Abstract
Purpose
We designed a network meta-analysis that investigated relatively different interventions that included the effects of metformin, oral contraceptives, and lifestyle modification on the metabolic parameters of patients with polycystic ovary syndrome. In addition, we searched for eligible interventions that improved the metabolism of glucose and lipids.
Methods
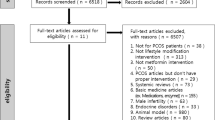
We searched the PubMed, EMBASE, and Cochrane Central databases from inception to May 2018. Publication types that were categorized as randomized controlled trials met our inclusion criteria. The main outcome included the homeostasis model assessment of insulin resistance, total cholesterol, low-density lipoprotein cholesterol, and total triglycerides. We performed both a pairwise meta-analysis and a network meta-analysis to evaluate the mean difference value and 95% credibility intervals, and we calculated the surface cumulative rank curve.
Results
There were a total of 12 kinds of interventions: metformin, 2 mg cyproterone acetate plus 0.05 mg ethinylestradiol (EE/CA), 0.15 mg desogestrel plus 0.03 mg ethinylestradiol (EE/DSG), and 3 mg drospirenone plus 0.03 mg ethinylestradiol (EE/DRSP), lifestyle, exercise, diet, metformin + lifestyle, metformin + diet, EE/CA + lifestyle, metformin + EE/CA, and EE/DRSP + lifestyle from the 20 eligible RCTs that were included in this study. Our meta-analysis results showed that metformin + lifestyle (MD = −2.04, 95% CrI = −3.64 to −0.41), EE/CA + lifestyle (MD = −2.23, 95% CrI = −4.11 to −0.35), and EE/DRSP + lifestyle (MD = −2.59, 95% CrI = −4.66 to −0.50) resulted in lower in the levels of total cholesterol. Women treated with metformin + lifestyle (MD = −1.82, 95% CrI = −2.88 to −0.79), EE/CA + lifestyle (MD = −2.25, 95% CrI = −3.58 to −1.08), or EE/DRSP + lifestyle (MD = −2.29, 95% CrI = −3.69 to −1.07) exhibited significantly lower low-density lipoprotein cholesterol when compared with the placebo group. There was no significant difference between any of the interventions compared with a placebo in the levels of homeostasis model assessment of insulin resistance and total triglycerides. The surface cumulative rank curve revealed that metformin + lifestyle might be the best intervention with respect to the improvement of the homeostasis model of assessment insulin resistance and EE/DRSP + lifestyle appeared to be the best intervention for the reduction of total cholesterol and low-density lipoprotein cholesterol. Moreover, the metformin + diet intervention was more effective in reducing the level of total triglycerides.
Conclusions
For overweight polycystic ovary syndrome patients, our evidence revealed that EE/CA and EE/SRSP combined with metformin or lifestyle changes can reduce the adverse effects on glucose and lipid metabolism of the use of oral contraceptive agents alone. Conventional PCOS treatments, such as metformin, EE/CA, and EE/DRSP, combined with lifestyle control can be particularly effective in improving the homeostasis model assessment of insulin resistance and lipid metabolism.




Similar content being viewed by others
References
G. Bozdag, S. Mumusoglu, D. Zengin, E. Karabulut, B.O. Yildiz, The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum. Reprod. 31, 2841–2855 (2016)
S. Mahalingaiah, E. Diamanti-Kandarakis, Targets to treat metabolic syndrome in polycystic ovary syndrome. Expert Opin. Ther. Targets 19, 1561–1574 (2015)
S.F. De Medeiros, Risks, benefits size and clinical implications of combined oral contraceptive use in women with polycystic ovary syndrome. Reprod. Biol. Endocrinol. 15, 93 (2017)
N. Naderpoor, S. Shorakae, B. de Courten, M.L. Misso, L.J. Moran, H.J. Teede, Metformin and lifestyle modification in polycystic ovary syndrome: systematic review and meta-analysis. Hum. Reprod. Update 21, 560–574 (2015)
R. Davidson, T. Motan, C. Korownyk, Clomiphene for anovulatory infertility. Can. Fam. Physician 62, 492 (2016)
S. Mitra, P.K. Nayak, S. Agrawal, Laparoscopic ovarian drilling: an alternative but not the ultimate in the management of polycystic ovary syndrome. J. Nat. Sci. Biol. Med. 6, 40–48 (2015)
A.P. Delitala, G. Capobianco, G. Delitala, P.L. Cherchi, S. Dessole, Polycystic ovary syndrome, adipose tissue and metabolic syndrome. Arch. Gynecol. Obstet. 296, 405–419 (2017)
R.S. Legro, Ovulation induction in polycystic ovary syndrome: current options. Best Pract. Res. Clin. Obstet. Gynaecol. 37, 152–159 (2016)
