Abstract
Cardiovascular disease (CVD) is the leading cause of death in China. To develop effective and timely strategies to cope with the challenges of CVD epidemics, we need to understand the current epidemiological features of the major types of CVD and the implications of these features for the prevention and treatment of CVD. In this Review, we summarize eight important features of the epidemiology of CVD in China. Some features indicate a transition in CVD epidemiology owing to interrelated changes in demography, environment, lifestyle, and health care, including the rising burden from atherosclerotic CVD (ischaemic heart disease and ischaemic stroke), declining mortality from haemorrhage stroke, varied regional epidemiological trends in the subtypes of CVD, increasing numbers of patients with moderate types of ischaemic heart disease and ischaemic stroke, and increasing ageing of patients with CVD. Other features highlight the problems that need particular attention, including the high proportion of out-of-hospital death of patients with ischaemic heart disease with insufficient prehospital care; the wide gaps between guideline-recommended goals and levels of lifestyle indicators; and the huge number of patients with undiagnosed, untreated, or uncontrolled hypertension, hypercholesterolaemia, or diabetes mellitus.
Key points
-
Eight important features of the epidemiology of cardiovascular disease (CVD) in China are identified in this Review.
-
An increasing burden of atherosclerotic CVD, declining mortality from haemorrhage stroke, and regional variations in CVD are features of the evolving epidemic of CVD.
-
An increasing number of patients with moderate types of ischaemic heart disease (IHD) or ischaemic stroke and the increasing age of patients have brought new challenges to CVD prevention and treatment.
-
The high proportion of out-of-hospital deaths of patients with IHD with insufficient prehospital care remains a problem with little improvement.
-
Despite some lifestyle indicators having shifted in a beneficial direction, the gaps between guideline-recommended targets and current levels of these indicators remain large.
-
A huge number of individuals have undiagnosed, untreated, or uncontrolled statuses for hypertension, hypercholesterolaemia, or diabetes mellitus.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Zhou, M. et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 387, 251–272 (2016).
Yang, G. et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 381, 1987–2015 (2013).
National Center for Cardiovascular Diseases. Report on Cardiovascular Diseases in China 2017 [Chinese] (Encyclopedia of China Publishing House, 2017).
Institute for Health Metrics and Evaluation (IHME). GBD Compare | Viz Hub. VizHub http://vizhub.healthdata.org/gbd-compare (2018).
Wright, P. Yingkai Wu–obituary. Lancet 363, 575–575 (2004).
Bothig, S. WHO MONICA project: objectives and design. Int. J. Epidemiol. 18, S29–S37 (1989).
Wu, Z. et al. Sino-MONICA project: a collaborative study on trends and determinants in cardiovascular diseases in China, part I: morbidity and mortality monitoring. Circulation 103, 462–468 (2001).
Zhao, D. et al. Epidemiological transition of stroke in China: twenty-one-year observational study from the Sino-MONICA-Beijing project. Stroke 39, 1668–1674 (2008).
Tunstall-Pedoe, H. et al. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet 353, 1547–1557 (1999).
Lewington, S. et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern. Med. 176, 524–532 (2016).
Li, H. & Ge, J. Cardiovascular diseases in China: current status and future perspectives. Int. J. Cardiol. Heart Vasc. 6, 25–31 (2015).
Li, Y. et al. Can China achieve a one-third reduction in premature mortality from non-communicable diseases by 2030? BMC Med. 15, 132 (2017).
Yang, W. Y. et al. Prevalence of diabetes among men and women in China. N. Engl. J. Med. 362, 1090–1101 (2010).
Institute for Health Metrics and Evaluation (IHME). GBD results tool. GHDx http://ghdx.healthdata.org/gbd-results-tool (2018).
UNC Carolina Population Center. Data Sets. CHNS http://www.cpc.unc.edu/projects/china/data/datasets/index.html (2018).
World Health Organisation. Global Health Observatory (GHO) data. WHO http://www.who.int/gho/countries/chn/country_profiles/en/ (2018).
Volgman, A. S. et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation 138, e1–e34 (2018).
