Abstract
Visceral leishmaniasis (VL), a deadly parasitic disease, is a major public health concern globally. Countries affected by VL have signed the London Declaration on Neglected Tropical Diseases and committed to eliminate VL as a public health problem by 2020. To achieve and sustain VL elimination, it will become progressively important not to miss any remaining cases in the community who can maintain transmission. This requires accurate identification of symptomatic and asymptomatic carriers using highly sensitive diagnostic tools at the primary health service setting. The rK39 rapid diagnostic test (RDT) is the most widely used tool and with its good sensitivity and specificity is the first choice for decentralized diagnosis of VL in endemic areas. However, this test cannot discriminate between current, subclinical, or past infections and is useless for diagnosis of relapses and as a prognostic (cure) test. Importantly, as the goal of elimination of VL as a public health problem is approaching, the number of people susceptible to infection will increase. Therefore, correct diagnosis using a highly sensitive diagnostic test is crucial for applying appropriate treatment and management of cases. Recent advances in molecular techniques have improved Leishmania detection and quantification, and therefore this technology has become increasingly relevant due to its possible application in a variety of clinical sample types. Most importantly, given current problems in identifying asymptomatic individuals because of poor correlation between the main methods of detection, molecular tests are valuable for VL elimination programs, especially to monitor changes in burden of infection in specific communities. This review provides a comprehensive overview of the available VL diagnostics and discusses the usefulness of molecular methods in the diagnosis, quantification, and species differentiation as well as their clinical applications.
Similar content being viewed by others
Due to the limited number of currently available anti-leishmanial drugs, effective clinical management, chemotherapy, and control of transmission depend largely on early and unequivocal diagnosis. Any patient residing in a visceral leishmaniasis (VL) endemic area presenting with a history of fever of more than 2 weeks’ duration and with no response to antibiotics/antimalarials should be tested for VL with an rK-39 dipstick test. |
The rK39 rapid diagnostic test (RDT), used within strict clinical criteria, is currently used with good results for diagnosis of VL, but this test cannot differentiate between active disease and past VL. Furthermore, a diagnostic algorithm of the rK39 RDT for detection of asymptomatic infection has only been validated for high-incidence settings in strict combination with clinical criteria (fever for more than 2 weeks’ duration plus an enlarged spleen). |
With the advent of technology, highly specific and sensitive molecular-based tools have been developed for detecting infection, diagnosis, and species differentiation and hold considerable further promise for delivering better point-of-care diagnostic tests in the elimination and post-elimination setting. |
Molecular-based methods play a key role in early diagnosis, monitoring of treatment effectiveness, and assessment of drug resistance in Leishmania parasites. |
1 Introduction
Leishmaniasis has been identified as high-priority disease by the World Health Organization (WHO) [1]. It is caused by protozoa belonging to the genus Leishmania and transmitted by the bite of a 2–3 mm long insect vector, the phlebotomine sand fly found throughout the world’s inter-tropical and temperate regions [2]. Around 21 species of Leishmania are known to be pathogenic to humans [3].The disease occurs in three forms: self-healing or chronic cutaneous leishmaniasis (CL), mutilating mucosal or muco-cutaneous leishmaniasis (ML or MCL), and life-threatening visceral leishmaniasis (VL). Each form varies in degree of severity, with VL being by far the most devastating with the highest mortality.
VL, also known as kala-azar, the most severe form of leishmaniasis, is caused by the obligate intracellular protozoan parasites Leishmania donovani/L. infantum. It is estimated by the WHO that 200,000–400,000 new cases of VL occur annually worldwide, 90% of which occur in three geographical regions: (1) South-East Asia—India (especially Bihar), Bangladesh, and Nepal; (2) Latin America—mainly north-eastern Brazil; and (3) East Africa—Sudan, Ethiopia, Kenya, Uganda, and Somalia [4,5,6,7]. In the Indian subcontinent (ISC), VL is now being reported in 54 districts in India, 16 upazila (administrative regions) in Bangladesh, and 12 districts in Nepal [8]. In Europe, VL is endemic in nine countries, accounting for less than 2% of the global burden [9]. In Brazil, VL is endemic in 21 of 26 states and a total of 14,859 cases were reported between 2001 and 2014 in 25% of Brazilian municipalities [10]. However, in Africa-VL is endemic in 17 localities in seven states in Sudan [11] and 6 regional states in Ethiopia.
The Leishmania parasite is transmitted by female Phlebotomine sand flies as a flagellated, metacyclic promastigote, which is phagocytized by host macrophages and then differentiates into the non-flagellated, replicative amastigotes [12]. The organs commonly affected during VL are the bone marrow, liver, and spleen [12]. Thus, clinical symptoms include hepatosplenomegaly, which is characterized by an enlarged abdomen with a palpable spleen and liver. Other symptoms include long-term, low-grade fever, muscle wasting, anemia, leukopenia, polyclonal hyper-gammaglobulinemia, and weight loss [13, 14]. If left untreated, it has a mortality rate of almost 100%. During an epidemic in the early 1990s in Sudan, there were an estimated 100,000 deaths. Risk of an epidemic still exists in the horn of Africa, at the junction of Eritrea, Ethiopia and Sudan, a highly endemic region where tens of thousands of refugees, returnees, and agricultural workers have been resettled. Especially in Sudan, Ethiopia, Kenya, Uganda, and Somalia, VL is the cause of much morbidity and mortality, and only a small minority of patients have access to diagnosis and treatment [15]. VL is endemic in several tropical and subtropical regions and has been reported in 56 countries around the world (Fig. 1). Importantly, the disease affects mostly poverty-stricken people, with over 80% of patients living below the poverty threshold (daily income of less than US$1) whose source of income is agriculture and/or animal husbandry [16]. More than 75% live in mud or grass-covered houses. These patients are thus completely dependent on charity or public health services for diagnosis or treatment, and these remain grossly deficient in endemic areas [17, 18].
Importantly, the three countries affected by VL on the Indian subcontinent, India, Nepal and Bangladesh, aspired to eliminate VL by 2015 (a deadline later reset to 2020). The aim is to reduce the incidence to less than 1 per 10,000 of population at the sub-districts level (i.e., block level in India and Nepal and upazila level in Bangladesh) through early diagnosis, complete treatment of cases, and integrated vector management [19]. However, as countries move towards elimination goals, the number of VL and post-kala-azar dermal leishmaniasis (PKDL) (characterized by skin lesions in which parasites can be identified, in a patient who is otherwise fully recovered from VL) cases will decrease, and a low number of such cases will almost inevitably lead to a decreasing awareness in the communities and by health providers. If cases of VL and PKDL are ignored or missed in such a context, a new epidemic phase may start. To avoid such a scenario, there is need for development and validation of an innovative set of tools to find cases of VL and PKDL, along with an outbreak management strategy, and surveillance methods for the measurement of infection. Thus, there is a direct need for new technology for the monitoring of infections, treatment effectiveness, and drug resistance because such validated methods under routine conditions do not exist. Molecular detection tools would constitute a more rapid and high-throughput alternative to detect parasites. In this review, we discuss the various molecular methods, focusing on recent developments and their clinical application in Leishmania detection, absolute quantification, species differentiation, and phylogenetic analysis.
2 Standard Diagnostic Tools and Their Limitations
A major challenge in the clinical management of VL is the weakness of health systems at the primary health centre (PHC) level in many affected countries, with multiple challenges and numerous constraints [8, 20]. Despite multiple techniques for confirming VL cases being available, they are all still far from being ideal. To date, observation of parasites in splenic aspirate is considered the gold standard for VL diagnosis [21]. While microscopic examination of spleen aspirates is a rapid and cheap approach with high sensitivity and specificity, it is not practical at the PHC level. However, in Kenya, VL policy specifies that all serologically proven leishmaniasis be confirmed by spleen aspirate, a procedure that can only be performed in referral hospitals [22]. Alternative parasitological diagnostic techniques are the lymph node or bone marrow aspirates (reviewed in Singh and Sundar [23]), the standard means of diagnosing VL in most countries. Sensitivity of such diagnostic methods is highly variable and dependent on the sampling procedure and technical skills of the physician or personnel performing the tests. Although sensitivity of bone marrow is lower than splenic aspiration, the diagnostic potential in combination with serology is adequate for clinical purposes [24, 25]. Again, these methods cannot be performed at the PHC setting in endemic areas because they require skilled personnel, have a high cost, and are less simple. Most importantly, examination of bone marrow/splenic aspirates is now only recommended when the rK39 rapid diagnostic test (RDT) is negative but the suspicion of VL disease is high or in VL patients diagnosed by rK39 who do not respond to first-line treatment [23]. Notably, very few practitioners currently have the skills to perform these dangerous aspirates and very limited numbers of these biopsies are taken in the Indian subcontinent. Culturing Leishmania promastigotes from tissue biopsies/peripheral blood mononuclear cell/whole blood is another method of diagnosis but is expensive and requires a sophisticated laboratory [26].