H. Abu Hashim, A. Wafa, M. El Rakhawy, Combined metformin and clomiphene citrate versus highly purified FSH for ovulation induction in clomiphene-resistant PCOS women: a randomised controlled trial. Gynecol. Endocrinol. 27, 190–196 (2011)
H. Nasri, M. Rafieian-Kopaei, Metformin: current knowledge. J. Res. Med. Sci. 19, 658–664 (2014)
K.G. Piparva, J.G. Buch, Deep vein thrombosis in a woman taking oral combined contraceptive pills. J. Pharmacol. Pharmacother. 2, 185–186 (2011)
R. Sitruk-Ware, A. Nath, Metabolic effects of contraceptive steroids. Rev. Endocr. Metab. Disord. 12, 63–75 (2011)
M. Api, H. Görgen, A. Cetin, Laparoscopic ovarian drilling in polycystic ovary syndrome. Eur. J. Obstet. Gynecol. Reprod. Biol. 119, 76–81 (2005)
J.P. Domecq, G. Prutsky, R.J. Mullan, A. Hazem, V. Sundaresh, Lifestyle modification programs in polycystic ovary syndrome: systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 98, 4655–4663 (2013)
H.F. Escobar Morreale, Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat. Rev. Endocrinol. 14, 270–284 (2018)
J.J. Deeks, J.P. Higgins, D.G. Altman, Assessing risk of bias in included studies. in Cochrane Handbook or Systematic Reviews of Interventions Version 5.1.0, ed. by J.P. Higgins, S. Green (The Cochrane Collaboration, UK, 2011), Chapter 8
B. Bruner, K. Chad, D. Chizen, Effects of exercise and nutritional counseling in women with polycystic ovary syndrome. Appl. Physiol. Nutr. Metab. 31, 384–391 (2006)
S.P. Hozo, B. Djulbegovic, I. Hozo, Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 5, 13 (2005)
A.E. Georgia Salantia, Adesb, P.A. John, Ioannidis: graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J. Clin. Epidemiol. 64, 163–171 (2011)
J. Lord, R. Thomas, B. Fox, U. Acharya, T. Wilkin, The effect of metformin on fat distribution and the metabolic syndrome in women with polycystic ovary syndrome—a randomised, double-blind, placebo-controlled trial. BJOG 113, 817–824 (2006)
A. Gambineri, L. Patton, A. Vaccina, M. Cacciari, A.M. Morselli-Labate, C. Cavazza, U. Pagotto, R. Pasquali, Treatment with flutamide, metformin, and their combination added to a hypocaloric diet in overweight-obese women with polycystic ovary syndrome: a randomized, 12-month, placebo-controlled study. J. Clin. Endocrinol. Metab. 91, 3970–3980 (2006)
T. Tang, J. Glanville, C.J. Hayden, D. White, J.H. Barth, A.H. Balen, Combined lifestyle modification and metformin in obese patients with polycystic ovary syndrome. A randomized, placebo-controlled, double-blind multicentre study. Hum. Reprod. 21, 80–89 (2006)
C. Vigorito, F. Giallauria, S. Palomba, T. Cascella, F. Manguso, R. Lucci, A. De Lorenzo, D. Tafuri, G. Lombardi, A. Colao, F. Orio, Beneficial effects of a three-month structured exercise training program on cardiopulmonary functional capacity in young women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 92, 1374–1384 (2007)
LK Ma, L.N. Jin, Q. Yu, L. Xu, Effect of lifestyle adjustment, metformin and rosiglitazone in polycystic ovary syndrome. Zhonghua. Fu. Chan. Ke. Za. Zhi. 42, 294–297 (2007)
S.K. Hutchison, C. Harrison, N. Stepto, C. Meyer, Teede Hj, Retinol-binding protein 4 and insulin resistance in polycystic ovary syndrome. Diabetes Care 31, 1427–1432 (2008)
R.L. Thomson, J.D. Buckley, M. Noakes, P.M. Clifton, R.J. Norman, G.D. Brinkworth, The effect of a hypocaloric diet with and without exercise training on body composition, cardiometabolic risk profile, and reproductive function in overweight and obese women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 93, 3373–3380 (2008)
L. Kebapcilar, A. Yuksel, G. Bozkaya et al. Effects of an EE/CA compared with EE/CA-metformin on serum ADMA levels in women with polycystic ovary syndrome. Cent. Eur. J. Med. 4, 423–427 (2009). https://doi.org/10.2478/s11536-009-0074-x
L. Kebapcilar, C.E. Taner, A.G. Kebapcilar, A. Alacacioglu, I. Sari, Comparison of four different treatment regimens on coagulation parameters, hormonal and metabolic changes in women with polycystic ovary syndrome. Arch. Gynecol. Obstet. 281, 35–42 (2010)
A. Kriplani, A.J. Periyasamy, N. Agarwal, V. Kulshrestha, A. Kumar, A.C. Ammini, Effect of oral contraceptive containing ethinyl estradiol combined with drospirenone vs. desogestrel on clinical and biochemical parameters in patients with polycystic ovary syndrome. Contraception 82, 139–146 (2010)
