Abstract
Modelling the electrical activity of the heart is an important tool for understanding electrical function in various diseases and conduction disorders. Clearly, for model results to be useful, it is necessary to have accurate inputs for the models, in particular the commonly used bidomain model. However, there are only three sets of four experimentally determined conductivity values for cardiac ventricular tissue and these are inconsistent, were measured around 40 years ago, often produce different results in simulations and do not fully represent the three-dimensional anisotropic nature of cardiac tissue. Despite efforts in the intervening years, difficulties associated with making the measurements and also determining the conductivities from the experimental data have not yet been overcome. In this review, we summarise what is known about the conductivity values, as well as progress to date in meeting the challenges associated with both the mathematical modelling and the experimental techniques.

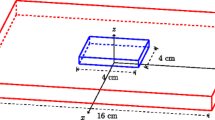
Epicardial potential distributions, arising from a subendocardial ischaemic region, modelled using conductivity data from the indicated studies.







Similar content being viewed by others
References
Arthur RM, Geselowitz DB (1970) Effect of inhomogeneities on the apparent location and magnitude of a cardiac current dipole source. IEEE Trans Biomed Eng 17:141–146
Austin TM, Trew ML, Pullan AJ (2006) Solving the cardiac bidomain equations for discontinuous conductivities. IEEE Trans Biomed Eng 53(7):1265–1272
Barnes JP (2013) Mathematically modeling the electrophysiological effects of ischaemia in the heart. Ph.D. thesis, Griffith University, Brisbane, Australia
Barnes JP, Johnston PR (2012) The effect of ischaemic region shape on epicardial potential distributions in transient models of cardiac tissue. ANZIAM J 53:C110–C126
Barnes JP, Johnston PR (2012) The effect of ischaemic region shape on ST potentials using a half–ellipsoid model of the left ventricle. In: Murray A (ed) Computing in cardiology, vol 39. IEEE Press, IEEE, pp 461–464
Barone A, Fenton F, Veneziani A (2017) Numerical sensitivity analysis of a variational data assimilation procedure for cardiac conductivities. Chaos 27(093):930
Barone A, Gizzi A, Fenton F, Filippi S, Veneziani A (2020) Experimental validation of a variational data assimilation procedure for estimating space-dependent cardiac conductivities. Comput Methods Appl Mech Eng 358(112):615
Barr RC, Plonsey R (2003) Electrode systems for measuring cardiac impedances using optical transmembrane potential sensors and interstitial electrodes — theoretical design. IEEE Trans Biomed Eng 50(8):925–934
Bauer S, Edelmann JC, Seemann G, Sachse FB, Dössel O. (2013) Estimating intracellular conductivity tensors from confocal microscopy of rabbit ventricular tissue. Biomedizinische Technik/Biomedical Engineering 58
Boccia E, Luther S, Parlitz U (2017) Modelling far field pacing for terminating spiral waves pinned to ischaemic heterogeneities in cardiac tissue. Philos Trans Royal Soc A 375(2096):20160,289
Caldwell BJ, Trew ML, Sands GB, Hooks DA, LeGrice IJ, Smaill BH (2009) Three distinct directions of intramural activation reveal nonuniform side–to–side electrical coupling of ventricular myocytes. Circ Arrhythm Electropysiol 2:433–440
Clayton RH, Bernus O, Cherry EM, Dierckx H, Fenton FH, Mirabella L, Panfilov AV, Sachse FB, Seemann G, Zhang H (2011) Models of cardiac tissue electrophysiology: progress, challenges and open questions. Prog Biophys Mol Biol 104(1–3):22–48
Clerc L (1976) Directional differences of impulse spread in trabecular muscle from mammalian heart. J Physiol 255:335–346
Colli Franzone P, Guerri L (1993) Spreading of excitation in 3–D models of the anisotropic cardiac tissue I: validation of the eikonal model. Math Biosci 113:145–209
Colli Franzone P, Guerri L, Taccardi B (1993) Spread of excitation in a myocardial volume: Simulation studies in a model of anisotropic ventricular muscle activated by point stimulation. J Cardiovasc Electrophysiol 4(2):144–160