Human VL is associated with high level of plasma antibodies; however, although it is useful in diagnosis, the role of antibodies in VL pathogenesis is not clear [27, 28]. A number of non-invasive serological tests to detect Leishmania antibodies are now available. The Direct Agglutination Test (DAT) has been extensively validated in endemic areas and is recommended by the WHO for VL control programs [21, 29]; however, the requirements of relatively specific material and expertise make its use difficult in peripheral health centers. Similarly, the Indirect Immunofluorescent Antibody Test (IFAT) requires an immune-fluorescence microscope, which restricts its use to referral hospitals. Hope is now directed at a rapid immunochromatographic test based on a recombinant 39-amino acid repeat antigen (rK39 dipstick), which, despite the variability initially observed among different producers and countries, seems to be the first choice for decentralized diagnosis of VL and has good sensitivity and specificity [30, 31]; however, it shows decreased sensitivity in East Africa when compared with the Indian subcontinent [31, 32]. The rK39 dipstick is stable, easy to use, and is a ‘rapid test’ (results available in 10 min). Performance of this test has been comprehensively reviewed in various studies recently [23, 24, 31]. In India, Bangladesh, and Nepal, the VL elimination initiative has adopted the rK39 RDT as its main tool, but it has significant limitations as it cannot be used to diagnose relapses or to assess response to treatment (test of cure) [23, 33]. Approximately 10–20% of healthy people living in endemic areas test positive with the rK39 RDT [34, 35]. Importantly, despite its limitations, the rK39 RDT has been, and is still, a great asset in the struggle against VL as it allows diagnosis and treatment to be decentralized to as close as possible to the villages where patients live. However, although the rK39 RDT test represents a sound approach in highly endemic areas, this is not the case in situations of low infection intensity. Furthermore, these antibody detection tests are of limited used in immunocompromised patients (i.e., HIV co-infection) [23]. Antigen detection is required as a means of identifying symptomatic infections in immunocompetent and immunocompromised patients (e.g., diagnosis of primary VL in Sudan where rK39 RDTs lack sensitivity and complex diagnosis of VL relapse is required) and as an indicator of cure. The latex agglutination test (KAtex; Kalon Biological, Guildford, UK) detects the leishmanial antigen in urine and records the results in a scoring system that correlates well with the parasite load. However, KAtex is currently not considered to be an ideal test as it had poor sensitivity when tested at different centers [32, 36,37,38].
2.1 Molecular Diagnosis and Detection of Infection
Most Leishmania species have been sequenced, revealing an overall conservation of gene order, chromosome structure, and discrete differences in gene content. These recent research advancements have helped in the development of more appropriate rapid molecular diagnostic devices and platforms [39]. However, despite the technological development, there is a huge difference in using a commercially available and standardized molecular diagnostic as opposed to in-house kits. So far, several molecular methods have been developed for detection, identification, quantification, and phylogenetic analysis, and these are summarized in Fig. 2.
Molecular tools and markers for diagnosis of visceral leishmaniasis. A2 amastigote stage gene, cpb cysteine protease B, EF1 elongation factor-1, ELISA enzyme-linked immunosorbent assay, G6PD glucose-6-phosphate dehydrogenase, HSP heat-shock protein, hsp70 heat-shock protein 70, kDNA kinetoplast DNA, LAMP loop-mediated isothermal amplification, MALDI-TOF Matrix assisted laser desorption ionization - time of flight, MLEE multilocus enzyme electrophoresis, MLMT multilocus microsatellite typing, NGS next generation sequencing, NASBA nucleic acid sequence-based amplification, OligoC oligochromatography test, PCR polymerase chain reaction, polA DNA polymerase α, RAPD random amplified polymorphic DNA, SNP single nucleotide polymorphism
The development of polymerase chain reaction (PCR) kits has provided one of the most sensitive and specific methods for diagnosis of clinical VL; they amplify parasite DNA and can be visually read without sophisticated equipment [44, 78,79,80]. The sensitivity of the PCR assay mostly depends on the biological sample (e.g., blood, bone marrow, splenic fluids, etc.) and the primers used to amplify the target sequence (variable or conserved target region) [81, 82]. The most commonly used amplification targets are nuclear DNA such as the small subunit ribosomal RNA (SSU rRNA) gene [45, 83, 84], extra-chromosomal DNA such as repetitive kinetoplastid DNA (kDNA) [45, 46, 85], mini-exon genes [86], and the ribosomal internal transcribed spacer (ITS) region [52]. A comparative overview of frequently used PCR targets and its sensitivity and specificities in different tissue samples are summarized in Table 1. One of the major limitation of DNA based PCR is the counting dead parasite DNA (as half life of DNA is 24 h within the body, which is still controversial and not proven); thus, RNA based amplification target is preferred [82, 87]. However, reliable RNA extraction is difficult in PHC settings. Srivastava et al. [44] validated 18S rRNA-based PCR in the blood of the largest number of patients and controls in their study, and found a sensitivity of 87.8% (95% confidence interval [CI] 84.1–89.8) and specificity of 94.6% (95% CI 92.8–96.1). Leishmanial DNA has been detected by PCR in the peripheral blood of persons with asymptomatic infection in Brazil and this was also documented recently in India and Nepal [88,89,90]. Several cohort studies conducted in India, Nepal, Bangladesh, Italy, Ethiopia, Sudan, and Brazil for detection of asymptomatic L. donovani infection in endemic villages has confirmed the increased capacity of PCR tests to detect infection in healthy individuals [89,90,91,92,93,94]. PCR assays have also been performed using non-invasive samples, such as buccal swabs and urine, with sensitivity of 79–83 and 88–97%, respectively [95, 96]. Molecular diagnosis using PCR is very useful in HIV–VL patients in whom the clinical picture is confusing and serological as well as immunological tests are not reliable due to low sensitivity [97]. Furthermore, sensitivity and specificity of PCR for detection of low-level parasitemia have been shown to be improved significantly by performing nested and semi-nested PCR, which involves two sets of primers (targeting a single gene locus) used in two successive runs. The second set of primers amplify the secondary target within the product of the first PCR product [49] but nested PCRs are prone to contamination and are not recommended except in accredited laboratories. The sensitivity and specificity of nested PCR using SSU-rRNA in the diagnosis of VL are reported to be 97% and 100%, respectively [98]. Similarly, multiplex PCR involves amplification of different DNA targets at the same time [99]. Although such assays are more sensitive than conventional PCR, their high costs make this test inappropriate in a field setting. Other forms of PCR such as the OligoC-TesT (Coris BioConcept, Gemblous, Belgium) [100], PCR-ELISA (enzyme-linked immunosorbent assay) [101], and nucleic acid sequence-based amplification (NASBA) have been developed and found to be more sensitive than conventional PCR [43]. More recently, rapid and highly specific loop-mediated isothermal amplification (LAMP) has emerged as a powerful tool for point-of-care diagnosis and has been validated in VL and PKDL in several countries [102, 103]. One of the advantages of this assay is that the test can be performed without the need for sophisticated equipment, making it a more attractive tool for field-based diagnosis. This assay is more rapid and cost effective than conventional PCR, but is limited in utility due to false positivity. Importantly, PCR-oligochromatography and LAMP are the only tests available commercially and this offers huge benefits over in-house kits in terms of reliability—of course, this comes at a price. Most recently, a recombinase polymerase amplification (RPA) assay (a simple and molecular assay as a mobile suitcase laboratory) was developed for canine VL [104]. This assay has also been tested and proved a promising diagnostic method for VL, which would significantly decrease the cost associated with testing [105].
Importantly, in view of mounting drug pressure, PCR diagnostic assays play a key role in monitoring drug efficacy and early reporting of drug resistance, which are essential to bring corrective actions in drug policy; this is even more important when the drug arsenal is limited, as in the case of VL [122,123,124]. The molecular assays are the only standard, rapid, high-throughput, and easy methods to track parasite resistance that can completely replace tedious in vitro susceptibility assays. Furthermore, such tools should be as simple as possible to be applicable and affordable in endemic countries. Recently, Srivastava et al. [125] identified a single nucleotide polymorphism in the cysteine proteinase B (cpb) gene that is associated with amphotericin B drug resistance.
2.2 Quantification of Parasites (Severity of Disease)
As an analytical technique, the conventional PCR method has some limitations. By first amplifying the DNA sequence and then analyzing the product, quantification is exceedingly difficult as the PCR gives rise to essentially the same amount of product independent of the initial amount of DNA template molecules that were present. Therefore, a conventional PCR (qualitative analysis) test shows only the presence or absence of Leishmania without quantification of the parasite load. With the highly efficient detection chemistry, sensitive instrumentation, and optimized assays that are available today in real-time PCR (also known as quantitative real-time PCR if DNA is the starting genetic material for quantification of parasites), the number of DNA molecules of a particular sequence in a complex sample can be determined with unprecedented accuracy and sensitivity that is sufficient to detect a single molecule. However, quantitative PCR (qPCR) does not directly measure the number of viable parasites circulating in the blood, but rather the amount of circulating parasite DNA. Therefore, sensitivity of qPCR depends on the assay design (primer and target region), chemistry used (SYBER® Green [Sigma-Aldrich, St Louis, MO, USA] or TaqMan® [Life Technologies, Foster City, CA, USA]), nature of clinical samples (blood, skin, bone marrow, or splenic fluids), and the DNA extraction methods (manual vs. commercial kits) [126] (Table 2). Using this technique, it was earlier demonstrated that the simultaneous quantitative evaluation of Leishmania DNA and cytokines by real-time PCR assay allows prediction of the development of disease in asymptomatic infected dogs [127]. Using qPCR, we have shown that the parasite load decreases during treatment in VL cases. Amplification of the 18Sr RNA gene sequence from a small volume of heparinized whole blood using real-time PCR revealed a wide range of blood parasitemia in VL patients prior to treatment that in each case began to decline within a few days of the start of their anti-leishmanial drug therapy [128], and thus can be used as a marker of treatment response as well as a measure of parasitic burden over time. Recently, Hossain et al. [129] evaluated the use of real-time PCR and revealed the difference in parasite loads between primary VL and relapse VL. Subsequently, in a larger cohort of asymptomatic subjects, we established the threshold of parasitemia (> 5 L. donovani parasite genomes detected/mL) in blood for clinical symptoms of VL to occur [61]. Later, in an enlarged cohort of 1606 healthy individuals, of whom 442 were recent sero-converters with DAT and/or rK39, the risk for progression of disease was found to be much higher in qPCR-positive patients (odds ratio 14.8, 95% CI 5.1–42.5) (Chakravarty et al., personal communication).
