Abstract
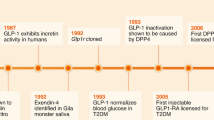
Gut hormones have many key roles in the control of metabolism, as they target diverse tissues involved in the control of intestinal function, insulin secretion, nutrient assimilation and food intake. Produced by scattered cells found along the length of the intestinal epithelium, gut hormones generate signals related to the rate of nutrient absorption, the composition of the luminal milieu and the integrity of the epithelial barrier. Gut hormones already form the basis for existing and developing therapeutics for type 2 diabetes mellitus and obesity, exemplified by the licensed glucagon-like peptide 1 (GLP1) mimetics and dipeptidyl peptidase inhibitors that enhance GLP1 receptor activation. Modulating the release of the endogenous stores of GLP1 and other gut hormones is thought to be a promising strategy to mimic bariatric surgery with its multifaceted beneficial effects on food intake, body weight and blood glucose levels. This Review focuses on the molecular mechanisms underlying the modulation of gut hormone release by food ingestion, obesity and the gut microbiota. Depending on the nature of the stimulus, release of gut hormones involves recruitment of a variety of signalling pathways, including G protein-coupled receptors, nutrient transporters and ion channels, which are targets for future therapeutics for diabetes mellitus and obesity.
Key points
-
Enteroendocrine cells produce a range of gut hormones that have key roles in the coordination of food digestion and absorption, insulin secretion and appetite.
-
Products of food digestion (for example, glucose, amino acids and fatty acids) and microbial fermentation (such as short chain fatty acids (SCFAs)) act as stimuli for local enteroendocrine cells.
-
Nutrient sensing by enteroendocrine cells involves a range of signalling pathways, including G protein-coupled receptors, nutrient transporters and ion channels.
-
Gut hormones, such as glucagon-like peptide 1, cholecystokinin and glucose-dependent insulinotropic polypeptide, are secreted rapidly following food ingestion and have key roles in human metabolism through their anorexigenic and/or insulinotropic actions.
-
The gut microbiota produces various metabolites (including SCFAs, secondary bile acids and lipopolysaccharides) that modulate enteroendocrine cells, generating hormonal signals that reflect dietary intake, microbial composition and epithelial integrity.
-
Bariatric surgery rearranges intestinal anatomy, resulting in markedly elevated postprandial concentrations of glucagon-like peptide 1 and peptide YY, which contribute to postsurgical weight loss and resolution of type 2 diabetes mellitus in humans.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Nauck, M. A., Bartels, E., Orskov, C., Ebert, R. & Creutzfeldt, W. Additive insulinotropic effects of exogenous synthetic human gastric inhibitory polypeptide and glucagon-like peptide-1-(7–36) amide infused at near-physiological insulinotropic hormone and glucose concentrations. J. Clin. Endocrinol. Metab. 76, 912–917 (1993).
Adriaenssens, A. E. et al. Transcriptomic profiling of pancreatic alpha, beta and delta cell populations identifies delta cells as a principal target for ghrelin in mouse islets. Diabetologia 59, 2156–2165 (2016).
Andersen, A., Lund, A., Knop, F. K. & Vilsbøll, T. Glucagon-like peptide 1 in health and disease. Nat. Rev. Endocrinol. 14, 390–403 (2018).
Nauck, M. A. et al. Preserved incretin activity of glucagon-like peptide 1 [7-36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J. Clin. Invest. 91, 301–307 (1993).
Miyawaki, K. et al. Inhibition of gastric inhibitory polypeptide signaling prevents obesity. Nat. Med. 8, 738–742 (2002).
Capozzi, M. E., DiMarchi, R. D., Tschöp, M. H., Finan, B. & Campbell, J. E. Targeting the incretin/glucagon system with triagonists to treat diabetes. Endocr. Rev. 39, 719–738 (2018).
Tan, T. et al. The effect of a subcutaneous infusion of GLP-1, OXM, and PYY on energy intake and expenditure in obese volunteers. J. Clin. Endocrinol. Metab. 102, 2364–2372 (2017).
Frias, J. P. et al. Efficacy and safety of LY3298176, a novel dual GIP and GLP-1 receptor agonist, in patients with type 2 diabetes: a randomised, placebo-controlled and active comparator-controlled phase 2 trial. Lancet 392, 2180–2193 (2018).