Colli Franzone P, Guerri L, Taccardi B (2004) Modeling ventricular excitation: axial and orthotropic anisotropy effects on wavefronts and potentials. Math Biosci 188(1–2):191–205
Colli Franzone P, Pavarino LF, Scacchi S (2007) Dynamical effects of myocardial ischemia in anisotropic cardiac models in three dimensions. Math Models Methods Appl Sci 17(12):1965–2008
Coltart DJ, Meldrum SJ (1970) A comparison of the transmembrane action potential of the human and canine myocardium. Cardiology 55:340–350
Costa CM, Hoetzl E, Rocha BM, Prassl AJ, Plank G (2013) Automatic parametrization strategy for cardiac electrophysiology simulations. In: Computing in cardiology, vol 40, pp 373–376
Coudiere Y, Davidovic A, Poignard C (2014) The modified bidomain model with periodic diffusive inclusions. In: Murray A (ed) Computing in cardiology, vol 41, pp 1033–1036
Edwards AG, Louch WE (2017) Species-dependent mechanisms of cardiac arrythmia: a cellular focus. Clin Med Insights Cardiol 11:1179546816686,061
Foster KR, Schwan HP (1989) Dielectic properties of tissue and biological materials: a critical review. Crit Rev Biomed Eng 17(1):25–104
Gielen FL, Wallinga-de Jonge W, Boon KL (1984) Electrical conductivity of skeletal muscle tissue: experimental results from different muscles in vivo. Med Biol Eng Comput 22:569–577
Gokhale TA, Medvescek E, Henriquez CS (2017) Modeling dynamics in diseased cardiac tissue: impact of model choice. Chaos 27:093,909
Graham LS, Kilpatrick D (2010) Estimation of the Bidomain conductivity parameters of cardiac tissue from extracellular potential distributions initiated by point stimulation. Ann Biomed Eng 38(12):3630–3648
Greiner J, Sankarankutty AC, Seemann G, Seidel T, Sachse FB (2018) Confocal microscopy-based estimaton of parameters for computational modeling of electrical conduction in the normal and infarcted heart. Front Physiol 9(239):1–15
Gulrajani RM (1998) Bioelectricity and biomagnetism. (John) Wiley and Sons, New York
Hand P, Griffith B, Peskin C (2009) Deriving macroscopic myocardial conductivities by homogenization of microscopic models. Bull Math Biol 71(7):1707–1726
Henriquez CS (2014) A brief history of tissue models for cardiac electrophysiology. IEEE Trans Biomed Eng 61(5):1457–1465
Hooks D (2007) Myocardial segment-specific model generation for simulating the electrical action of the heart. BioMed Eng OnLine 6(1):21–21
Hooks DA, Tomlinson KA, Marsden SG, LeGrice IJ, Smaill BH, Pullan AJ, Hunter PJ (2002) Cardiac microstructure: Implications for electrical propagation and defibrillation in the heart. Circ Res 91(4):331–338
Hooks DA, Trew ML, Caldwell BJ, Sands GB, LeGrice IJ, Smaill BH (2007) Laminar arrangement of ventricular myocytes influences electrical behavior of the heart. Circ Res 101(10):e103–112–e103–112
Hopenfeld B, Stinstra JG, MacLeod RS (2004) Mechanism for ST depression associated with contiguous subendocardial ischaemia. J Cardiovasc Electrophysiol 15:1200–1206
Hopenfeld B, Stinstra JG, MacLeod RS (2005) The effect of conductivity on ST-segment epicardial potentials arising from subendocardial ischemia. Ann Biomed Eng 33(6):751–763
Huang Q, Eason JC, Claydon FJ (1999) Membrane polarization induced in the myocardium by defibrillation fields: an idealized 3-d finite element bidomain/monodomain torso model. IEEE Trans Biomed Eng 46(1):26–34
Janse MJ, Opthof T, Kléber AG (1998) Animal models of cardiac arrhythmias. Cardiovasc Res 39:165–177
Johnston BM (2013) Design of a multi–electrode array to measure cardiac conductivities. ANZIAM J 54:C271–C290
Johnston BM (2013) Using a sensitivity study to facilitate the design of a multi–electrode array to measure six cardiac conductivity values. Math Biosci 244:40–46
Johnston BM (2016) Six conductivity values to use in the bidomain model of cardiac tissue. IEEE Trans Biomed Eng 63(7):1525–1531
Johnston BM, Barnes JP (2014) Exploiting GPUs to investigate an inversion method that retrieves cardiac conductivities from potential measurements. ANZIAM J 55:C17–C31
Johnston BM, Barnes JP, Johnston PR, Murray A (2016) The effect of conductivity values on activation times and defibrillation thresholds. In: Computing in cardiology, vol 43, pp 161–164