Elevated levels of interleukin (IL)-10 during active disease is a hallmark of VL, and this overproduction of IL-10 promote parasite replication and disease progression. Verma et al. [145] evaluated the parasitic burden measured by qPCR and its association with IL-10 production in VL and found that high qPCR load strongly correlates with plasma IL-10 levels, making it suitable for a biomarker of disease severity. Later, Wilson’s group developed several qPCR methods and strategies for Leishmania species differentiation and quantification in clinical specimens [63]. Leon et al. [146] evaluated the analytical performance of qPCR methods (designed on primers directed at kDNA, HSP70, 18S, and ITS-1 targets) and found that the 18S marker presented the highest sensitivity and specificity [146].
A qPCR assay usually provides a measure of the parasite load of blood at a given timepoint, but it remains unclear how this load can be correlated to the load at infection because the parasite load may vary with time, and likely reflects both host parasite interactions as well as the initial load. A number of researchers use PCR-ELISA for early detection and quantification, which allows multiple sample testing using whole blood, with a sensitivity of 87% [101, 147]. However, this method is tedious, expensive, and less sensitive than qPCR and has been tested on a limited number of clinical samples [101, 148].
2.3 Species Identification
VL is the most common Leishmania disease in the Indian subcontinent; however, recent identification of CL patients in Rajasthan (caused by L. tropica) and Himachal Pradesh (caused by L. donovani and L. tropica) [149,150,151] suggest that the clinical profile of CL is different in these states. Therefore, species identification assays are useful in such areas for proper management of the control programs. Importantly, in the Indian subcontinent (mainly India and Bangladesh) as well as in Africa (mainly Sudan), where L. donovani is the causative parasite for VL, a common complication of VL is PKDL [152]; it occurs in up to 50% of people who have recovered from VL in the months following treatment. It is much less common in India, with an incidence of less than 5–10%, and when it does occur, it does so many years after the acute infection [153]. In Africa, PKDL is even more common, but there are important intra-regional differences. It is most common in Sudan: up to 50–60% of VL cases develop PKDL, usually within 6 months, and virtually all cases develop within 12 months (mean 4.5 months). In Ethiopia, Kenya, and Uganda, PKDL is less common for reasons that are not well-understood.
Through whole-genome sequencing, Downing et al. [71] reported that there are a large number of chromosome copy number variations between L. donovani strains and other Leishmania species on the Indian subcontinent [71]. Therefore, better characterization of the parasite strain (i.e., species differentiation) is needed to resolve the mystery of whether the disease is due to reactivation of persistent parasites following clinical cure of VL or re-infection, and also to establish the cause of different forms of PKDL.
Commonly used target genes in Leishmania for species identification includes ITS (non-coding spacer DNA located between the 18S rRNA and 5.8S rRNA) [52, 154,155,156], repetitive nuclear DNA sequences [157], cytochrome-b genes [158, 159], mini-exon genes [160], G6PD genes [161], cpb genes [162, 163], gp63 genes [164], and hsp70 genes [165, 166]. For example, digestion of the ITS-1 PCR product with the Hae-III restriction enzyme differentiates most of the Leishmania species. The restriction fragment length polymorphism (RFLP) pattern is dependent on the restriction enzyme used, and thus the use of sequencing for confirmation is suggested. The random amplified polymorphic DNA technique (RAPD) is another molecular assay where amplification of DNA is performed using arbitrarily short primes without knowing the target sequences. Several studies have been performed using RAPD for investigation of genomic diversity [167,168,169,170], but its use in leishmaniasis is restricted due to the need for specific PCR standardization conditions and poor reproducibility [171]. Amplified fragment length polymorphism (AFLP) is a more advanced assay for investigation of variations in strains or closely related species [172]. It uses a restriction enzyme for genomic DNA digestion followed by selective PCR amplification of restriction fragments. Recently developed more sensitive PCR–fingerprinting techniques include multilocus sequence typing (MLST), which is based on the PCR amplification of multiple unlinked housekeeping genes followed by sequencing [68]. Moreover, a multilocus microsatellite typing (MLMT) approach has recently been developed by which East-African strains of L. donovani and Mediterranean strains of L. infantum could be resolved and assigned to genetically isolated populations [57, 74]. Srivastava et al. [70] explored the discriminatory power of different molecular assay and markers to detect genetic heterogeneity in clinical isolates of L. donovani from India [70]. Multilocus enzyme electrophoresis (MLEE) is another technique based on protein-based method which differentiates Leishmania parasites to species and subspecies levels using the electrophoretic mobility of enzymes [173]. This method has been known as the gold standard for characterization and identification of parasite strains. However, the requirement of mass cultivation of parasites, its low differentiation power in a homologous population, and the development of more sensitive molecular markers as alternative methods are the major drawbacks of MLEE [174]. Hernandez et al. [175] identified six new world Leishmania species through implementation of a High Resolution Melting (HRM) genotyping assay, which is another robust, highly sensitive, and reproducible genotyping technique.
2.4 Phylogenetic Analysis
The evolutionary pattern among species and the taxonomic status of Leishmania parasites are essential to understand the divergence among closely related species, design reliable diagnostic tools, and develop novel control methods. The malaria field is driving much of the relevant technology for this type of work. A major limiting factor to leishmaniasis is a critical lack of expertise throughout endemic areas. So far, many Leishmania strains have been typed by MLEE. On the other hand, introduction of numerous molecular typing methodologies with multicopy targets or multigene families have improved the analysis of phylogenetic, taxonomic, and genetic studies. These include DNA targets such as ITS [176], the single copy gene for the catalytic polypeptide from DNA polymerase α (polA) [177], cytochrome oxidase II (COII) gene [178, 179], cpB genes [180], 7SL RNA [181], and, most recently, the hsp70 subfamily sequence [165]. For example, Zhang et al. [73] investigated the phylogenetic relationship using ITS1 and kinetoplast COII gene sequencing and hypothesized that the phylogeny of Chinese Leishmania strains is associated with the geographical origin rather than the clinical form of the disease [73]. Fraga et al. [77] analyzed the phylogenetic study of 43 Leishmania strains from different geographic origins using the hsp70 sequence and found that monophylactic genus Leishmania consisted of three distinct subgenera: L. (Leishmania), L. (Viannia), and L. (Sauroleishmania) [77].
3 Technical Challenges and Future Prospects of Molecular-Based Assays
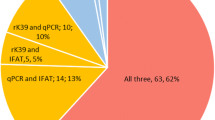
VL-affected patients living in endemic areas will not have access to quality care unless efforts are made to integrate existing innovative diagnostic technology into clinical management. For example, 3520 VL cases were reported in Sudan in 2014 and only 62% were diagnosed as confirmed VL. Molecular diagnostics are not only beneficial for patients, but if carried out through active case detection (such as sero surveys with the rk39 RDT) in the villages it will also reduce the parasite reservoir in highly endemic areas, given that humans are the only host reservoir for L. donovani on the Indian subcontinent. Though the sensitivity and diagnostic accuracy of molecular assays are reasonable to excellent in laboratory-based evaluations (reference laboratories), these methods are not currently able to be adapted to a PHC setting due to the expensive infrastructure and technical expertise required. The overall cost associated with a PCR assay is less than US$5 (230.0 Indian rupees) per sample [44]. Though this cost is two times greater than that for the rK39 RDT, it is currently not clear how such innovative techniques will replace rk39 RDT testing and how it can be meaningfully applied within the health system context of VL endemic areas. However, it is assumed that such rapid and highly sensitive molecular tools to assist clinicians working in the frontline PHC setting will help to better manage patients presenting with fever-related clinical syndromes. Strengthening early diagnosis and treatment capacities in PHC settings may provide long-term sustainability of the elimination effort through integrated case management as close as possible to the patient’s village. Importantly, the emergence and spread of drug resistance is a challenge for the VL control program. Therefore, monitoring drug efficacy and early reporting are essential as the drug arsenal is limited. Molecular detection tools would constitute a more rapid and high-throughput alternative to detect drug-resistant parasites, but requires a standardized way to use them and a structure to implement them in the sentinel sites.
4 Conclusion
There is no preventive or therapeutic vaccine for VL and the arsenal of anti-leishmanial drugs is limited; therefore, it is important to identify VL patients likely to relapse after drug treatment as well as new ways to recognize individuals who have had recent exposure to live parasites. Effective clinical management, chemotherapy, and control of transmission depend largely on early and unequivocal diagnosis. Molecular-based methods that can detect infection at a low level have recently become popular tools for diagnosis, and are relevant to the goal of VL elimination. To date, several molecular-based assays have been developed and evaluated, but PCR-based assays are found to be simple, rapid, and highly sensitive. The availability of such rapid tests that can be used to diagnose VL and as a marker of cure at peripheral health centers could have a great impact on the way VL is managed in endemic communities. These tests could be an alternative to the current rK39 dipstick test for accurate diagnosis and could be used to identify treatment failures and relapses.
References
Research priorities for Chagas disease, human African trypanosomiasis and leishmaniasis. World Health Organ Tech Rep Ser. 2012(975):v–xii, 1–100. http://apps.who.int/iris/bitstream/10665/77472/1/WHO_TRS_975_eng.pdf. Accessed 30 May 2018.