Phillips, L. K., Deane, A. M., Jones, K. L., Rayner, C. K. & Horowitz, M. Gastric emptying and glycaemia in health and diabetes mellitus. Nat. Rev. Endocrinol. 11, 112–128 (2015).
Wu, T., Rayner, C. K., Young, R. L. & Horowitz, M. Gut motility and enteroendocrine secretion. Curr. Opin. Pharmacol. 13, 928–934 (2013).
Müller, T. D. et al. Ghrelin. Mol. Metab. 4, 437–460 (2015).
Grosse, J. et al. Insulin-like peptide 5 is an orexigenic gastrointestinal hormone. Proc. Natl Acad. Sci. USA 111, 11133–11138 (2014).
Lewis, H. B. et al. Effect of reducing portion size at a compulsory meal on later energy intake, gut hormones, and appetite in overweight adults. Obesity (Silver Spring) 23, 1362–1370 (2015).
Brennan, I. M. et al. Effects of fat, protein, and carbohydrate and protein load on appetite, plasma cholecystokinin, peptide YY, and ghrelin, and energy intake in lean and obese men. Am. J. Physiol. Gastrointest. Liver Physiol. 303, G129–G140 (2012).
Gribble, F. M. & Reimann, F. Enteroendocrine cells: chemosensors in the intestinal epithelium. Annu. Rev. Physiol. 78, 277–299 (2016).
Li, H. J., Ray, S. K., Singh, N. K., Johnston, B. & Leiter, A. B. Basic helix-loop-helix transcription factors and enteroendocrine cell differentiation. Diabetes Obes. Metab. 13 (Suppl. 1), 5–12 (2011).
Eissele, R. et al. Glucagon-like peptide-1 cells in the gastrointestinal-tract and pancreas of rat, pig and man. Eur. J. Clin. Invest. 22, 283–291 (1992).
Sakata, I. & Sakai, T. Ghrelin cells in the gastrointestinal tract. Int. J. Pept. 2010, 945056 (2010).
Kusumoto, Y., Grube, D., Sato, A. G., Kaneda, K. & Nakamae, E. Cytology and arrangement of enterochromaffin (EC) cells in the human stomach. Arch. Histol Cytol. 51, 271–276 (1988).
Dockray, G. J. Cholecystokinin and gut-brain signalling. Regul. Pept. 155, 6–10 (2009).
Williams, E. K. et al. Sensory neurons that detect stretch and nutrients in the digestive system. Cell 166, 209–221 (2016).
Martin, A. M. et al. The diverse metabolic roles of peripheral serotonin. Endocrinology 158, 1049–1063 (2017).
Bellono, N. W. et al. Enterochromaffin cells are gut chemosensors that couple to sensory neural pathways. Cell 170, 185–198 (2017).
Lund, M. L. et al. Enterochromaffin 5-HT cells - a major target for GLP-1 and gut microbial metabolites. Mol. Metab. 11, 70–83 (2018).
Kaelberer, M. M. et al. A gut-brain neural circuit for nutrient sensory transduction. Science 361, eaat5236 (2018).
Lu, V. B. et al. Adenosine triphosphate is co-secreted with glucagon-like peptide-1 to modulate intestinal enterocytes and afferent neurons. Nat. Commun. (in the press).
Han, W. et al. A neural circuit for gut-induced reward. Cell 175, 887–888 (2018).
Nishi, Y. et al. Ingested medium-chain fatty acids are directly utilized for the acyl modification of ghrelin. Endocrinology 146, 2255–2264 (2005).
Aw, T. Y. & Grigor, M. R. Digestion and absorption of milk triacylglycerols in 14-day-old suckling rats. J. Nutr. 110, 2133–2140 (1980).
Ikenoya, C. et al. β-oxidation in ghrelin-producing cells is important for ghrelin acyl-modification. Sci. Rep. 8, 9176 (2018).
Cummings, D. E. et al. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes 50, 1714–1719 (2001).
Brede, S. et al. Visual food cues decrease postprandial glucose concentrations in lean and obese men without affecting food intake and related endocrine parameters. Appetite 117, 255–262 (2017).
Zhao, T. J. et al. Ghrelin secretion stimulated by β1-adrenergic receptors in cultured ghrelinoma cells and in fasted mice. Proc. Natl Acad. Sci. USA 107, 15868–15873 (2010).
Williams, D. L., Cummings, D. E., Grill, H. J. & Kaplan, J. M. Meal-related ghrelin suppression requires postgastric feedback. Endocrinology 144, 2765–2767 (2003).