Johnston BM, Coveney S, Chang ETY, Johnston PR, Clayton RH (2018) Quantifying the effect of uncertainty in input parameters in a simplified bidomain model of partial thickness ischaemia. Med Biol Eng Comput 56:761–780
Johnston BM, Johnston PR (2013) A multi-electrode array and inversion technique for retrieving six conductivities from heart potential measurements. Med Biol Eng Comput 51(12):1295–1303
Johnston BM, Johnston PR (2013) The sensitivity of the passive bidomain equation to variations in six conductivity values. In: Boccaccini A (ed) Proceedings of the IASTED international conference biomedical engineering (BioMed 2013). IASTED, ACTA Press, Calgary, pp 538–545
Johnston BM, Johnston PR (2014) How accurately can cardiac conductivity values be determined from heart potential measurements?. In: Murray A (ed) Computing in cardiology, vol 41. IEEE, pp 533–536
Johnston BM, Johnston PR (2015) Determining six cardiac conductivities from realistically large datasets. Math Biosci 266:15–22
Johnston BM, Johnston PR (2018) Determining the most significant input parameters in models of subendocardial ischaemia and their effect on ST segment epicardial potential distributions. Comput Biol Med 95:75–89
Johnston BM, Johnston PR (2018) Sensitivity analysis of ST-segment epicardial potentials arising from changes in ischaemic region conductivities in early and late stage ischaemia. Comput Biol Med 102:288–299
Johnston BM, Johnston PR (2019) Differences between models of partial thickness ischaemia and subendocardial ischaemia in terms of sensitivity analyses of ST-segment epcicardial potential distributions. Math Biosci 318:108,273
Johnston BM, Johnston PR, Kilpatrick D (2006) Analysis of electrode configurations for measuring cardiac tissue conductivities and fibre rotation. Ann Biomed Eng 34(6):986–996
Johnston BM, Johnston PR, Kilpatrick D (2006) A new approach to the determinination of cardiac potential distributions: application to the analysis of electrode configurations. Math Biosci 202(2):288–309
Johnston BM, Narayan A, Johnston PR (2020) A comparison of methods for examining the effect of uncertainty in the conductivities in a model of partial thickness ischaemia. In: Pickett C (ed) Computing in cardiology, vol 46, pp 1–4
Johnston PR (2005) The effect of simplifying assumptions in the bidomain model of cardiac tissue: application to ST-segment shifts during partial ischaemia. Math Biosci 198(1):97–118
Johnston PR (2010) A finite volume method solution for the bidomain equations and their application to modelling cardiac ischaemia. Comput Methods Biomech Biomed Eng 13(2):157–170
Johnston PR (2011) Cardiac conductivity values — a challenge for experimentalists? Noninvasive Functional Source Imaging of the Brain and Heart & 2011 8th International Conference on Bioelectromagnetism (NFSI & ICBEM), 39–43
Johnston PR (2011) A non-dimensional formulation of the passive bidomain equation. J Electrocardiol 44(2):184–188
Johnston PR (2011) A sensitivity study of conductivity values in the passive bidomain equation. Math Biosci 232(2):142–150
Johnston PR, Kilpatrick D (2003) The effect of conductivity values on ST segment shift in subendocardial ischaemia. IEEE Trans Biomed Eng 50(2):150–158
Johnston PR, Kilpatrick D, Li CY (2001) The importance of anisotropy in modelling ST segment shift in subendocardial ischaemia. IEEE Trans Biomed Eng 48(12):1366–1376
Keller DUJ, Webster FM, Seemann G, Dössel O. (2010) Ranking the influence of tissue conductivities on forward-calculated ECGs. IEEE Trans Biomedial Eng 57(7):1568–1576
Kleber AG, Riegger CB (1987) Electrical constants of arterially perfused rabbit papillary muscle. J Physiol 385:307–324
Krassowska W, Neu JC (1992) Theoretical versus experimental estimates of the effective conductivities of cardiac muscle. In: Computers in cardiology 1992, IEEE, pp 703–706
Kwon H, Guasch M, Nagy JA, Rutkove SB, Sanchez B (2019) New electrical impedance methods for the in situ measurement of the complex permittivity of anisotropic skeletal muscle using multipolar needles. Sci Rept 9:3145
Kwon H, Nagy JA, Taylor R, Rutkove SB, Sanchez B (2017) New electrical impedance methods for the in situ measurement of the complex permittivity of anisotropic biological tissues. Phys Med Biol 62:8616–8633