Tiwary P, Singh S, Kushwaha AK, Rowton E, Sacks D, Singh OP, et al. Establishing, expanding, and certifying a closed colony of Phlebotomus argentipes (Diptera: Psychodidae) for xenodiagnostic studies at the Kala Azar Medical Research Center, Muzaffarpur, Bihar, India. J Med Entomol. 2017;54(5):1129–39.
Guerin PJ, Olliaro P, Sundar S, Boelaert M, Croft SL, Desjeux P, et al. Visceral leishmaniasis: current status of control, diagnosis, and treatment, and a proposed research and development agenda. Lancet Infect Dis. 2002;2(8):494–501.
Singh OP, Hasker E, Boelaert M, Sundar S. Elimination of visceral leishmaniasis on the Indian subcontinent. Lancet Infect Dis. 2016;16(12):e304–e309.
Le Rutte EA, Coffeng LE, Bontje DM, Hasker EC, Postigo JA, Argaw D, et al. Feasibility of eliminating visceral leishmaniasis from the Indian subcontinent: explorations with a set of deterministic age-structured transmission models. Parasit Vect. 2016;9:24. https://doi.org/10.1186/s13071-016-1292-0.
Hollingsworth TD, Adams ER, Anderson RM, Atkins K, Bartsch S, Basáñez M-G, et al. Quantitative analyses and modelling to support achievement of the 2020 goals for nine neglected tropical diseases. Parasite Vect. 2015;8(1):630. http://www.parasitesandvectors.com/content/8/1/630. Accessed 30 May 2018.
Naghavi M, Wang H, Lozano R, Davis A, Liang X, Zhou M, et al. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–71. https://doi.org/10.1016/S0140-6736(14)61682-2.
Hirve S, Kroeger A, Matlashewski G, Mondal D, Banjara MR, Das P, et al. Towards elimination of visceral leishmaniasis in the Indian subcontinent: translating research to practice to public health. PLoS Negl Trop Dis. 2017;11(10):e0005889.
WHO/Regional Office for Europe. Manual on case management and surveillance of the leishmaniases in the WHO European Region. 2017. http://www.who.int/leishmaniasis/resources/978-92-89052-51-1/en/. Accessed 30 May 2018.
Reis LLD, Balieiro A, Fonseca FR, Goncalves MJF. Changes in the epidemiology of visceral leishmaniasis in Brazil from 2001 to 2014. Rev Soc Bras Med Trop. 2017;50(5):638–645.
Adam GK, Ali KM, Abdella YH, Omar SM, Ahmed MA, Abdalla TM, et al. Trend in cumulative cases and mortality rate among visceral leishmaniasis patients in Eastern Sudan: a 14-year registry, 2002–2015. Int J Infect Dis. 2016;51:81–4.
Stanley A, Engwerda C. Balancing immunity and pathology in visceral leishmaniasis. Immunol Cell Biol. 2007;85(2):138–147.
Pearson R, Sousa A. Clinical spectrum of leishmaniasis. Clin Infect Dis. 1996;22(1):1–11.
Dedet J, Pratlong F. Leishmaniasis. In: Cook GC, Zumla AI, editors. Manson’s tropical diseases. 22nd ed. London: Saunders; 2008. p. 1341–1365. https://doi.org/10.1016/j.trstmh.2009.09.003.
Control of the leishmaniases: report of a meeting of the WHO Expert Committee on the Control of Leishmaniases, Geneva, 22-26 March 2010. World Health Organisation Technical Report Series. 2011. http://apps.who.int/iris/handle/10665/44412. Accessed 30 May 2018.
Boelaert M, Meheus F, Sanchez A, Singh SP, Vanlerberghe V, Picado A, et al. The poorest of the poor: a poverty appraisal of households affected by visceral leishmaniasis in Bihar, India. Trop Med Int Health. 2009;14(6):639–44.
Boelaert M, Le Ray D, Der Van, Stuyft P. How better drugs could change kala-azar control. Lessons from a cost-effectiveness analysis. Trop Med Int Health. 2002;7(11):955–9.
Singh OP, Singh B, Chakravarty J, Sundar S. Current challenges in treatment options for visceral leishmaniasis in India: a public health perspective. Infect Dis Poverty. 2016;5:19. https://doi.org/10.1186/s40249-016-0112-2.
London Declaration on Neglected Tropical Diseases 2012. http://unitingtocombatntds.org/london-declaration-neglected-tropical-diseases/. Accessed 30 May 2018.
Sundar S, Mondal D, Rijal S, Bhattacharya S, Ghalib H, Kroeger A, et al. Implementation research to support the initiative on the elimination of kala azar from Bangladesh, India and Nepal—the challenges for diagnosis and treatment. Trop Med Int Health. 2008;13(1):2–5.
Sundar S, Rai M. Laboratory diagnosis of visceral leishmaniasis. Clin Diagn Lab Immunol. 2002;9(5):951–8.
Burki T. East African countries struggle with visceral leishmaniasis. Lancet. 2009;374(9687):371–2.
Singh OP, Sundar S. Developments in diagnosis of visceral leishmaniasis in the elimination era. J Parasitol Res. 2015;239469. https://doi.org/10.1155/2015/239469.
Chappuis F, Rijal S, Soto A, Menten J, Boelaert M. A meta-analysis of the diagnostic performance of the direct agglutination test and rK39 dipstick for visceral leishmaniasis. BMJ. 2006;333(7571):723.
Chappuis F, Sundar S, Hailu A, Ghalib H, Rijal S, Peeling RW, et al. Visceral leishmaniasis: what are the needs for diagnosis, treatment and control? Nat Rev Microbiol. 2007;5(11):873–82.
Maurya R, Mehrotra S, Prajapati VK, Nylen S, Sacks D, Sundar S. Evaluation of blood agar microtiter plates for culturing Leishmania parasites to titrate parasite burden in spleen and peripheral blood of patients with visceral leishmaniasis. J Clin Microbiol. 2010;48(5):1932–4.
Buxbaum L, Scott P. Interleukin 10- and Fcγ receptor-deficient mice resolve Leishmania mexicana Lesions. Infect Immun. 2005;73(4):2101–8.
Gidwani K, Picado A, Ostyn B, Singh SP, Kumar R, Khanal B, et al. Persistence of Leishmania donovani antibodies in past visceral leishmaniasis cases in India. Clin Vaccine Immunol. 2011;18(2):346–8.
Jacquet D, Boelaert M, Seaman J, Rijal S, Sundar S, Menten J, et al. Comparative evaluation of freeze-dried and liquid antigens in the direct agglutination test for serodiagnosis of visceral leishmaniasis (ITMA-DAT/VL). Trop Med Int Health. 2006;11(12):1777–84.
Sundar S, Reed SG, Singh VP, Kumar PC, Murray HW. Rapid accurate field diagnosis of Indian visceral leishmaniasis. Lancet. 1998;351(9102):563–5.
Cunningham J, Hasker E, Das P, El Safi S, Goto H, Mondal D, et al. A global comparative evaluation of commercial immunochromatographic rapid diagnostic tests for visceral leishmaniasis. Clin Infect Dis. 2012;55(10):1312–9.
Boelaert M, El-Safi S, Hailu A, Mukhtar M, Rijal S, Sundar S, et al. Diagnostic tests for kala-azar: a multi-centre study of the freeze-dried DAT, rK39 strip test and KAtex in East Africa and the Indian subcontinent. Trans R Soc Trop Med Hyg. 2008;102(1):32–40.
Srividya G, Kulshrestha A, Singh R, Salotra P. Diagnosis of visceral leishmaniasis: developments over the last decade. Parasitol Res. 2011;110(3):1065–78.
Das VN, Siddiqui NA, Verma RB, Topno RK, Singh D, Das S, et al. Asymptomatic infection of visceral leishmaniasis in hyperendemic areas of Vaishali district, Bihar, India: a challenge to kala-azar elimination programmes. Trans R Soc Trop Med Hyg. 2011;105(11):661–6.
Gidwani K, Kumar R, Rai M, Sundar S. Longitudinal seroepidemiologic study of visceral leishmaniasis in hyperendemic regions of Bihar. India. Am J Trop Med Hyg. 2009;80(3):345–6.
Rijal S, Boelaert M, Regmi S, Karki BM, Jacquet D, Singh R, et al. Evaluation of a urinary antigen-based latex agglutination test in the diagnosis of kala-azar in eastern Nepal. Trop Med Int Health. 2004;9(6):724–9.
Sundar S, Agrawal S, Pai K, Chance M, Hommel M. Detection of leishmanial antigen in the urine of patients with visceral leishmaniasis by a latex agglutination test. Am J Trop Med Hyg. 2005;73(2):269–71.
Diro E, Techane Y, Tefera T, Assefa Y, Kebede T, Genetu A, et al. Field evaluation of FD-DAT, rK39 dipstick and KATEX (urine latex agglutination) for diagnosis of visceral leishmaniasis in northwest Ethiopia. Trans R Soc Trop Med Hyg. 2007;101(9):908–14.
Akhoundi M, Downing T, Votýpka J, Kuhls K, Lukeš J, Cannet A, et al. Leishmania infections: molecular targets and diagnosis. Mol Aspects Med. 2017;57:1–29.
de Ruiter CM, van der Veer C, Leeflang MM, Deborggraeve S, Lucas C, Adams ER. Molecular tools for diagnosis of visceral leishmaniasis: systematic review and meta-analysis of diagnostic test accuracy. J Clin Microbiol. 2014;52(9):3147–55.