Sakata, I. et al. Glucose-mediated control of ghrelin release from primary cultures of gastric mucosal cells. Am. J. Physiol. Endocrinol. Metab. 302, E1300–E1310 (2012).
Lu, X. et al. Postprandial inhibition of gastric ghrelin secretion by long-chain fatty acid through GPR120 in isolated gastric ghrelin cells and mice. Am. J. Physiol. Gastrointest. Liver Physiol. 303, G367–376 (2012).
Gong, Z. et al. G protein-coupled receptor 120 signaling regulates ghrelin secretion in vivo and in vitro. Am. J. Physiol. Endocrinol. Metab. 306, E28–E35 (2014).
Engelstoft, M. S. et al. Seven transmembrane G protein-coupled receptor repertoire of gastric ghrelin cells. Mol. Metab. 2, 376–392 (2013).
Billing, L. J. et al. Co-storage and release of insulin-like peptide-5, glucagon-like peptide-1 and peptideYY from murine and human colonic enteroendocrine cells. Mol. Metab. 16, 65–75 (2018).
Lee, Y. S. et al. Insulin-like peptide 5 is a microbially regulated peptide that promotes hepatic glucose production. Mol. Metab. 5, 263–270 (2016).
Luo, X. et al. The insulinotrophic effect of insulin-like peptide 5 in vitro and in vivo. Biochem. J. 466, 467–473 (2015).
Liu, C. et al. INSL5 is a high affinity specific agonist for GPCR142 (GPR100). J. Biol. Chem. 280, 292–300 (2005).
Degen, L. et al. Effect of peptide YY3-36 on food intake in humans. Gastroenterology 129, 1430–1436 (2005).
Kanoski, S. E., Rupprecht, L. E., Fortin, S. M., De Jonghe, B. C. & Hayes, M. R. The role of nausea in food intake and body weight suppression by peripheral GLP-1 receptor agonists, exendin-4 and liraglutide. Neuropharmacology 62, 1916–1927 (2012).
Skibicka, K. P. & Dickson, S. L. Enteroendocrine hormones - central effects on behavior. Curr. Opin. Pharmacol. 13, 977–982 (2013).
O’Neil, P. M. et al. Efficacy and safety of emaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. Lancet 392, 637–649 (2018).
Coskun, T. et al. LY3298176, a novel dual GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes mellitus: from discovery to clinical proof of concept. Mol. Metab. 18, 3–14 (2018).
Mroz, P. A. et al. Optimized GIP analogs promote body weight lowering in mice through GIPR agonism not antagonism. Mol. Metab. 20, 51–62 (2019).
Sjölund, K., Sandén, G., Håkanson, R. & Sundler, F. Endocrine cells in human intestine: an immunocytochemical study. Gastroenterology 85, 1120–1130 (1983).
Habib, A. M. et al. Overlap of endocrine hormone expression in the mouse intestine revealed by transcriptional profiling and flow cytometry. Endocrinology 153, 3054–3065 (2012).
Egerod, K. L. et al. A major lineage of enteroendocrine cells coexpress CCK, secretin, GIP, GLP-1, PYY, and neurotensin but not somatostatin. Endocrinology 153, 5782–5795 (2012).
Roberts, G. et al. Comparison of human and murine enteroendocrine cells by transcriptomic and peptidomic profiling. Diabetes https://doi.org/10.2337/db18-0883.
Grunddal, K. V. et al. Neurotensin is coexpressed, coreleased, and acts together with GLP-1 and PYY in enteroendocrine control of metabolism. Endocrinology 157, 176–194 (2016).
Beumer, J. et al. Enteroendocrine cells switch hormone expression along the crypt-to-villus BMP signalling gradient. Nat. Cell Biol. 20, 909–916 (2018).
Fothergill, L. J., Callaghan, B., Hunne, B., Bravo, D. M. & Furness, J. B. Co-storage of enteroendocrine hormones evaluated at the cell and subcellular levels in male mice. Endocrinology 158, 2113–2123 (2017).
Pilichiewicz, A. N. et al. Load-dependent effects of duodenal glucose on glycemia, gastrointestinal hormones, antropyloroduodenal motility, and energy intake in healthy men. Am. J. Physiol. Endocrinol. Metab. 293, E743–E753 (2007).