Le Guyader P, Savard P, Trelles F (1995) Measurement of myocardial conductivities with an eight–electrode technique in the frequency domain. 17th IEEE-EMBS, 71–72
Le Guyader P, Savard P, Trelles F (1997) Measurement of myocardial conductivities with a four–electrode technique in the frequency domain. In: Proceedings of 19th international conference, IEEE/EMBS, pp 2448–2449
Le Guyader P, Trelles F, Savard P (2001) Extracellular measurement of anisotropic bidomain myocardial conductivities. I. theoretical analysis. Ann Biomed Eng 29:862–877
LeGrice IJ, Hunter PJ, Smail BH (1997) Laminar structure of the heart: a mathematical model. Am J Physiol 272:H2466–H2476
LeGrice IJ, Smaill BH, Chai LZ, Edgar SG, Gavin JB, Hunter PJ (1995) Laminar structure of the heart: ventricular myocyte arrangement and connective tissue architecture in the dog. Am J Physiol 269:H571–H582
Li Q (2005) Transmyocardial ST potential distributions in ischaemic heart disease. Ph.D. thesis, University of Tasmania
Lombaert H, Peyrat J, Croisille P, Rapacchi S, Fanton L, Cheriet F, Clarysse P, Magnin I, Delingette H, Ayache N (2012) Human atlas of the cardiac fiber architecture: study on a healthy population. IEEE Trans Med Imaging 31(7):1436–1447
MacLachlan MC, Sundnes J, Lines GT (2005) Simulation of ST segment changes during subendocardial ischemia using a realistic 3-D cardiac geometry. IEEE Trans Biomed Eng 52(5):799–807
van Oosterom A, de Boer RW, Dam RTV (1979) Intramural resistivity of cardiac tissue. Med & Biol Eng & Comput 17:337–343
Plonsey R, Barr RC (1982) The four-electrode resistivity technique as applied to cardiac muscle. IEEE Trans Biomed Eng 29(7):541–546
Plourde E, Savard P, Le Guyader P (2000) Electrical alignment of a cardiac impedance probe. In: Computers in cardiology, vol 27, IEEE, IEEE Press, pp 773-775
Pollard AE, Barr RC (2006) Cardiac micro–impedance measurement in two–dimensional models using multisite interstitial stimulation. Am J Physiol-Heart Circ Physiol 290(5):H1976–H1987
Pollard AE, Barr RC (2010) A biophysical model for cardiac microimpedance measurements. Am J Physiol-Heart Circ Physiol 298:H1699–H1709
Pollard AE, Barr RC (2013) A new approach for resolution of complex tissue impedance spectra in hearts. IEEE Trans Biomed Eng 60(9):2494–2503
Pollard AE, Barr RC (2014) A structural framework for interpretation of four-electrode microimpedance spectra in cardiac tissue. In: Conference proceedings of IEEE engineering in medicine and biology society, pp 6467–6470
Pollard AE, Ellis CD, Smith WM (2008) Linear electrode arrays for stimulation and recording within cardiac tissue space constants. IEEE Trans Biomed Eng 55(4):1408–1414
Pollard AE, Hooke N, Henriquez CS (1992) Cardiac propagation simulation. Crit Rev Biomed Eng 20:171–210
Pollard AE, Smith WM, Barr RC (2004) Feasibility of cardiac microimpedance measurement using multisite interstitial stimulation. Am J Physiol Circ Physiol 287:H2402–H2411
Pormann JB (1999) A simulation system for the bidomain equations. Ph.D thesis, Duke University, Durham NC
Potse M, Coronel R, Falcao S, LeBlanc AR, Vinet A (2007) The effect of lesion size and tissue remodeling on ST deviation in partial-thickness ischemia. Heart Rhythm 4(2):200–206
Potse M, LeBlanc AR, Cardinal R, Vinet A (2006) ST elevation or depression in subendocardial ischemia?. In: 28Th IEEE EMBS annual international conference, pp 3899–3902
Roberts DE, Hersh LT, Scher AM (1979) Influence of cardiac fiber orientation on wavefront voltage, conduction velocity and tissue resistivity in the dog. Circ Res 44:701–712
Roberts DE, Scher AM (1982) Effects of tissue anisotropy on extracellular potential fields in canine myocardium in situ. Circ Res 50:342–351
Roth BJ (1988) The electrical potential produced by a strand of cardiac muscle: a bidomain analysis. Ann Biomed Eng 16:609–637
Roth BJ (1997) Electrical conductivity values used with the bidomain model of cardiac tissue. IEEE Trans Biomed Eng 44(4):326–328
Roth BJ (1997) Nonsustained reentry following successive stimulation of cardiac tissue through a unipolar electrode. J Cardiovasc Electrophysiol 8:768–778