Saad AA, Ahmed NG, Osman OS, Al-Basheer AA, Hamad A, Deborggraeve S, et al. Diagnostic accuracy of the Leishmania OligoC-TesT and NASBA-Oligochromatography for diagnosis of leishmaniasis in Sudan. PLoS Negl Trop Dis. 2010;4(8):e776.
Mugasa CM, Deborggraeve S, Schoone GJ, Laurent T, Leeflang MM, Ekangu RA, et al. Accordance and concordance of PCR and NASBA followed by oligochromatography for the molecular diagnosis of Trypanosoma brucei and Leishmania. Trop Med Int Health. 2010;15(7):800–5.
Mugasa CM, Laurent T, Schoone GJ, Basiye FL, Saad AA, El Safi S, et al. Simplified molecular detection of Leishmania parasites in various clinical samples from patients with leishmaniasis. Parasit Vectors. 2010;3(1):13.
Srivastava P, Mehrotra S, Tiwary P, Chakravarty J, Sundar S. Diagnosis of Indian visceral leishmaniasis by nucleic acid detection using PCR. PLoS ONE. 2011;6(4):e19304.
Salotra P, Sreenivas G, Pogue GP, Lee N, Nakhasi HL, Ramesh V, et al. Development of a species-specific PCR assay for detection of Leishmania donovani in clinical samples from patients with kala-azar and post-kala-azar dermal leishmaniasis. J Clin Microbiol. 2001;39(3):849–54.
Maurya R, Singh RK, Kumar B, Salotra P, Rai M, Sundar S. Evaluation of PCR for diagnosis of Indian kala-azar and assessment of cure. J Clin Microbiol. 2005;43(7):3038–41.
Molina R, Lopez-Velez R, Gutierrez-Solar B, Jimenez I, Alvar J. Isolation of Leishmania infantum from the blood of a patient with AIDS using sandflies. Trans R Soc Trop Med Hyg. 1992;86(5):516.
Dweik A, Schonian G, Mosleh IM, Karanis P. Evaluation of PCR-RFLP (based on ITS-1 and HaeIII) for the detection of Leishmania species, using Greek canine isolates and Jordanian clinical material. Ann Trop Med Parasitol. 2007;101(5):399–407.
da Silva MA, Pedrosa Soares CR, Medeiros RA, Medeiros Z, de Melo FL. Optimization of single-tube nested PCR for the diagnosis of visceral leishmaniasis. Exp Parasitol. 2013;134(2):206–10.
Noyes HA, Reyburn H, Bailey JW, Smith D. A nested-PCR-based schizodeme method for identifying Leishmania kinetoplast minicircle classes directly from clinical samples and its application to the study of the epidemiology of Leishmania tropica in Pakistan. J Clin Microbiol. 1998;36(10):2877–81.
Harris E, Kropp G, Belli A, Rodriguez B, Agabian N. Single-step multiplex PCR assay for characterization of new world Leishmania complexes. J Clin Microbiol. 1998;36(7):1989–95.
Schonian G, Nasereddin A, Dinse N, Schweynoch C, Schallig HD, Presber W, et al. PCR diagnosis and characterization of Leishmania in local and imported clinical samples. Diagn Microbiol Infect Dis. 2003;47(1):349–58.
Ceccarelli M, Galluzzi L, Diotallevi A, Andreoni F, Fowler H, Petersen C, et al. The use of kDNA minicircle subclass relative abundance to differentiate between Leishmania (L.) infantum and Leishmania (L.) amazonensis. Parasit Vectors. 2017;10(1):239. https://doi.org/10.1186/s13071-017-2181-x.
Flegontov PN, Strelkova MV, Kolesnikov AA. The Leishmania major maxicircle divergent region is variable in different isolates and cell types. Mol Biochem Parasitol. 2006;146(2):173–9.
Mauricio IL, Gaunt MW, Stothard JR, Miles MA. Glycoprotein 63 (gp63) genes show gene conversion and reveal the evolution of Old World Leishmania. Int J Parasitol. 2007;37(5):565–76.
Lixia L, Jiping L, Hongtao J, Limin S, Bo L, Feng W, et al. Detection of Leishmania donovani infection using magnetic beads-based serum peptide profiling by MALDI-TOF MS in mice model. Parasitol Res. 2012;110(3):1287–90.
Schonian G, Kuhls K, Mauricio IL. Molecular approaches for a better understanding of the epidemiology and population genetics of Leishmania. Parasitology. 2010;138(4):405–25.
Montalvo AM, Fraga J, Monzote L, Montano I, De Doncker S, Dujardin JC, et al. Heat-shock protein 70 PCR-RFLP: a universal simple tool for Leishmania species discrimination in the new and old world. Parasitology. 2010;137(8):1159–68.
da Silva LA, de Sousa Cdos S, da Graca GC, Porrozzi R, Cupolillo E. Sequence analysis and PCR-RFLP profiling of the hsp70 gene as a valuable tool for identifying Leishmania species associated with human leishmaniasis in Brazil. Infect Genet Evol. 2010;10(1):77–83.
Cupolillo E, Grimaldi G Jr, Momen H. Discrimination of Leishmania isolates using a limited set of enzymatic loci. Ann Trop Med Parasitol. 1995;89(1):17–23.
Sudarshan M, Singh T, Singh AK, Chourasia A, Singh B, Wilson ME, et al. Quantitative PCR in epidemiology for early detection of visceral leishmaniasis cases in India. PLoS Negl Trop Dis. 2014;8(12):e3366. https://doi.org/10.1371/journal.pntd.0003366.
Sudarshan M, Sundar S. Parasite load estimation by qPCR differentiates between asymptomatic and symptomatic infection in Indian visceral leishmaniasis. Diagn Microbiol Infect Dis. 2014;80(1):40–2. https://doi.org/10.1016/j.diagmicrobio.2014.01.031.
Weirather JL, Jeronimo SM, Gautam S, Sundar S, Kang M, Kurtz MA, et al. Serial quantitative PCR assay for detection, species discrimination, and quantification of Leishmania spp. in human samples. J Clin Microbiol. 2011;49(11):3892–904.
van der Meide W, Guerra J, Schoone G, Farenhorst M, Coelho L, Faber W, et al. Comparison between quantitative nucleic acid sequence-based amplification, real-time reverse transcriptase PCR, and real-time PCR for quantification of Leishmania parasites. J Clin Microbiol. 2008;46(1):73–8.
Kobets T, Badalova J, Grekov I, Havelkova H, Svobodova M, Lipoldova M. Leishmania parasite detection and quantification using PCR-ELISA. Nat Protoc. 2010;5(6):1074–80.
Mary C, Faraut F, Lascombe L, Dumon H. Quantification of Leishmania infantum DNA by a real-time PCR assay with high sensitivity. J Clin Microbiol. 2004;42(11):5249–55.
Galluzzi L, Ceccarelli M, Diotallevi A, Menotta M, Magnani M. Real-time PCR applications for diagnosis of leishmaniasis. Parasit Vect. 2018;11(1):273. https://doi.org/10.1186/s13071-018-2859-8.
Boite MC, Mauricio IL, Miles MA, Cupolillo E. New insights on taxonomy, phylogeny and population genetics of Leishmania (Viannia) parasites based on multilocus sequence analysis. PLoS Negl Trop Dis. 2012;6(11):e1888.
Mauricio IL, Yeo M, Baghaei M, Doto D, Pratlong F, Zemanova E, et al. Towards multilocus sequence typing of the Leishmania donovani complex: resolving genotypes and haplotypes for five polymorphic metabolic enzymes (ASAT, GPI, NH1, NH2, PGD). Int J Parasitol. 2006;36(7):757–69.
Srivastava P, Singh T, Sundar S. Genetic heterogeneity in clinical isolates of Leishmania donovani from India. J Clin Microbiol. 2011;49(10):3687–90.
Downing T, Imamura H, Decuypere S, Clark TG, Coombs GH, Cotton JA, et al. Whole genome sequencing of multiple Leishmania donovani clinical isolates provides insights into population structure and mechanisms of drug resistance. Genome Res. 2011;21(12):2143–56.
Downing T, Stark O, Vanaerschot M, Imamura H, Sanders M, Decuypere S, et al. Genome-wide SNP and microsatellite variation illuminate population-level epidemiology in the Leishmania donovani species complex. Infect Genet Evol. 2012;12(1):149–59.
Zhang CY, Lu XJ, Du XQ, Jian J, Shu L, Ma Y. Phylogenetic and evolutionary analysis of Chinese Leishmania isolates based on multilocus sequence typing. PLoS One. 2013;8(4):e63124.
Kuhls K, Keilonat L, Ochsenreither S, Schaar M, Schweynoch C, Presber W, et al. Multilocus microsatellite typing (MLMT) reveals genetically isolated populations between and within the main endemic regions of visceral leishmaniasis. Microbes Infect. 2007;9(3):334–43.
Montalvo AM, Monzote L, Fraga J, Montano I, Muskus C, Marin M, et al. PCR-RFLP and RAPD for typing neotropical Leishmania. Biomedica. 2008;28(4):597–606.
Toledo A, Martin-Sanchez J, Pesson B, Sanchiz-Marin C, Morillas-Marquez F. Genetic variability within the species Leishmania infantum by RAPD. A lack of correlation with zymodeme structure. Mol Biochem Parasitol. 2002;119(2):257–64.
Fraga J, Montalvo AM, De Doncker S, Dujardin JC, Van der Auwera G. Phylogeny of Leishmania species based on the heat-shock protein 70 gene. Infect Genet Evol. 2010;10(2):238–45.