C. Fux Otta, M. Wior, G.S. Iraci, R. Kaplan, D. Torres, M.I. Gaido, E.P. Wyse, Clinical, metabolic, and endocrine parameters in response to metformin and lifestyle intervention in women with polycystic ovary syndrome: A randomized, double-blind, and placebo control trial. Gynecol. Endocrinol. 26, 173–178 (2010)
S.M. Bhattacharya, A. Jha, Comparative study of the therapeutic effects of oral contraceptive pills containing desogestrel, cyproterone acetate, and drospirenone in patients with polycystic ovary syndrome. Fertil. Steril. 98, 1053–1059 (2012)
S. Bonakdaran, Z. Mazloom Khorasani, B. Davachi, J. Mazloom Khorasani, The effects of calcitriol on improvement of insulin resistance, ovulation and comparison with metformin therapy in PCOS patients: a randomized placebo- controlled clinical trial. Iran. J. Reprod. Med. 10, 465–472 (2012)
F. Esfahanian, M.M. Zamani, R. Heshmat, F. Moini nia, Effect of metformin compared with hypocaloric diet on serum C-reactive protein level and insulin resistance in obese and overweight women with polycystic ovary syndrome. J. Obstet. Gynaecol. Res. 39, 806–813 (2012)
D.D. Curi, A.M. Fonseca, J.A. Marcondes, J.A. Almeida, V.R. Bagnoli, J.M. Soares Jr, E.C. Baracat, Metformin versus lifestyle changes in treating women with polycystic ovary syndrome. Gynecol. Endocrinol. 28, 182–185 (2012)
M. Amiri, M. Golsorkhtabaramiri, S. Esmaeilzadeh, F. Ghofrani, A. Bijani, L. Ghorbani et al. Effect of metformin and flutamide on anthropometric indices and laboratory tests in obese/overweight PCOS women under hypocaloric diet. J. Reprod. Infertil. 15, 205–213 (2014)
I. Almenning, A. Rieber-Mohn, K.M. Lundgren, T. Shetelig Løvvik, K.K. Garnæs, T. Moholdt, Effects of high intensity interval training and strength training on metabolic, cardiovascular and hormonal outcomes in women with polycystic ovary syndrome: a pilot study. PLoS ONE 10, 1–16 (2015)
W. Feng, Y.Y. Jia, D.Y. Zhang, H.R. Shi, Management of polycystic ovarian syndrome with Diane-35 or Diane-35 plus metformin. Gynecol. Endocrinol. 32, 147–150 (2016)
Q.Y. Wang, Y. Song, W. Huang, L. Xiao, Q.S. Wang, G.M. Feng, Comparison of drospirenone- with cyproterone acetate-containing oral contraceptives, combined with metformin and lifestyle modifications in women with polycystic ovary syndrome and metabolic disorders: a prospective randomized control trial. Chin. Med. J. (Engl.). 129, 883–890 (2016)
J. Song, X. Ruan, M. Gu, L. Wang, H. Wang, A.O. Mueck, Effect of orlistat or metformin in overweight and obese polycystic ovary syndrome patients with insulin resistance. Gynecol. Endocrinol. 34, 413–417 (2017)
M. Jové, I. Pradas, A. Naudí, S. Rovira-Llopis, C. Bañuls, M. Rocha, M. Portero-Otin, A. Hernández-Mijares, V.M. Victor, R. Pamplona, Lipidomics reveals altered biosynthetic pathways of glycerophospholipids and cell signaling as biomarkers of the polycystic ovary syndrome. Oncotarget 9, 4522–4536 (2018)
C.J. Glueck, R. Papanna, P. Wang, N. Goldenberg, L. Sieve-Smith, Incidence and treatment of metabolic syndrome in newly referred women with confirmed polycystic ovarian syndrome. Metabolism 52, 908–915 (2003)
R. De Pirro, F. Forte, A. Bertoli, A.V. Greco, R. Lauro, Changes in insulin receptors during oral contraception. J. Clin. Endocrinol. Metab. 52, 29–33 (1981)
I.F. Godsland, C. Walton, C. Felton, A. Proudler, A. Patel, V. Wynn, Insulin resistance, secretion, and metabolism in users of oral contraceptives. J. Clin. Endocrinol. Metab. 74, 64–70 (1992)
M. Amiri, F. Ramezani Tehrani, F. Nahidi, A. Kabir, F. Azizi, E. Carmina, Effects of oral contraceptives on metabolic profile in women with polycystic ovary syndrome: a meta-analysis comparing products containing cyproterone acetate with third generation progestins. Metabolism 73, 22–35 (2017)
A. Nath, R. Sitruk-Ware, Different cardiovascular effects of progestins according to structure and activity. Climacteric 12, 96–101 (2009)
K.M. Hoeger, L. Kochman, N. Wixom, K. Craig, R.K. Miller, D.S. Guzick, A randomized, 48-week, placebo-controlled trial of intensive lifestyle modification and/or metformin therapy in overweight women with polycystic ovary syndrome: a pilot study. Fertil. Steril. 82, 421–429 (2004)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wang, A., Mo, T., Li, Q. et al. The effectiveness of metformin, oral contraceptives, and lifestyle modification in improving the metabolism of overweight women with polycystic ovary syndrome: a network meta-analysis. Endocrine 64, 220–232 (2019). https://doi.org/10.1007/s12020-019-01860-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-01860-w