted spinal cord imaging using a respiratory trace. Magn. Reson. Med. 81, 3745–3753 (2019).
Stejskal, E. O. & Tanner, J. E. Spin diffusion measurements: spin echoes in the presence of a time-dependent field gradient. J. Chem. Phys. 42, 288–292 (1965).
Shemesh, N. et al. Conventions and nomenclature for double diffusion encoding NMR and MRI. Magn. Reson. Med. 75, 82–87 (2016).
Coelho, S., Pozo, J. M., Jespersen, S. N., Jones, D. K. & Frangi, A. F. Resolving degeneracy in diffusion MRI biophysical model parameter estimation using double diffusion encoding. Magn. Reson. Med. 82, 395–410 (2019).
Reisert, M., Kiselev, V. G. & Dhital, B. A unique analytical solution of the white matter standard model using linear and planar encodings. Magn. Reson. Med. 81, 3819–3825 (2019).
Yang, G., Tian, Q., Leuze, C., Wintermark, M. & McNab, J. A. Double diffusion encoding MRI for the clinic. Magn. Reson. Med. 80, 507–520 (2018).
Jones, D. K., Knösche, T. R. & Turner, R. White matter integrity, fiber count, and other fallacies: the do’s and don’ts of diffusion MRI. Neuroimage 73, 239–254 (2013).
Wheeler-Kingshott, C. A. & Cercignani, M. About ‘axial’ and ‘radial’ diffusivities. Magn Reson. 61, 1255–1260 (2009).
Jensen, J. H., Helpern, J. A., Ramani, A., Lu, H. & Kaczynski, K. Diffusional kurtosis imaging: the quantification of non-gaussian water diffusion by means of magnetic resonance imaging. Magn. Reson. Med. 53, 1432–1440 (2005).
Assaf, Y. & Basser, P. J. Composite hindered and restricted model of diffusion (CHARMED) MR imaging of the human brain. Neuroimage 27, 48–58 (2005).
Zhang, H., Schneider, T., Wheeler-Kingshott, C. A. & Alexander, D. C. NODDI: practical in vivo neurite orientation dispersion and density imaging of the human brain. Neuroimage 61, 1000–1016 (2012).
Hori, M. et al. Application of quantitative microstructural MR imaging with atlas-based analysis for the spinal cord in cervical spondylotic myelopathy. Sci. Rep. 8, 5213 (2018).
Okita, G. et al. Application of neurite orientation dispersion and density imaging or diffusion tensor imaging to quantify the severity of cervical spondylotic myelopathy and to assess postoperative neurologic recovery. Spine J. 18, 268–275 (2018).
Novikov, D. S., Kiselev, V. G. & Jespersen, S. N. On modeling. Magn. Reson. Med. 79, 3172–3193 (2018).
Morawski, M. et al. Developing 3D microscopy with CLARITY on human brain tissue: towards a tool for informing and validating MRI-based histology. Neuroimage 182, 417–428 (2018).
Stikov, N. et al. Bound pool fractions complement diffusion measures to describe white matter micro and macrostructure. Neuroimage 54, 1112–1121 (2011).
Callaghan, M. F., Helms, G., Lutti, A., Mohammadi, S. & Weiskopf, N. A general linear relaxometry model of R1 using imaging data. Magn. Reson. Med. 73, 1309–1314 (2015).
Helms, G., Dathe, H., Kallenberg, K. & Dechent, P. High-resolution maps of magnetization transfer with inherent correction for RF inhomogeneity and T1 relaxation obtained from 3D FLASH MRI. Magn. Reson. Med. 60, 1396–1407 (2008).
MacKay, A. et al. In vivo visualization of myelin water in brain by magnetic resonance. Magn. Reson. Med. 31, 673–677 (1994).
Wolff, S. D. & Balaban, R. S. Magnetization transfer contrast (MTC) and tissue water proton relaxation in vivo. Magn. Reson. Med. 10, 135–144 (1989).
Thiessen, J. D. et al. Quantitative MRI and ultrastructural examination of the cuprizone mouse model of demyelination. NMR Biomed. 26, 1562–1581 (2013).
Levesque, I. et al. The role of edema and demyelination in chronic T1 black holes: a quantitative magnetization transfer study. J. Magn. Reson. Imaging 21, 103–110 (2005).