Alam MZ, Yasin G, Kato H, Sakurai T, Katakura K. PCR-based detection of Leishmania donovani DNA in a Stray dog from a visceral Leishmaniasis endemic focus in Bangladesh. J Vet Med Sci. 2012;75(1):75–8.
Blackwell JM. Leishmaniasis epidemiology: all down to the DNA. Parasitology. 1992;104(Suppl):S19–34.
Brustoloni YM, Lima RB, da Cunha RV, Dorval ME, Oshiro ET, de Oliveira AL, et al. Sensitivity and specificity of polymerase chain reaction in Giemsa-stained slides for diagnosis of visceral leishmaniasis in children. Mem Inst Oswaldo Cruz. 2007;102(4):497–500.
Schallig HD, Oskam L. Molecular biological applications in the diagnosis and control of leishmaniasis and parasite identification. Trop Med Int Health. 2002;7(8):641–51.
Reithinger R, Dujardin JC. Molecular diagnosis of leishmaniasis: current status and future applications. J Clin Microbiol. 2007;45(1):21–5.
Srivastava P, Dayama A, Mehrotra S, Sundar S. Diagnosis of visceral leishmaniasis. Trans R Soc Trop Med Hyg. 2010;105(1):1–6.
Mathis A, Deplazes P. PCR and in vitro cultivation for detection of Leishmania spp. in diagnostic samples from humans and dogs. J Clin Microbiol. 1995;33(5):1145–9.
Cortes S, Rolao N, Ramada J, Campino L. PCR as a rapid and sensitive tool in the diagnosis of human and canine leishmaniasis using Leishmania donovani s.l.-specific kinetoplastid primers. Trans R Soc Trop Med Hyg. 2004;98(1):12–7.
Katakura K, Kawazu S, Naya T, Nagakura K, Ito M, Aikawa M, et al. Diagnosis of kala-azar by nested PCR based on amplification of the Leishmania mini-exon gene. J Clin Microbiol. 1998;36(8):2173–7.
Prina E, Roux E, Mattei D, Milon G. Leishmania DNA is rapidly degraded following parasite death: an analysis by microscopy and real-time PCR. Microbes Infect. 2007;9(11):1307–15.
Costa CH, Stewart JM, Gomes RB, Garcez LM, Ramos PK, Bozza M, et al. Asymptomatic human carriers of Leishmania chagasi. Am J Trop Med Hyg. 2002;66(4):334–7.
Topno RK, Das VN, Ranjan A, Pandey K, Singh D, Kumar N, et al. Asymptomatic infection with visceral leishmaniasis in a disease-endemic area in Bihar, India. Am J Trop Med Hyg. 2010;83(3):502–6.
Bhattarai NR, Van der Auwera G, Khanal B, De Doncker S, Rijal S, Das ML, et al. PCR and direct agglutination as Leishmania infection markers among healthy Nepalese subjects living in areas endemic for Kala-Azar. Trop Med Int Health. 2009;14(4):404–11.
Srivastava P, Gidwani K, Picado A, Van der Auwera G, Tiwary P, Ostyn B, et al. Molecular and serological markers of Leishmania donovani infection in healthy individuals from endemic areas of Bihar, India. Trop Med Int Health. 2013;18(5):548–54.
Vallur AC, Duthie MS, Reinhart C, Tutterrow Y, Hamano S, Bhaskar KR, et al. Biomarkers for intracellular pathogens: establishing tools as vaccine and therapeutic endpoints for visceral leishmaniasis. Clin Microbiol Infect. 2013;20(6):O374–83. https://doi.org/10.1111/1469-0691.12421.
Biglino A, Bolla C, Concialdi E, Trisciuoglio A, Romano A, Ferroglio E. Asymptomatic Leishmania infantum infection in an area of northwestern Italy (Piedmont region) where such infections are traditionally nonendemic. J Clin Microbiol. 2009;48(1):131–6.
Abbasi I, Aramin S, Hailu A, Shiferaw W, Kassahun A, Belay S, et al. Evaluation of PCR procedures for detecting and quantifying Leishmania donovani DNA in large numbers of dried human blood samples from a visceral leishmaniasis focus in Northern Ethiopia. BMC Infect Dis. 2013;27(13):153.
Fisa R, Riera C, Lopez-Chejade P, Molina I, Gallego M, Falco V, et al. Leishmania infantum DNA detection in urine from patients with visceral leishmaniasis and after treatment control. Am J Trop Med Hyg. 2008;78(5):741–4.
Vaish M, Singh OP, Chakravarty J, Sundar S. rK39 antigen for the diagnosis of visceral leishmaniasis by using human saliva. Am J Trop Med Hyg. 2012;86(4):598–600.
Motazedian M, Fakhar M, Motazedian MH, Hatam G, Mikaeili F. A urine-based polymerase chain reaction method for the diagnosis of visceral leishmaniasis in immunocompetent patients. Diagn Microbiol Infect Dis. 2008;60(2):151–4.
Salam MA, Mondal D, Kabir M, Ekram AR, Haque R. PCR for diagnosis and assessment of cure in kala-azar patients in Bangladesh. Acta Trop. 2010;113(1):52–5.
Jorquera A, Gonzalez R, Marchan-Marcano E, Oviedo M, Matos M. Multiplex-PCR for detection of natural Leishmania infection in Lutzomyia spp. captured in an endemic region for cutaneous leishmaniasis in state of Sucre, Venezuela. Mem Inst Oswaldo Cruz. 2005;100(1):45–8.
Deborggraeve S, Laurent T, Espinosa D, Van der Auwera G, Mbuchi M, Wasunna M, et al. A simplified and standardized polymerase chain reaction format for the diagnosis of leishmaniasis. J Infect Dis. 2008;198(10):1565–72.
De Doncker S, Hutse V, Abdellati S, Rijal S, Singh Karki BM, Decuypere S, et al. A new PCR-ELISA for diagnosis of visceral leishmaniasis in blood of HIV-negative subjects. Trans R Soc Trop Med Hyg. 2005;99(1):25–31.
Verma S, Avishek K, Sharma V, Negi NS, Ramesh V, Salotra P. Application of loop-mediated isothermal amplification assay for the sensitive and rapid diagnosis of visceral leishmaniasis and post-kala-azar dermal leishmaniasis. Diagn Microbiol Infect Dis. 2013;75(4):390–5.
Khan MG, Bhaskar KR, Salam MA, Akther T, Pluschke G, Mondal D. Diagnostic accuracy of loop-mediated isothermal amplification (LAMP) for detection of Leishmania DNA in buffy coat from visceral leishmaniasis patients. Parasit Vectors. 2012;5:280. https://doi.org/10.1186/1756-3305-5-280.
Castellanos-Gonzalez A, Saldarriaga OA, Tartaglino L, Gacek R, Temple E, Sparks H, et al. A novel molecular test to diagnose canine visceral leishmaniasis at the point of care. Am J Trop Med Hyg. 2015;93(5):970–5.
Mondal D, Ghosh P, Khan MA, Hossain F, Bohlken-Fascher S, Matlashewski G, et al. Mobile suitcase laboratory for rapid detection of Leishmania donovani using recombinase polymerase amplification assay. Parasit Vectors. 2016;9(1):281.
Srivastava P, Gidwani K, Picado A, Van der Auwera G, Tiwary P, Ostyn B, et al. Molecular and serological markers of Leishmania donovani infection in healthy individuals from endemic areas of Bihar. India. Trop Med Int Health. 2013;18(5):548–54.
Vaish M, Mehrotra S, Chakravarty J, Sundar S. Noninvasive molecular diagnosis of human visceral leishmaniasis. J Clin Microbiol. 2011;49(5):2003–5.
Ferreira Sde A, Almeida GG, Silva Sde O, Vogas GP, Fujiwara RT, de Andrade AS, et al. Nasal, oral and ear swabs for canine visceral leishmaniasis diagnosis: new practical approaches for detection of Leishmania infantum DNA. PLoS Negl Trop Dis. 2013;7(4):e2150.
de Ruiter CM, van der Veer C, Leeflang MMG, Deborggraeve S, Lucas C, Adams ER. Molecular tools for diagnosis of visceral leishmaniasis: systematic review and meta-analysis of diagnostic test accuracy. J Clin Microbiol. 2014; 52(9):3147–55.
Adhya S, Chatterjee M, Hassan MQ, Mukherjee S, Sen S. Detection of Leishmania in the blood of early kala-azar patients with the aid of the polymerase chain reaction. Trans R Soc Trop Med Hyg. 1995;89(6):622–4.
Disch J, Maciel FC, de Oliveira MC, Orsini M, Rabello A. Detection of circulating Leishmania chagasi DNA for the non-invasive diagnosis of human infection. Trans R Soc Trop Med Hyg. 2003;97(4):391–5.
Wu Z, Bao Y, Ding Y, Yu M, Lu L, Zhang Y. An experimental study on application of PCR in detection of kala-azar. Southeast Asian J Trop Med Public Health. 1997;28(1):169–72.
Osman OF, Oskam L, Zijlstra EE, Kroon NC, Schoone GJ, Khalil ET, et al. Evaluation of PCR for diagnosis of visceral leishmaniasis. J Clin Microbiol. 1997;35(10):2454–7.
Alam MZ, Shamsuzzaman AK, Kuhls K, Schonian G. PCR diagnosis of visceral leishmaniasis in an endemic region, Mymensingh district. Bangladesh. Trop Med Int Health. 2009;14(5):499–503.