Pilichiewicz, A. N. et al. Load-dependent effects of duodenal lipid on antropyloroduodenal motility, plasma CCK and PYY, and energy intake in healthy men. Am. J. Physiol. Regul. Integr. Comp. Physiol. 293, R2170–R2178 (2007).
Little, T. J. et al. The release of GLP-1 and ghrelin, but not GIP and CCK, by glucose is dependent upon the length of small intestine exposed. Am. J. Physiol. Endocrinol. Metab. 291, E647–E655 (2006).
Reimann, F., Tolhurst, G. & Gribble, F. M. G-protein-coupled receptors in intestinal chemosensation. Cell Metab. 15, 421–431 (2012).
Gribble, F. M. The gut endocrine system as a coordinator of postprandial nutrient homoeostasis. Proc. Nutr. Soc. 71, 456–462 (2012).
Gribble, F. M., Diakogiannaki, E. & Reimann, F. Gut hormone regulation and secretion via FFA1 and FFA4. Handb. Exp. Pharmacol. 236, 181–203 (2016).
Moss, C. E. et al. Lipid derivatives activate GPR119 and trigger GLP-1 secretion in primary murine L-cells. Peptides 77, 16–20 (2016).
Maciejewski, B. S., Manion, T. B. & Steppan, C. M. Pharmacological inhibition of diacylglycerol acyltransferase-1 and insights into postprandial gut peptide secretion. World J. Gastrointest. Pathophysiol. 8, 161–175 (2017).
Brighton, C. A. et al. Bile acids trigger GLP-1 release predominantly by accessing basolaterally located G protein-coupled bile acid receptors. Endocrinology 156, 3961–3970 (2015).
Lin, H. V. et al. GPR142 controls tryptophan-induced insulin and incretin hormone secretion to improve glucose metabolism. PLOS ONE 11, e0157298 (2016).
Mace, O. J., Schindler, M. & Patel, S. The regulation of K- and L-cell activity by GLUT2 and CasR in rat small intestine. J. Physiol. 590, 2917–2936 (2012).
Diakogiannaki, E. et al. Oligopeptides stimulate glucagon-like peptide-1 secretion in mice through proton-coupled uptake and the calcium-sensing receptor. Diabetologia 56, 2688–2696 (2013).
Oya, M. et al. The G protein-coupled receptor family C group 6 subtype A (GPRC6A) receptor is involved in amino acid-induced glucagon-like peptide-1 secretion from GLUTag cells. J. Biol. Chem. 288, 4513–4521 (2013).
Jang, H. J. et al. Gut-expressed gustducin and taste receptors regulate secretion of glucagon-like peptide-1. Proc. Natl Acad. Sci. USA 104, 15069–15074 (2007).
Nakamura, E., Hasumura, M., Uneyama, H. & Torii, K. Luminal amino acid-sensing cells in gastric mucosa. Digestion 83 (Suppl. 1), 13–18 (2011).
Goldspink, D. A. et al. Mechanistic insights into the detection of free fatty and bile acids by ileal glucagon-like peptide-1 secreting cells. Mol. Metab. 7, 90–101 (2018).
Pais, R., Gribble, F. M. & Reimann, F. Signalling pathways involved in the detection of peptones by murine small intestinal enteroendocrine L-cells. Peptides 77, 9–15 (2016).
Emery, E. C. et al. Stimulation of glucagon-like peptide-1 secretion downstream of the ligand-gated ion channel TRPA1. Diabetes 64, 1202–1210 (2014).
Zhou, H. R. & Pestka, J. J. Deoxynivalenol (vomitoxin)-induced cholecystokinin and glucagon-like peptide-1 release in the STC-1 enteroendocrine cell model is mediated by calcium-sensing receptor and transient receptor potential ankyrin-1 channel. Toxicol. Sci. 145, 407–417 (2015).
Lieu, T. et al. The bile acid receptor TGR5 activates the TRPA1 channel to induce itch in mice. Gastroenterology 147, 1417–1428 (2014).
Parker, H. E. et al. Predominant role of active versus facilitative glucose transport for glucagon-like peptide-1 secretion. Diabetologia 55, 2445–2455 (2012).
Gorboulev, V. et al. Na+-D-glucose cotransporter SGLT1 is pivotal for intestinal glucose absorption and glucose-dependent incretin secretion. Diabetes 61, 187–196 (2012).
Schirra, J. et al. Gastric emptying and release of incretin hormones after glucose ingestion in humans. J. Clin. Invest. 97, 92–103 (1996).