Wyss, P. O. et al. MR Spectroscopy of the cervical spinal cord in chronic spinal cord injury. Radiology 291, 131–138 (2019).
Holly, L. T., Freitas, B., McArthur, D. L. & Salamon, N. Proton magnetic resonance spectroscopy to evaluate spinal cord axonal injury in cervical spondylotic myelopathy. J. Neurosurg. Spine 10, 194–200 (2009).
Powers, J. et al. Ten key insights into the use of spinal cord fMRI. Brain Sci. 8, 173 (2018).
Stroman, P. W. et al. Noninvasive assessment of the injured human spinal cord by means of functional magnetic resonance imaging. Spinal Cord 42, 59–66 (2004).
Cadotte, D. W. et al. Plasticity of the injured human spinal cord: insights revealed by spinal cord functional MRI. PLOS ONE 7, e45560 (2012).
Ellingson, B. M., Woodworth, D. C., Leu, K., Salamon, N. & Holly, L. T. Spinal cord perfusion MR imaging implicates both ischemia and hypoxia in the pathogenesis of cervical spondylosis. World Neurosurg. 128, e773–e781 (2019).
Tabelow, K. et al. hMRI — a toolbox for quantitative MRI in neuroscience and clinical research. Neuroimage 194, 191–210 (2019).
Edwards, L. J., Kirilina, E., Mohammadi, S. & Weiskopf, N. Microstructural imaging of human neocortex in vivo. Neuroimage 182, 184–206 (2018).
Weiskopf, N., Mohammadi, S., Lutti, A. & Callaghan, M. F. Advances in MRI-based computational neuroanatomy: from morphometry to in-vivo histology. Curr. Opin. Neurol. 28, 313–322 (2015).
West, K. L. et al. Myelin volume fraction imaging with MRI. Neuroimage 182, 511–521 (2018).
Edwards, L. J., Pine, K. J., Ellerbrock, I., Weiskopf, N. & Mohammadi, S. NODDI-DTI: estimating neurite orientation and dispersion parameters from a diffusion tensor in healthy white matter. Front. Neurosci. 11, 720 (2017).
Jespersen, S. N., Olesen, J. L., Hansen, B. & Shemesh, N. Diffusion time dependence of microstructural parameters in fixed spinal cord. Neuroimage 182, 329–342 (2018).
Lampinen, B. et al. Neurite density imaging versus imaging of microscopic anisotropy in diffusion MRI: a model comparison using spherical tensor encoding. Neuroimage 147, 517–531 (2017).
Stikov, N. et al. In vivo histology of the myelin g-ratio with magnetic resonance imaging. Neuroimage 118, 397–405 (2015).
Mohammadi, S. et al. Whole-brain in-vivo measurements of the axonal g-ratio in a group of 37 healthy volunteers. Front. Neurosci. 9, 441 (2015).
De Leener, B., Kadoury, S. & Cohen-Adad, J. Robust, accurate and fast automatic segmentation of the spinal cord. Neuroimage 98, 528–536 (2014).
Mohammadi, S., Freund, P., Feiweier, T., Curt, A. & Weiskopf, N. The impact of post-processing on spinal cord diffusion tensor imaging. Neuroimage 70, 377–385 (2013).
David, G., Freund, P. & Mohammadi, S. The efficiency of retrospective artifact correction methods in improving the statistical power of between-group differences in spinal cord DTI. Neuroimage 158, 296–307 (2017).
De Leener, B. et al. PAM50: unbiased multimodal template of the brainstem and spinal cord aligned with the ICBM152 space. Neuroimage 165, 170–179 (2018).
Lévy, S. et al. White matter atlas of the human spinal cord with estimation of partial volume effect. Neuroimage 119, 262–271 (2015).
Eden, D. et al. Spatial distribution of multiple sclerosis lesions in the cervical spinal cord. Brain 142, 633–646 (2019).
Hopkins, B. S. et al. Tract-specific volume loss on 3T MRI in patients with cervical spondylotic myelopathy. Spine 43, 1 (2018).
Sprenger, C., Stenmans, P., Tinnermann, A. & Büchel, C. Evidence for a spinal involvement in temporal pain contrast enhancement. Neuroimage 183, 788–799 (2018).