Sudarshan M, Singh T, Chakravarty J, Sundar S. A correlative study of splenic parasite score and peripheral blood parasite load estimation by quantitative PCR in visceral leishmaniasis. J Clin Microbiol. 2015;53(12):3905–7.
de Paiva-Cavalcanti M, de Morais RC, Pessoa-E-Silva R, Trajano-Silva LA, Gonçalves-de-Albuquerque SC, Tavares Dde H, et al. Leishmaniases diagnosis: an update on the use of immunological and molecular tools. Cell Biosci. 2015;5:31. https://doi.org/10.1186/s13578-015-0021-2.
Galai Y, Chabchoub N, Ben-Abid M, Ben-Abda I, Ben-Alaya-Bouafif N, Amri F, et al. Diagnosis of mediterranean visceral leishmaniasis by detection of leishmania antibodies and leishmania DNA in oral fluid samples collected using an Oracol device. J Clin Microbiol. 2011;49(9):3150–3.
Hu XS, Yang WT, Lu HG, Yan HP, Cheng JP, Ma Y, et al. Sequencing a specific kinetoplast DNA fragment of Leishmania donovani for polymerase chain reaction amplification in diagnosis of leishmaniasis in bone marrow and blood samples. J Parasitol. 2000;86(4):822–6.
Adams ER, Schoone GJ, Ageed AF, Safi SE, Schallig HD. Development of a reverse transcriptase loop-mediated isothermal amplification (LAMP) assay for the sensitive detection of Leishmania parasites in clinical samples. Am J Trop Med Hyg. 2010;82(4):591–6.
Takagi H, Itoh M, Islam MZ, Razzaque A, Ekram AR, Hashighuchi Y, et al. Sensitive, specific, and rapid detection of Leishmania donovani DNA by loop-mediated isothermal amplification. Am J Trop Med Hyg. 2009;81(4):578–82.
Adams ER, Schoone G, Versteeg I, Gomez MA, Diro E, Mori Y, et al. Development and evaluation of a novel LAMP assay for the diagnosis of cutaneous and visceral leishmaniasis. J Clin Microbiol. Epub. 2018. https://doi.org/10.1128/JCM.00386-18.
Hendrickx S, Guerin PJ, Caljon G, Croft SL, Maes L. Evaluating drug resistance in visceral leishmaniasis: the challenges. Parasitology. 2018;145(4):453–63.
Singh OP, Singh B, Chakravarty J, Sundar S. Current challenges in treatment options for visceral leishmaniasis in India: a public health perspective. Infect Dis Poverty. 2016;8(5):19. https://doi.org/10.1186/s40249-016-0112-2.
Freitas-Junior LH, Chatelain E, Kim HA, Siqueira-Neto JL. Visceral leishmaniasis treatment: what do we have, what do we need and how to deliver it? Int J Parasitol Drugs Drug Resist. 2012;2:11–9.
Srivastava P, Prajapati VK, Rai M, Sundar S. Unusual case of resistance to amphotericin B in visceral leishmaniasis in a region in India where leishmaniasis is not endemic. J Clin Microbiol. 2011;49(8):3088–91.
Gomes CM, Cesetti MV, de Paula NA, Vernal S, Gupta G, Sampaio RN, et al. Field validation of SYBR green- and TaqMan-based real-time PCR using biopsy and swab samples to diagnose american tegumentary leishmaniasis in an area where Leishmania (Viannia) braziliensis is endemic. J Clin Microbiol. 2017;55(2):526–34. https://doi.org/10.1128/JCM.01954-16.
Manna L, Reale S, Viola E, Vitale F, Foglia Manzillo V, Pavone LM, et al. Leishmania DNA load and cytokine expression levels in asymptomatic naturally infected dogs. Vet Parasitol. 2006;142(3–4):271–80.
Sudarshan M, Weirather JL, Wilson ME, Sundar S. Study of parasite kinetics with antileishmanial drugs using real-time quantitative PCR in Indian visceral leishmaniasis. J Antimicrob Chemother. 2011;66(8):1751–5.
Hossain F, Ghosh P, Khan MAA, Duthie MS, Vallur AC, Picone A, et al. Real-time PCR in detection and quantitation of Leishmania donovani for the diagnosis of Visceral Leishmaniasis patients and the monitoring of their response to treatment. PLoS One. 2017;12(9):e0185606. https://doi.org/10.1371/journal.pone.0185606.
de Paiva Cavalcanti M, Felinto de Brito ME, de Souza WV, de Miranda Gomes Y, Abath FG. The development of a real-time PCR assay for the quantification of Leishmania infantum DNA in canine blood. Vet J. 2009;182(2):356–8.
Dantas-Torres F, da Silva Sales KG, Gomes da Silva L, Otranto D, Figueredo LA. Leishmania-FAST15: a rapid, sensitive and low-cost real-time PCR assay for the detection of Leishmania infantum and Leishmania braziliensis kinetoplast DNA in canine blood samples. Mol Cell Probes. 2017;31:65–9. https://doi.org/10.1016/j.mcp.2016.08.006.
Molina I, Fisa R, Riera C, Falco V, Elizalde A, Salvador F, et al. Ultrasensitive real-time PCR for the clinical management of visceral leishmaniasis in HIV-infected patients. Am J Trop Med Hyg. 2013;89(1):105–10. https://doi.org/10.4269/ajtmh.12-0527.
Silva RC, Richini-Pereira VB, Kikuti M, Marson PM, Langoni H. Detection of Leishmania (L.) infantum in stray dogs by molecular techniques with sensitive species-specific primers. Vet Q. 2017;37(1):23–30.
Ribeiro-Romão RP, Saavedra AF, Da-Cruz AM, Pinto EF, Moreira OC. Development of real-time PCR assays for evaluation of immune response and parasite load in golden hamster (Mesocricetus auratus) infected by Leishmania (Viannia) braziliensis. Parasit Vectors. 2016;9(1):361. https://doi.org/10.1186/s13071-016-1647-6).
Suárez M, Valencia BM, Jara M, Alba M, Boggild AK, Dujardin JC, et al. Quantification of Leishmania (Viannia) kinetoplast DNA in ulcers of cutaneous leishmaniasis reveals inter-site and inter-sampling variability in parasite load. PLoS Negl Trop Dis. 2015;9(7):e0003936. https://doi.org/10.1371/journal.pntd.0003936.
Jara M, Adaui V, Valencia BM, Martinez D, Alba M, Castrillon C, et al. Real-time PCR assay for detection and quantification of Leishmania (viannia) organisms in skin and mucosal lesions: exploratory study of parasite load and clinical parameters. J Clin Microbiol. 2013;51(6):1826–33.
Talmi-Frank D, Nasereddin A, Schnur LF, Schonian G, Toz SO, Jaffe CL, et al. Detection and identification of old world Leishmania by high resolution melt analysis. PLoS Negl Trop Dis. 2010;4(1):e581.
de Almeida ME, Koru O, Steurer F, Herwaldt BL, da Silva AJ. Detection and differentiation of Leishmania spp. in clinical specimens by use of a SYBR green-based real-time PCR assay. J Clin Microbiol. 2016;55(1):281-290. https://doi.org/10.1128/JCM.01764-16.
Bossolasco S, Gaiera G, Olchini D, Gulletta M, Martello L, Bestetti A, et al. Real-time PCR assay for clinical management of human immunodeficiency virus-infected patients with visceral leishmaniasis. J Clin Microbiol. 2003;41(11):5080–4.
Schulz A, Mellenthin K, Schonian G, Fleischer B, Drosten C. Detection, differentiation, and quantitation of pathogenic leishmania organisms by a fluorescence resonance energy transfer-based real-time PCR assay. J Clin Microbiol. 2003;41(4):1529–35.
Miro G, Oliva G, Cruz I, Canavate C, Mortarino M, Vischer C, et al. Multicentric, controlled clinical study to evaluate effectiveness and safety of miltefosine and allopurinol for canine leishmaniosis. Vet Dermatol. 2009;20(5–6):397–404.
Wortmann G, Hochberg L, Houng HH, Sweeney C, Zapor M, Aronson N, et al. Rapid identification of Leishmania complexes by a real-time PCR assay. Am J Trop Med Hyg. 2005;73(6):999–1004.
León CM, Muñoz M, Hernández C, Ayala MS, Flórez C, Teherán A, et al. Analytical performance of four polymerase chain reaction (PCR) and real time PCR (qPCR) assays for the detection of six Leishmania species DNA in Colombia. Front Microbiol. 2017;8:1907. https://doi.org/10.3389/fmicb.2017.01907.
Zampieri RA, Laranjeira-Silva MF, Muxel SM, Stocco de Lima AC, Shaw JJ, Floeter-Winter LM. High resolution melting analysis targeting hsp70 as a fast and efficient method for the discrimination of Leishmania species. PLoS Negl Trop Dis. 2016;10(2):e0004485. https://doi.org/10.1371/journal.pntd.0004485.
Verma S, Kumar R, Katara GK, Singh LC, Negi NS, Ramesh V, et al. Quantification of parasite load in clinical samples of leishmaniasis patients: IL-10 level correlates with parasite load in visceral leishmaniasis. PLoS One. 2010;5(4):e10107.
Leon CM, Munoz M, Hernandez C, Ayala MS, Florez C, Teheran A, et al. Analytical performance of four polymerase chain reaction (PCR) and real time PCR (qPCR) assays for the detection of six Leishmania species DNA in Colombia. Front Microbiol. 2017;8:1907.
Medeiros FA, Gomes LI, Oliveira E, de Souza CS, Mourao MV, Cota GF, et al. Development and validation of a PCR-ELISA for the diagnosis of symptomatic and asymptomatic infection by Leishmania (Leishmania) infantum. J Trop Med. 2017;2017:7364854.