Chinese Society of Cardiology of Chinese Medical Association, Editorial Board of Chinese Journal of Cardiology. Chinese guidelines for prevention of cardiovascular diseases [Chinese]. Zhonghua Xin Xue Guan Bing Za Zhi 46, 10–25 (2018).
Stone, N. J. et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. Circulation 129, S1–S45 (2014).
Zhao, D., Liu, J., Xie, W. & Qi, Y. Cardiovascular risk assessment: a global perspective. Nat. Rev. Cardiol. 12, 301–311 (2015).
Tunstall-Pedoe, H. et al. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation 90, 583–612 (1994).
Zhang, G. et al. Burden of ischaemic heart disease and attributable risk factors in China from 1990 to 2015: findings from the global burden of disease 2015 study. BMC Cardiovasc. Disord. 18, 18 (2018).
Wang, W. et al. Prevalence, Incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation 135, 759–771 (2017).
Krishnamurthi, R. V. et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet Glob. Health 1, e259–e281 (2013).
Wang, C. et al. Significant underuse of warfarin in patients with nonvalvular atrial fibrillation: results from the China national stroke registry. J. Stroke Cerebrovasc. Dis. 23, 1157–1163 (2014).
Gao, Q. et al. Use of oral anticoagulation among stroke patients with atrial fibrillation in China: the ChinaQUEST (Quality evaluation of stroke care and treatment) registry study. Int. J. Stroke 8, 150–154 (2013).
Longde, W. et al. Fixed-dose combination treatment after stroke for secondary prevention in China: a national community-based study. Stroke 46, 1295–1300 (2015).
Wang, X. et al. Prevalence of atrial fibrillation in different socioeconomic regions of China and its association with stroke: Results from a national stroke screening survey. Int. J. Cardiol. 271, 92–97 (2018).
Yang, X. et al. Atrial fibrillation is not uncommon among patients with ischemic stroke and transient ischemic stroke in China. BMC Neurol. 17, 207 (2017).
Wang, W. et al. Trend of declining stroke mortality in China: reasons and analysis. Stroke Vasc. Neurol. 2, 132–139 (2017).
Jiang, Y. et al. Construction of China cardiovascular health index. BMC Publ. Health 18, 937 (2018).
GBD 2013 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990-2013: quantifying the epidemiological transition. Lancet 386, 2145–2191 (2015).
GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1151–1210 (2017).
Moran, A. et al. Future cardiovascular disease in china: markov model and risk factor scenario projections from the coronary heart disease policy model-china. Circ. Cardiovasc. Qual. Outcomes 3, 243–252 (2010).
Moran, A. et al. The future impact of population growth and aging on coronary heart disease in China: projections from the Coronary Heart Disease Policy Model-China. BMC Publ. Health 8, 394 (2008).
Fulcher, J. et al. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet 385, 1397–1405 (2015).
Brunstrom, M. & Carlberg, B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern. Med. 178, 28–36 (2018).
Rafique, A. M. et al. Optimal P2Y12 inhibitor in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: a network meta-analysis. JACC Cardiovasc. Interv. 9, 1036–1046 (2016).
Tisminetzky, M., Goldberg, R. & Gurwitz, J. H. Magnitude and impact of multimorbidity on clinical outcomes in older adults with cardiovascular disease: a literature review. Clin. Geriatr. Med. 32, 227–246 (2016).
Boyd, C. M. & Kent, D. M. Evidence-based medicine and the hard problem of multimorbidity. J. Gen. Intern. Med. 29, 552–553 (2014).
Stefanidis, K. B., Askew, C. D., Greaves, K. & Summers, M. J. The effect of non-stroke cardiovascular disease states on risk for cognitive decline and dementia: a systematic and meta-analytic review. Neuropsychol. Rev. 28, 1–15 (2018).
Stampfer, M. J. Cardiovascular disease and Alzheimer’s disease: common links. J. Intern. Med. 260, 211–223 (2006).
Amsterdam, E. A. et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. Circulation 130, 2354–2394 (2014).
Chinese Society of Cardiology, Editorial Board of Chinese Journal of Cardiology. CSC guidelines for the diagnosis and treatment of acute coronary syndromes in patients presenting without persistent ST-segment elevation [Chinese]. Chinese J. Cardiol. 5, 18 (2017).