Cadotte, D. W. & Fehlings, M. G. Will imaging biomarkers transform spinal cord injury trials? Lancet Neurol. 12, 843–844 (2013).
Acknowledgements
S.M. has received funding from the ERA-NET NEURON (hMRIofSCI) and the Bundesministerium für Bildung und Forschung (BMBF; 01EW1711A and B) and is supported by the Deutsche Forschungsgemeinschaft (grant MO 2397/4-1) and the Forschungszentrums Medizintechnik Hamburg (fmthh; grant 01fmthh2017). A.R.M. has received support from the Canadian Institutes of Health Research (CHIR; 359116). J.C.-A. holds funding from the Canada Research Chair in Quantitative Magnetic Resonance Imaging (950–230815), the CIHR (FDN-143263), the Canada Foundation for Innovation (32454, 34824), the Fonds de Recherche du Québec – Santé (28826), the Natural Sciences and Engineering Research Council of Canada (435897-2013), the Canada First Research Excellence Fund (IVADO and TransMedTech) and the Quebec BioImaging Network (5886), Spinal Research and Wings for Life (INSPIRED project). N.W. reports grants from the European Research Council/ERC grant agreement no. 616905, grants from the BMBF (01EW1711A B) in the framework of ERA-NET NEURON, grants from the BRAINTRAIN European research network (Collaborative Project) supported by the European Commission (grant agreement no. 602186), grants from NISCI supported by the European Union’s Horizon 2020 research and innovation program under the grant agreement no. 681094, and supported by the Swiss State Secretariat for Education, Research and Innovation (SERI) under contract number 15.0137, and grants from UCL Impact Awards; The Wellcome Centre for Human Neuroimaging and Max Planck Institute for Human Cognitive and Brain Sciences have institutional research agreements with Siemens Healthcare. P.F. reports grants from ERA-NET NEURON (hMRIofSCI no. 32NE30_173678), grants from NISCI supported by the European Union’s Horizon 2020 research and innovation program under grant agreement no. 681094, and supported by the Swiss State Secretariat for Education, Research and Innovation (SERI) under contract number 15.0137, grants from the Wings for life charity (no. WFL-CH-007/14) and grants from the International Foundation for Research (IRP-158). P.F. is funded by a SNF Eccellenza Professorial Fellowship grant (PCEFP3_181362/1). A.T. acknowledges support from the UCL/UCLH NIHR Biomedical Research Centre.
Review criteria
PubMed and MEDLINE were searched for articles published in English from 1 January 2010 to 31 March 2019. The search terms “traumatic spinal cord injury”, “cervical spondylotic myelopathy” and “degenerative spondylotic myelopathy” were used in combination with each of the terms “diffusion MRI”, “diffusion tensor imaging”, “DTI”, “conventional MRI”, and “atrophy”. The reference lists of the identified papers were also searched for further articles. The final reference list for inclusion in this Review was generated on the basis of originality and relevance to the topics covered.
Author information
Authors and Affiliations
Contributions
All authors provided substantial contributions to discussion of the content of the article, wrote the article and undertook the review and/or editing of the manuscript before submission. G.D and P.F also researched data for the article.
Corresponding author
Ethics declarations
Competing interests
A.T. reports personal fees paid to his institution from Eisai Ltd. and fees and support for travel from Hoffmann-La Roche outside the submitted work. A.T. is an Editorial Board member of The Lancet Neurology and receives a free subscription. A.T. is the Editor-in-Chief of the Multiple Sclerosis Journal and receives an honorarium from SAGE Publications. A.T. receives support for travel as Chair, Scientific Advisory Committee, International Progressive MS Alliance, and member, National MS Society (USA), Research Programs Advisory Committee. A.T. has received honoraria and support for travel for lecturing from Almirall and EXCEMED. N.W. is supported by Siemens Healthcare. The other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Neurology thanks L. Holly, S. Kurpad and P. Narayana for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- T1-weighted
-
T1-weighted MRI pulse sequences are optimized to create an image contrast that primarily depends on the T1 (longitudinal or spin-lattice) relaxation time of the tissue. In T1-weighted images, white matter appears bright and grey matter appears dark.