Reimann, F. et al. Glucose sensing in L cells: a primary cell study. Cell. Metab. 8, 532–539 (2008).
Powell, D. R. et al. LX4211 increases serum glucagon-like peptide 1 and peptide YY levels by reducing sodium/glucose cotransporter 1 (SGLT1)-mediated absorption of intestinal glucose. J. Pharmacol. Exp. Ther. 345, 250–259 (2013).
Roberts, G. P. et al. Gastrectomy with Roux-en-Y reconstruction as a lean model of bariatric surgery. Surg. Obes. Relat. Dis. 14, 562–568 (2018).
Reimann, F. & Gribble, F. M. Glucose-sensing in glucagon-like peptide-1-secreting cells. Diabetes 51, 2757–2763 (2002).
Saltiel, M. Y. et al. Sweet taste receptor activation in the gut is of limited importance for glucose-stimulated GLP-1 and GIP secretion. Nutrients 9, 418 (2017).
Fujita, Y. et al. Incretin release from gut is acutely enhanced by sugar but not by sweeteners in vivo. Am. J. Physiol. Endocrinol. Metab. 296, E473–E479 (2009).
Rogers, G. J. et al. Electrical activity-triggered glucagon-like peptide-1 secretion from primary murine L-cells. J. Physiol. 589, 1081–1093 (2011).
Sun, E. W. et al. Mechanisms controlling glucose-induced GLP-1 secretion in human small intestine. Diabetes 66, 2144–2149 (2017).
Kuhre, R. E., Frost, C. R., Svendsen, B. & Holst, J. J. Molecular mechanisms of glucose-stimulated GLP-1 secretion from perfused rat small intestine. Diabetes 64, 370–382 (2015).
El-Ouaghlidi, A. et al. The dipeptidyl peptidase 4 inhibitor vildagliptin does not accentuate glibenclamide-induced hypoglycemia but reduces glucose-induced glucagon-like peptide 1 and gastric inhibitory polypeptide secretion. J. Clin. Endocrinol. Metab. 92, 4165–4171 (2007).
Beglinger, S. et al. Role of fat hydrolysis in regulating glucagon-like peptide-1 secretion. J. Clin. Endocrinol. Metab. 95, 879–886 (2010).
Sykaras, A. G., Demenis, C., Case, R. M., McLaughlin, J. T. & Smith, C. P. Duodenal enteroendocrine I-cells contain mRNA transcripts encoding key endocannabinoid and fatty acid receptors. PLOS ONE 7, e42373 (2012).
Parker, H. E., Habib, A. M., Rogers, G. J., Gribble, F. M. & Reimann, F. Nutrient-dependent secretion of glucose-dependent insulinotropic polypeptide from primary murine K cells. Diabetologia 52, 289–298 (2009).
Edfalk, S., Steneberg, P. & Edlund, H. Gpr40 is expressed in enteroendocrine cells and mediates free fatty acid stimulation of incretin secretion. Diabetes 57, 2280–2287 (2008).
Sankoda, A. et al. Long-chain free fatty acid receptor GPR120 mediates oil-induced gip secretion through CCK in male mice. Endocrinology 158, 1172–1180 (2017).
Psichas, A., Larraufie, P. F., Goldspink, D. A., Gribble, F. M. & Reimann, F. Chylomicrons stimulate incretin secretion in mouse and human cells. Diabetologia 60, 2475–2485 (2017).
Christensen, L. W., Kuhre, R. E., Janus, C., Svendsen, B. & Holst, J. J. Vascular, but not luminal, activation of FFAR1 (GPR40) stimulates GLP-1 secretion from isolated perfused rat small intestine. Physiol. Rep. 3, e12551 (2015).
Tough, I. R. et al. Bidirectional GPR119 agonism requires peptide YY and glucose for activity in mouse and human colon mucosa. Endocrinology 159, 1704–1717 (2018).
Tolhurst, G. et al. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes 61, 364–371 (2012).
Chimerel, C. et al. Bacterial metabolite indole modulates incretin secretion from intestinal enteroendocrine L cells. Cell Rep. 9, 1202–1208 (2014).
Lebrun, L. J. et al. Enteroendocrine L cells sense LPS after gut barrier injury to enhance GLP-1 secretion. Cell Rep. 21, 1160–1168 (2017).