European Society of Cardiology. Recent hospitalization trends for acute myocardial infarction in Beijing. Eur. Heart J. 37, 3188–3189 (2016).
Zhang, Q. et al. Recent trends in hospitalization for acute myocardial infarction in Beijing: increasing overall burden and a transition from ST-segment elevation to non-ST-segment elevation myocardial infarction in a population-based study. Medicine (Baltimore) 95, e2677 (2016).
Yang, Q. et al. Invasive management strategies and antithrombotic treatments in patients with non-ST-segment-elevation acute coronary syndrome in China: findings from the improving CCC project (Care for Cardiovascular Disease in China). Circ. Cardiovasc. Interv. 10, e004750 (2017).
Gomez, C. R., Schneck, M. J. & Biller, J. Recent advances in the management of transient ischemic attacks. F1000Res 6, 1893 (2017).
Wang, Y. et al. Prevalence, knowledge, and treatment of transient ischemic attacks in China. Neurology 84, 2354–2361 (2015).
Wang, L. et al. Factors associated with delayed presentation in patients with TIA and minor stroke in China: analysis of data from the China National Stroke Registry (CNSR). Neurol. Res. 35, 517–521 (2013).
Wang, M. et al. Cost-effectiveness of optimal use of acute myocardial infarction treatments and impact on coronary heart disease mortality in China. Circ. Cardiovasc. Qual. Outcomes 7, 78–85 (2014).
Zhao, D. The epidemiology of coronary heart disease (CHD) in 16 provinces of China. Multi-province cooperative group of cardiovascular disease surveillance (MONICA Project) [Chinese]. Zhonghua Liu Xing Bing Xue Za Zhi 14, 10–13 (1993).
Gao, Y. L. et al. Characteristics of out-of-hospital acute coronary heart disease deaths of Beijing permanent residents at the age of 25 or more from 2007 to 2009 [Chinese]. Chinese. J. Cardiol. 40, 4 (2012).
Wan, H. et al. The epidemiology of out-of-hospital deaths due to acute coronary events in young Beijing adults [Chinese]. Zhonghua Nei Ke Za Zhi 51, 274–278 (2012).
Shao, F., Li, C. S., Liang, L. R., Li, D. & Ma, S. K. Outcome of out-of-hospital cardiac arrests in Beijing. Resuscitation 85, 1411–1417 (2014).
Liu, X. Improvement of treatment strategy for acute myocardial infarction by chest pain center and regional synergy system [Chinese]. Chinese Circul. J. 33, 830–832 (2018).
Chinese Chest Pain Center Accreditation Working Committee. The impacts of the chest pain center accreditation on the efficacy of pre-hospital care in patients with ST-segment elevation myocardial infarction [Chinese]. Chinese J. Front. Med. Sci. 9, 11–15 (2017).
Bennett, D. A. et al. Association of physical activity with risk of major cardiovascular diseases in Chinese men and women. JAMA Cardiol. 2, 1349–1358 (2017).
Chen, Z. et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet 386, 1447–1456 (2015).
Du, H. et al. Fresh fruit consumption and major cardiovascular disease in China. N. Engl. J. Med. 374, 1332–1343 (2016).
Lv, J. et al. Adherence to healthy lifestyle and cardiovascular diseases in the Chinese population. J. Am. Coll. Cardiol. 69, 1116–1125 (2017).
Wang, Y. et al. Lifetime risk for cardiovascular disease in a Chinese population: the Chinese multi-provincial cohort study. Eur. J. Prev. Cardiol. 22, 380–388 (2015).
Wang, Y. et al. Lifetime risk of stroke in young-aged and middle-aged Chinese population: the Chinese multi-provincial cohort study. J. Hypertens. 34, 2434–2440 (2016).
Bi, Y. et al. Status of cardiovascular health in Chinese adults. J. Am. Coll. Cardiol. 65, 1013–1025 (2015).
Li, Y. et al. Potential impact of time trend of life-style factors on cardiovascular disease burden in China. J. Am. Coll. Cardiol. 68, 818–833 (2016).