Sue MJ, Yeap SK, Omar AR, Tan SW. Application of PCR-ELISA in molecular diagnosis. Biomed Res Int. 2014;2014:653014. https://doi.org/10.1155/2014/653014.
Aara N, Khandelwal K, Bumb RA, Mehta RD, Ghiya BC, Jakhar R, et al. Clinco-epidemiologic study of cutaneous leishmaniasis in Bikaner, Rajasthan, India. Am J Trop Med Hyg. 2013;89(1):111–5. https://doi.org/10.4269/ajtmh.12-0558.
Khandelwal K, Bumb RA, Mehta RD, Kaushal H, Lezama-Davila C, Salotra P, et al. A patient presenting with diffuse cutaneous leishmaniasis (DCL) as a first indicator of HIV infection in India. Am J Trop Med Hyg. 2011;85(1):64–5.
Sharma NL, Mahajan VK, Kanga A, Sood A, Katoch VM, Mauricio I, et al. Localized cutaneous leishmaniasis due to Leishmania donovani and Leishmania tropica: preliminary findings of the study of 161 new cases from a new endemic focus in himachal pradesh. India. Am J Trop Med Hyg. 2005;72(6):819–24.
Zijlstra EE, Musa AM, Khalil EA. el-Hassan IM, el-Hassan AM. Post-kala-azar dermal leishmaniasis. Lancet Infect Dis. 2003;3(2):87–98.
Rahman KM, Islam S, Rahman MW, Kenah E, Ghalib CM, Zahid MM, et al. Increasing incidence of post-kala-azar dermal leishmaniasis in a population-based study in Bangladesh. Clin Infect Dis. 2009;50(1):73–6.
Cupolillo E, Grimaldi Junior G, Momen H, Beverley SM. Intergenic region typing (IRT): a rapid molecular approach to the characterization and evolution of Leishmania. Mol Biochem Parasitol. 1995;73(1–2):145–55.
Mauricio IL, Stothard JR, Miles MA. Leishmania donovani complex: genotyping with the ribosomal internal transcribed spacer and the mini-exon. Parasitology. 2004;128(Pt 3):263–7.
Chargui N, Haouas N, Jaouadi K, Gorcii M, Pratlong F, Dedet JP, et al. Usefulness of a PCR-based method in the detection and species identification of Leishmania from clinical samples. Pathol Biol (Paris). 2012;60(6):e75–9.
Piarroux R, Azaiez R, Lossi AM, Reynier P, Muscatelli F, Gambarelli F, et al. Isolation and characterization of a repetitive DNA sequence from Leishmania infantum: development of a visceral leishmaniasis polymerase chain reaction. Am J Trop Med Hyg. 1993;49(3):364–9.
Luyo-Acero GE, Uezato H, Oshiro M, Takei K, Kariya K, Katakura K, et al. Sequence variation of the cytochrome b gene of various human infecting members of the genus Leishmania and their phylogeny. Parasitology. 2004;128(Pt 5):483–91.
Yang BB, Chen DL, Chen JP, Liao L, Hu XS, Xu JN. Analysis of kinetoplast cytochrome b gene of 16 Leishmania isolates from different foci of China: different species of Leishmania in China and their phylogenetic inference. Parasit Vectors. 2013;6:32.
Marfurt J, Nasereddin A, Niederwieser I, Jaffe CL, Beck HP, Felger I. Identification and differentiation of Leishmania species in clinical samples by PCR amplification of the miniexon sequence and subsequent restriction fragment length polymorphism analysis. J Clin Microbiol. 2003;41(7):3147–53.
Castilho TM, Shaw JJ, Floeter-Winter LM. New PCR assay using glucose-6-phosphate dehydrogenase for identification of Leishmania species. J Clin Microbiol. 2003;41(2):540–6.
Hide M, Banuls AL. Polymorphisms of cpb multicopy genes in the Leishmania (Leishmania) donovani complex. Trans R Soc Trop Med Hyg. 2008;102(2):105–6.
Hide M, Banuls AL. Species-specific PCR assay for L. infantum/L. donovani discrimination. Acta Trop. 2006;100(3):241–5.
Victoir K, Banuls AL, Arevalo J, Llanos-Cuentas A, Hamers R, Noel S, et al. The gp63 gene locus, a target for genetic characterization of Leishmania belonging to subgenus Viannia. Parasitology. 1998;117(Pt 1):1–13.
Fraga J, Montalvo AM, Van der Auwera G, Maes I, Dujardin JC, Requena JM. Evolution and species discrimination according to the Leishmania heat-shock protein 20 gene. Infect Genet Evol. 2013;28(18C):229–37.
Garcia L, Kindt A, Bermudez H, Llanos-Cuentas A, De Doncker S, Arevalo J, et al. Culture-independent species typing of neotropical Leishmania for clinical validation of a PCR-based assay targeting heat shock protein 70 genes. J Clin Microbiol. 2004;42(5):2294–7.
Hamad SH, Khalil EA, Musa AM, Ibrahim ME, Younis BM, Elfaki ME, et al. Leishmania donovani: genetic diversity of isolates from Sudan characterized by PCR-based RAPD. Exp Parasitol. 2010;125(4):389–93.
Mauricio IL, Howard MK, Stothard JR, Miles MA. Genomic diversity in the Leishmania donovani complex. Parasitology. 1999;119(Pt 3):237–46.
Martinez E, Alonso V, Quispe A, Thomas MC, Alonso R, Pinero JE, et al. RAPD method useful for distinguishing Leishmania species: design of specific primers for L. braziliensis. Parasitology. 2003;127(Pt 6):513–7.
Khanra S, Bandopadhyay SK, Chakraborty P, Datta S, Mondal D, Chatterjee M, et al. Characterization of the recent clinical isolates of Indian Kala-azar patients by RAPD-PCR method. J Parasit Dis. 2012;35(2):116–22.
Eisenberger CL, Jaffe CL. Leishmania: identification of Old World species using a permissively primed intergenic polymorphic-polymerase chain reaction. Exp Parasitol. 1999;91(1):70–7.
Kumar A, Boggula VR, Misra P, Sundar S, Shasany AK, Dube A. Amplified fragment length polymorphism (AFLP) analysis is useful for distinguishing Leishmania species of visceral and cutaneous forms. Acta Trop. 2010;113(2):202–6.
Rioux JA, Lanotte G, Serres E, Pratlong F, Bastien P, Perieres J. Taxonomy of Leishmania. Use of isoenzymes. Suggestions for a new classification. Ann Parasitol Hum Comp. 1990;65(3):111–25.
Banuls AL, Hide M, Prugnolle F. Leishmania and the leishmaniases: a parasite genetic update and advances in taxonomy, epidemiology and pathogenicity in humans. Adv Parasitol. 2007;64:1–109.
Hernandez C, Alvarez C, Gonzalez C, Ayala MS, Leon CM, Ramirez JD. Identification of six New World Leishmania species through the implementation of a high-resolution melting (HRM) genotyping assay. Parasit Vectors. 2014;14(7):501.
Berzunza-Cruz M, Cabrera N, Crippa-Rossi M, Sosa Cabrera T, Perez-Montfort R, Becker I. Polymorphism analysis of the internal transcribed spacer and small subunit of ribosomal RNA genes of Leishmania mexicana. Parasitol Res. 2002;88(10):918–25.
Croan DG, Morrison DA, Ellis JT. Evolution of the genus Leishmania revealed by comparison of DNA and RNA polymerase gene sequences. Mol Biochem Parasitol. 1997;89(2):149–59.
Ibrahim ME, Barker DC. The origin and evolution of the Leishmania donovani complex as inferred from a mitochondrial cytochrome oxidase II gene sequence. Infect Genet Evol. 2001;1(1):61–8.
Asato Y, Oshiro M, Myint CK, Yamamoto Y, Kato H, Marco JD, et al. Phylogenic analysis of the genus Leishmania by cytochrome b gene sequencing. Exp Parasitol. 2009;121(4):352–61.
Hide M, Bras-Goncalves R, Banuls AL. Specific cpb copies within the Leishmania donovani complex: evolutionary interpretations and potential clinical implications in humans. Parasitology. 2007;134(Pt 3):379–89.
Zelazny AM, Fedorko DP, Li L, Neva FA, Fischer SH. Evaluation of 7SL RNA gene sequences for the identification of Leishmania spp. Am J Trop Med Hyg. 2005;72(4):415–20.
Pita-Pereira D, Lins R, Oliveira MP, Lima RB, Pereira BA, Moreira OC, Brazil RP, Britto C. SYBR Green-based Real-Time PCR targeting kinetoplast DNA can be used to discriminate between the main etiologic agents of Brazilian cutaneous and visceral leishmaniases. Parasit Vect. 2012;5:15. https://doi.org/10.1186/1756-3305-5-15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SS and OPS declare no conflicts of interest.
Funding
This work was supported by the Bill & Melinda Gates Foundation (BMGF), USA (Grant no. OPP 1117011), Extramural Program of the National Institute of Allergy and Infectious Disease (NIAID), and National Institute of Health (TMRC [Tropical Medicine Research Centers] Grant no. U19AI074321). The funders had no role in the design, decision to publish, or preparation of this report.
Rights and permissions
About this article
Cite this article
Sundar, S., Singh, O.P. Molecular Diagnosis of Visceral Leishmaniasis. Mol Diagn Ther 22, 443–457 (2018). https://doi.org/10.1007/s40291-018-0343-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-018-0343-y