Wichmann, A. et al. Microbial modulation of energy availability in the colon regulates intestinal transit. Cell Host Microbe 14, 582–590 (2013).
Arora, T. et al. Microbial regulation of the L cell transcriptome. Sci. Rep. 8, 1207 (2018).
Petersen, N. et al. Generation of L cells in mouse and human small intestine organoids. Diabetes 63, 410–420 (2014).
Brooks, L. et al. Fermentable carbohydrate stimulates FFAR2-dependent colonic PYY cell expansion to increase satiety. Mol. Metab. 6, 48–60 (2017).
Larraufie, P. et al. SCFAs strongly stimulate PYY production in human enteroendocrine cells. Sci. Rep. 8, 74 (2018).
Psichas, A. et al. The short chain fatty acid propionate stimulates GLP-1 and PYY secretion via free fatty acid receptor 2 in rodents. Int. J. Obes. (Lond.) 39, 424–429 (2014).
Nohr, M. K. et al. GPR41/FFAR3 and GPR43/FFAR2 as cosensors for short-chain fatty acids in enteroendocrine cells versus FFAR3 in enteric neurons and FFAR2 in enteric leukocytes. Endocrinology 154, 3552–3564 (2013).
Christiansen, C. B. et al. The impact of short chain fatty acids on GLP-1 and PYY secretion from the isolated perfused rat colon. Am. J. Physiol. Gastrointest. Liver Physiol. 315, G53–G65 (2018).
Kuhre, R. E. et al. Bile acids are important direct and indirect regulators of the secretion of appetite- and metabolism-regulating hormones from the gut and pancreas. Mol. Metab. 11, 84–95 (2018).
Kawamata, Y. et al. A G protein-coupled receptor responsive to bile acids. J. Biol. Chem. 278, 9435–9440 (2003).
Larraufie, P., Doré, J., Lapaque, N. & Blottière, H. M. TLR ligands and butyrate increase Pyy expression through two distinct but inter-regulated pathways. Cell. Microbiol. 19, e12648 (2017).
Drucker, D. J. & Yusta, B. Physiology and pharmacology of the enteroendocrine hormone glucagon-like peptide-2. Annu. Rev. Physiol. 76, 561–583 (2014).
Reijnders, D. et al. Effects of gut microbiota manipulation by antibiotics on host metabolism in obese humans: a randomized double-blind placebo-controlled trial. Cell Metab. 24, 63–74 (2016).
Mikkelsen, K. H. et al. Effect of antibiotics on gut microbiota, gut hormones and glucose metabolism. PLOS ONE 10, e0142352 (2015).
Lim, E. L. et al. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 54, 2506–2514 (2011).
Brereton, M. F. et al. Reversible changes in pancreatic islet structure and function produced by elevated blood glucose. Nat. Commun. 5, 4639 (2014).
Nauck, M., Stöckmann, F., Ebert, R. & Creutzfeldt, W. Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia 29, 46–52 (1986).
Meier, J. J. & Nauck, M. A. Incretins and the development of type 2 diabetes. Curr. Diab. Rep. 6, 194–201 (2006).
Cnop, M. et al. Longevity of human islet α- and β-cells. Diabetes Obes. Metab. 13 (Suppl. 1), 39–46 (2011).
Drucker, D. J., Jin, T. R., Asa, S. L., Young, T. A. & Brubaker, P. L. Activation of proglucagon gene-transcription by protein kinase-A in a novel mouse enteroendocrine cell-line. Mol. Endocrinol. 8, 1646–1655 (1994).
Tseng, C. C., Jarboe, L. A. & Wolfe, M. M. Regulation of glucose-dependent insulinotropic peptide gene expression by a glucose meal. Am. J. Physiol. 266, G887–G891 (1994).
Batterham, R. L. et al. Inhibition of food intake in obese subjects by peptide YY3-36. N. Engl. J. Med. 349, 941–948 (2003).
Færch, K. et al. GLP-1 response to oral glucose is reduced in prediabetes, screen-detected type 2 diabetes, and obesity and influenced by sex: the ADDITION-PRO Study. Diabetes 64, 2513–2525 (2015).
Richards, P. et al. High fat diet impairs the function of glucagon-like peptide-1 producing L-cells. Peptides 77, 21–27 (2015).
Dusaulcy, R. et al. Functional and molecular adaptations of enteroendocrine l-cells in male obese mice are associated with preservation of pancreatic α-cell function and prevention of hyperglycemia. Endocrinology 157, 3832–3843 (2016).