- T2-weighted
-
T2-weighted MRI pulse sequences are optimized to create an image contrast that primarily depends on the T2 (transversal or spin-spin) relaxation time of the tissue. In T2-weighted images, areas of water accumulation (for example, oedema or lesions) appear bright in contrast with other tissue.
- Anisotropic
-
A type of diffusion with direction dependency; that is, the diffusion is not the same in all spatial directions (for example, in white matter).
- Tensor
-
Mathematical object used to describe diffusion in homogeneous anisotropic media, having the form of a 3 × 3 symmetrical matrix for 3D diffusion.
- Scalar
-
A scalar is a quantity that is completely described by its magnitude.
- Isotropic
-
A type of diffusion with no directional dependency; that is, the diffusion is the same in all spatial directions (for example, in a glass of water).
- Wallerian degeneration
-
A degenerative process that involves the breakdown of the distal part of a severed axon.
- Pulse sequences
-
In MRI, a pulse sequence refers to a particular setting of measurement parameters. Each pulse sequence results in a particular image appearance, with T1-weighted, T2-weighted, and diffusion-weighted pulse sequences resulting in T1, T2, and diffusion image contrasts, respectively.
- Gradient echo-based T2*-weighted sequences
-
MRI pulse sequences that are optimized to create an image contrast that depends primarily on T2* (effective transversal) relaxation time. T2*-weighted images offer good distinction between grey and white matter in the spinal cord and form the basis of grey matter segmentation.
- Partial volume effects
-
Artefacts that arise at tissue interfaces where multiple tissues are contained in a single voxel. These artefacts are more severe at lower resolution.
- Susceptibility artefacts
-
Artefacts resulting from the different magnetic properties of tissues. They appear at and near tissue interfaces and lead to image distortions and signal dropouts.
- Coil coverage
-
Part of the body that falls into the receptive field of the receiver coils.
- Receive coil
-
Part of the MRI hardware that is responsible for receiving the signal and is crucial for acquiring images with high signal-to-noise ratios.
- Shimming
-
A procedure that aims to make the magnetic field homogeneous within the imaging volume, which is crucial for good-quality, distortion-free images.
- Field fluctuations
-
Variations in the magnetic field within the body caused by susceptibility artefacts and imperfect shimming.
- Pulsed field gradient design
-
A pair of spatially varying magnetic fields (gradients) applied in succession to encode the water diffusion along a particular direction in diffusion-weighted MRI scans.
- Double diffusion encoding
-
In contrast to the pulsed field gradient design, this technique encodes diffusion along two directions in the images.
- Nonlinear diffusion encoding
-
A modification of the pulsed field gradient design, where the variation of the applied spatially varying magnetic field is not linear.
- b-value
-
A scalar measure that describes the amount of diffusion weighting in the images; a higher b-value means more diffusion weighting but also less signal.
- Restricted diffusion component
-
Usually refers to the intracellular space of white matter, which is assumed to show a restricted diffusion profile, meaning that the myelinated axons are impermeable to water molecules.
- Multicontrast biophysical models
-
Models that incorporate information from multiple types of MRI acquisitions (contrasts) to estimate a meaningful tissue parameter such as axonal or myelin volume fraction.
Rights and permissions
About this article
Cite this article
David, G., Mohammadi, S., Martin, A.R. et al. Traumatic and nontraumatic spinal cord injury: pathological insights from neuroimaging. Nat Rev Neurol 15, 718–731 (2019). https://doi.org/10.1038/s41582-019-0270-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-019-0270-5
This article is cited by
-
Intrathecal injection of human placental mesenchymal stem cells derived exosomes significantly improves functional recovery in spinal cord injured rats
Molecular Biology Reports (2024)
-
Mesoporous polydopamine delivering 8-gingerol for the target and synergistic treatment to the spinal cord injury
Journal of Nanobiotechnology (2023)
-
Targeting ANXA7/LAMP5-mTOR axis attenuates spinal cord injury by inhibiting neuronal apoptosis via enhancing autophagy in mice
Cell Death Discovery (2023)
-
Investigation of perfusion impairment in degenerative cervical myelopathy beyond the site of cord compression
Scientific Reports (2023)
-
Targeting epigenetic and posttranslational modifications regulating ferroptosis for the treatment of diseases
Signal Transduction and Targeted Therapy (2023)