Rush S, Abildskov JA, McFee R (1963) Resistivity of body tissues at low frequencies. Circ Res 12:40–50
Sachse FB, Moreno A, Seemann G, Abildskov J (2009) A model of electrical conduction in cardiac tissue including fibroblasts. Ann Biomed Eng 37:874–889
Sadleir R, Henriquez C (2006) Estimation of cardiac bidomain parameters from extracellular measurement: Two dimensional study. Ann Biomed Eng 34(8):1289–1303
Sanchez C, D’Ambrosio G, Maffessanti F, Caiani EG, Prinzen FW, Krause R, A A, Potse M (2018) Sensitivity analysis of ventricular activation and eletrocardiogram in tailored models of heart-failure patients. Med Biol Eng Comput 56:491–504
Schmitt OH (1969) Biological information processing using the concept of interpenetrating domains. In: Leibovic KN (ed) Information processing in the nervous system. chap. 18. Springer–Verlag, New York, pp 325–331
Schwab BC, Seemann G, Lasher R, Torres N, Wulfers E, Arp M, Carruth E, Bridge J, Sachse F (2013) Quantitative analysis of cardiac tissue including fibroblasts using three-dimensional confocal microscopy and image reconstruction: towards a basis for electrophysiological modeling. IEEE Trans Med Imaging 32(5):862–872
Shome S, Stinstra JG, Hopenfeld B, Punske BB, MacLeod RS (2004) A study of the dynamics of cardiac ischaemia using experimental and modeling approaches. In: Proceedings of the IEEE engineering in medicine and biology 26th annual international conference. 3585-3588, IEEE EMBS, IEEE Press
Shor NZ (1985) Minimization methods for Non-Differentiable Functions, Springer Series in Computational Mathematics, vol. 3 Springer–Verlag
Smith W, Fleet W, Johnson F, Engle T, Cascio C (1995) The ib phase of ventricular arrhythmias in ischemic in situ porcine heart is related to changes in cell-to-cell electrical coupling. Circulation 92:3051–3060
Steendijk P, Mur G, van der Velde ET, Baan J (1993) The four-electrode resistivity technique in anisotropic media: Theoretical analysis and application on myocardial tissue in Vivo. IEEE Trans Biomed Eng 40(11):1138–1147
Stinstra J, Hopenfeld B, MacLeod R (2005) On the passive cardiac conductivity. Ann Biomed Eng 33(12):1743–1751
Stinstra JG, Hopenfeld B, MacLeod R (2003) A model for the passive cardiac conductivity. Int J Biolectromagnetism 5(1):185–186
Streeter D Jr, Spotnitz H, Patel D, Ross J Jr, Sonnenblick E (1969) Fiber orientation in the canine left ventricle during diastole and systole. Circ Res 24:339–347
Tikhonov AN, Arsenin VY (1977) Solutions of ill-posed problems. V.H. Winston and Sons Washington
Trayanova N, Eason J, Aguel F (2002) Computer simulations of cardiac defibrillation: a look inside the heart. Comput Vis Sci 4:259–270
Trew ML, Caldwell BJ, Gamage TPB, Sands GB, Smaill BH (2008) Experiment-specific models of ventricular electrical activation: construction and application. In: 30Th annual international IEEE EMBS conference, pp 137–140
Tung L (1978) A bi–domain model for describing ischaemic myocardial D-C potentials. Ph.D. thesis, Massachusetts Institute of Technology
Varro A, Lathrop DA, Hester SB, Nanasi PP, Papp JGY (1193) Ionic currents and action potential in rabbit, rat and guinea pig ventricular myocytes. Basic Res Cardiol 88(2):93–102
Waits CMK, Barr RC, Pollard AE (2014) Sensor spacing affects the tissue impedance spectra of rabbit ventricular epicardium. Am J Physiol Heart Circ Physiol 306(12):H1660–H1668
Weidmann S (1970) Electrical constants of trabecular muscle from mammalian heart. J Physiol 210:1041–1054
Yang H, Veneziani A (2015) Estimation of cardiac conductivities in ventricular tissue by a variational approach. Inverse Probl 31(115):001
Yang H, Veneziani A (2017) Efficient estimation of cardiac conductvities via POD-DIEM model order reduction. Appl Numer Math 115:180–199
Funding
We acknowledge funding from the National Institute of Health, Bethesda, USA (R03EB029625).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Johnston, B.M., Johnston, P.R. Approaches for determining cardiac bidomain conductivity values: progress and challenges. Med Biol Eng Comput 58, 2919–2935 (2020). https://doi.org/10.1007/s11517-020-02272-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-020-02272-z