Rhee, N. A. et al. Effect of Roux-en-Y gastric bypass on the distribution and hormone expression of small-intestinal enteroendocrine cells in obese patients with type 2 diabetes. Diabetologia 58, 2254–2258 (2015).
Mumphrey, M. B., Patterson, L. M., Zheng, H. & Berthoud, H. R. Roux-en-Y gastric bypass surgery increases number but not density of CCK-, GLP-1-, 5-HT-, and neurotensin-expressing enteroendocrine cells in rats. Neurogastroenterol. Motil. 25, e70–79 (2013).
Larraufie, P. et al. Important role of the GLP-1 axis for glucose homeostasis after bariatric surgery. Cell Rep. 26, 1399–1408 (2019).
Jørgensen, N. B. et al. Acute and long-term effects of Roux-en-Y gastric bypass on glucose metabolism in subjects with Type 2 diabetes and normal glucose tolerance. Am. J. Physiol. Endocrinol. Metab. 303, E122–E131 (2012).
Svane, M. S. et al. Peptide YY and glucagon-like peptide-1 contribute to decreased food intake after Roux-en-Y gastric bypass surgery. Int. J. Obes. (Lond.) 40, 1699–1706 (2016).
Jørgensen, N. B. et al. Exaggerated glucagon-like peptide 1 response is important for improved β-cell function and glucose tolerance after Roux-en-Y gastric bypass in patients with type 2 diabetes. Diabetes 62, 3044–3052 (2013).
Wilson-Pérez, H. E. et al. Vertical sleeve gastrectomy is effective in two genetic mouse models of glucagon-like peptide 1 receptor deficiency. Diabetes 62, 2380–2385 (2013).
Garibay, D. et al. β-cell glucagon-like peptide-1 receptor contributes to improved glucose tolerance after vertical sleeve gastrectomy. Endocrinology 157, 3405–3409 (2016).
Ley, R. E., Turnbaugh, P. J., Klein, S. & Gordon, J. I. Microbial ecology: human gut microbes associated with obesity. Nature 444, 1022–1023 (2006).
Ley, R. E. et al. Obesity alters gut microbial ecology. Proc. Natl Acad. Sci. USA 102, 11070–11075 (2005).
Turnbaugh, P. J. et al. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 444, 1027–1031 (2006).
Ridaura, V. K. et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science 341, 1241214 (2013).
Liou, A. P. et al. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Sci. Transl Med. 5, 178ra141 (2013).
Kootte, R. S. et al. Improvement of insulin sensitivity after lean donor feces in metabolic syndrome is driven by baseline intestinal microbiota composition. Cell Metab. 26, 611–619 (2017).
Finucane, M. M., Sharpton, T. J., Laurent, T. J. & Pollard, K. S. A taxonomic signature of obesity in the microbiome? Getting to the guts of the matter. PLOS ONE 9, e84689 (2014).
Falony, G. et al. Population-level analysis of gut microbiome variation. Science 352, 560–564 (2016).
Gordon, H. A. & Pesti, L. The gnotobiotic animal as a tool in the study of host microbial relationships. Bacteriol. Rev. 35, 390–429 (1971).
Bhattarai, Y. & Kashyap, P. C. Germ-free mice model for studying host-microbial interactions. Methods Mol. Biol. 1438, 123–135 (2016).
Acknowledgements
The work of the authors is supported by the Wellcome Trust and the UK Medical Research Council.
Reviewer information
Nature Reviews Endocrinology thanks J. Campbell, D. Keating and other anonymous reviewers for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gribble, F.M., Reimann, F. Function and mechanisms of enteroendocrine cells and gut hormones in metabolism. Nat Rev Endocrinol 15, 226–237 (2019). https://doi.org/10.1038/s41574-019-0168-8
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-019-0168-8
This article is cited by
-
Microbiota–gut–brain axis and its therapeutic applications in neurodegenerative diseases
Signal Transduction and Targeted Therapy (2024)
-
Postprandial glucose metabolism in children and adolescents with type 1 diabetes mellitus: potential targets for improvement
European Journal of Clinical Nutrition (2024)
-
The gut microbiome modifies the associations of short- and long-term physical activity with body weight changes
Microbiome (2023)
-
Standard: Human intestinal organoids
Cell Regeneration (2023)
-
Gut enterochromaffin cells drive visceral pain and anxiety
Nature (2023)