Chinese Nutrition Society. Dietary Guidelines for Chinese Residents [Chinese] Ch. 1, page 3 (People’s Medical Publishing House, 2016).
Wang, Z. et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation 137, 2344–2356 (2018).
Lu, J. et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet 390, 2549–2558 (2017).
National Bureau of Disease Prevention and Control of the National Health Commission. Report on the Nutrition and Chronic Disease Status of Chinese Residents [Chinese] Ch. 5, Section 5, page 55 (People’s Medical Publishing House, 2015).
Wang, L. Report on the Nutrition and Health Status of Chinese Residents [Chinese] Ch. 2, Section 6, page 61 (People’s Medical Publishing House, 2002).
Zhang, M. et al. Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults: a nationally representative survey of 163,641 adults. Int. J. Cardiol. 260, 196–203 (2018).
Li, J. et al. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet 385, 441–451 (2015).
Yusuf, S. et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet 378, 1231–1243 (2011).
Stevens, W. et al. Estimating the future burden of cardiovascular disease and the value of lipid and blood pressure control therapies in China. BMC Health Serv. Res. 16, 175 (2016).
The World Bank: Human Development Unit: East Asia and Pacific Region. Toward a healthy and harmonious life in china: stemming the rising tide of non-communicable diseases. The World Bank http://www.worldbank.org/content/dam/Worldbank/document/NCD_report_en.pdf (2011).
Lu, Y. et al. Comparison of prevalence, awareness, treatment, and control of cardiovascular risk factors in China and the United States. J. Am. Heart Assoc. 7, e007462 (2018).
Xu, Y. et al. Prevalence and control of diabetes in Chinese adults. JAMA 310, 948–959 (2013).
Zhou, B. et al. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 387, 1513–1530 (2016).
Su, M. et al. Availability, cost, and prescription patterns of antihypertensive medications in primary health care in China: a nationwide cross-sectional survey. Lancet 390, 2559–2568 (2017).
Acknowledgements
Reviewer information
Nature Reviews Cardiology thanks Y. Zhang and the other anonymous reviewer(s), for their contribution to the peer review of this work.
Review criteria
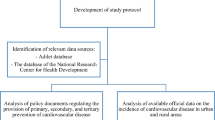
Articles were identified using the online PubMed database, citation tracking, books, and open database of websites. The search scope was confined mostly to articles in the English language, but also included articles in Chinese. The disease-related search terms included: “cardiovascular disease”, “ischemic heart disease”, “coronary heart disease”, “acute coronary syndrome”, “myocardial infarction”, “stroke”, “cerebral haemorrhage”, “cerebral infarction”, and their synonyms, variations, or abbreviations; other search terms included “death”, “mortality”, “prevalence”, “incidence”, “disease burden”, and “epidemiology”. Risk factor-related search terms included: “hypertension”, “diabetes”, “diabetic”, “obesity”, “dyslipidemia”, “smoke”, and their synonyms or variations; “prevalence”, “control”, “treatment”, and “epidemiology”.
Author information
Authors and Affiliations
Contributions
D.Z., X.Z., and M.Z. researched data for the article, and all the authors discussed its content. D.Z. wrote the manuscript, and all the authors reviewed and edited it before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, D., Liu, J., Wang, M. et al. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol 16, 203–212 (2019). https://doi.org/10.1038/s41569-018-0119-4
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-018-0119-4
This article is cited by
-
Joint association of physical activity and diet quality with dyslipidemia: a cross-sectional study in Western China
Lipids in Health and Disease (2024)
-
Beneficial effects of time-restricted fasting on cardiovascular disease risk factors: a meta-analysis
BMC Cardiovascular Disorders (2024)
-
Relationship between triglyceride-glucose index baselines and trajectories with incident cardiovascular diseases in the elderly population
Cardiovascular Diabetology (2024)
-
CVD phenotyping in oncologic disorders: cardio-miRNAs as a potential target to improve individual outcomes in revers cardio-oncology
Journal of Translational Medicine (2024)
-
Characteristics and correlation of body fat distribution and brachial-ankle pulse wave velocity in adults aged 20–59 years: a cross-sectional study
BMC Cardiovascular Disorders (2024)